This article was co-authored by Shaun Berger, MD. Dr. Shaun Berger is a board certified Pediatrician based in the San Diego, California metro area. Dr. Berger provides comprehensive primary care for newborns, children, and adolescents, focusing on preventive medicine. Dr. Berger earned a BA in Psychology from the University of California, San Diego and an MD from the University of Illinois at Chicago. Dr. Berger then completed a residency at the UCSF/Fresno Community Medical Centers/Valley Children’s Hospital where he was elected Chief Resident. He has been awarded the UCSF Foundation Award and is a Fellow of the American Academy of Pediatrics.
There are 31 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 65,570 times.
Asthma is a treatable disease that works like an allergic reaction: environmental triggers cause inflammation in the airways. This leads to trouble breathing until the inflammation is treated and reduced. The disease is very common and affects about 334 million people worldwide, including 25 million in the US alone.[1] If you suspect you might have asthma, there are signs and symptoms, risk factors, and diagnostic tests that can help you know for sure.
Steps
Knowing the Risk Factors for Asthma
-
1Take the combination of gender and age into consideration. In the US, boys under 18 years have a 54% higher rate of asthma than girls. But by 20, female asthma sufferers outnumber the males. After 35 this gap grows, with 10.1% of women having asthma compared to 5.6% of men. After menopause the rate decreases for females, and the gap narrows but does not completely disappear.[2] Experts have a few theories on why gender and age seem to affect asthma risk:
- Increased atopy (a predisposition to allergic sensitivity) in male adolescents.
- Smaller airway size in male adolescents compared to females.[3]
- Sex hormone fluctuations during premenstrual, menstrual, and menopausal years in women.
- Studies that re-introduced hormones for menopausal women had an increase in newly diagnosed asthma.
-
2Look for a family history of asthma. Experts have found more than 100 genes that associated with asthma and allergies. Research done on families — especially twins — suggests that asthma is caused by a shared hereditary factor. A 2009 study found that family history was actually the strongest predictor of whether someone will develop asthma. If comparing families with normal, moderate, and high genetic risk for asthma, moderate risk subjects were 2.4 times more likely to develop asthma, and high risk subjects 4.8 times more likely.[4]
- Ask your parents and other relatives if there is a history of asthma in your family.
- If you are adopted, your biological parents may have provided a family history to your adoptive family.
Advertisement -
3Take note of any allergies. Research has linked an immune protein antibody called "IgE" with the development of asthma. If you have high IgE levels, you're also more likely to inherit a predisposition to developing allergies.[5] When there's IgE in the blood, the body experiences an inflammatory allergic reaction that causes airway constriction, rashes, itchiness, watery eyes, wheezing, etc.
- Note an allergic reaction you may have to common triggers, including food, roaches, animals, mold, pollen and dust mites.[6]
- If you have allergies, you also have an increased risk of developing asthma.
- If you experience severe allergic reactions but can't identify the trigger, ask your doctor for allergy testing. He or she will expose small patches of your skin to different types of allergens to look for allergic changes.
-
4Avoid exposure to tobacco smoke. When we inhale particles into our lungs, the body's reaction is to cough it out. These particles can also trigger an inflammatory response and asthma symptoms. The more exposure you get to tobacco smoke, the greater risk you have of developing asthma. If you're addicted to smoking, talk to your healthcare professional about strategies and medications you can use to quit. Common strategies include using nicotine gum and patches, gradually decreasing cigarette use, or taking medications like Chantix or Wellbutrin.[7] Even if you're having trouble quitting, make sure not to smoke around other people. Consistent exposure to second-hand smoke can cause asthma to develop in those around you.
- Smoking while pregnant causes childhood wheezing, increased risk of food allergies, and inflammatory proteins in the blood. The effect is even greater if the child continues to be exposed to second-hand smoke after birth.[8] Talk to your OBGYN before taking any oral medication to help you stop smoking.
-
5Lower your stress levels. Many studies have shown that high levels of stress hormones can lead to the onset of asthma symptoms, increased allergen sensitivity, and lung constriction.[9] Try to identify the things that cause the most stress in your life, and work toward removing those stressors.
- Try relaxation techniques such as deep breathing, meditation, and yoga.
- Exercise regularly to release endorphins that ease pain and reduce stress levels.
- Improve your sleeping habits: go to sleep when you're tired, don't sleep with the TV on, don't eat before going to sleep, avoid night time caffeine, and try to maintain same sleep schedule daily.[10]
-
6Stay away from the air pollution in your environment. A significant portion of childhood asthma is caused by exposure to air pollution from factories, construction, vehicles, and industrial plants. Just as tobacco smoke irritates the lungs, air pollution triggers inflammatory reactions that lead to lung damage and constriction. While you can't eliminate air pollution, you can reduce your exposure.[11]
- Avoid breathing the air around major streets or highways when possible.
- Have children play outside in areas far away from highways or construction.
- If relocation is an option, see the EPA's air quality index guidelines to find the areas with the best air quality.[12]
-
7Take your medications into consideration. If you are taking certain medications, note if you've been having more asthma symptoms since you began taking them. If so, consult your doctor before stopping, reducing dosage for, or changing medications.
- Studies show that aspirin and ibuprofen can cause lung and airway constriction in asthmatic patients sensitive to them.[13]
- ACE inhibitors used to treat blood pressure don't cause asthma, but cause a dry cough that can be mistaken for it. However, excessive coughing from ACE inhibitors can irritate your lungs and trigger the onset of asthma. Common ACE inhibitors include ramipril and perindopril.
- Beta blockers are used to treat heart problems, high blood pressure, and migraines. They can constrict your lung airways.[14] Some doctors may prescribe beta blockers even if you have asthma, and just keep an eye on you for changes. Common beta blockers include metoprolol and propanolol.
-
8Maintain a healthy weight.[15] Many studies have found a link between increased weight and increased risk of asthma. The extra weight makes it harder to breathe and pump blood throughout your body. It also increases the number of inflammatory proteins (cytokines) in the body, making you more likely to experience airway inflammation and constriction.
Recognizing Mild and Moderate Signs and Symptoms
-
1See a doctor even for mild symptoms. Early symptoms aren't serious enough to interfere with your normal activities or daily life.[16] When the condition starts to progress, though, you'll notice yourself having trouble with normal activities. People usually continue to experience the early symptoms, but more severely.
- If left undiagnosed or untreated, the early, mild symptoms of asthma can get progressively worse. This is especially true if you don't identify your triggers and avoid them.
-
2Notice excessive coughing. If you have asthma, your airways can get closed off because of the constriction or inflammation from the disease. Your body will respond by trying to clear your airways through coughing. While the coughs you get during a bacterial infection are wet, mucus-y coughs, asthma coughs tend to be dry, with very little mucus.[17]
- If coughing begins or worsens at night, it may be asthma. A common symptom of asthma is nighttime coughing, or coughing that gets worse right after you wake up.[18]
- In more progressed cases, coughing extends into the day.
-
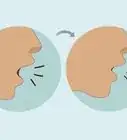
3Listen for noise when you exhale. Asthmatics often notice a wheezing or high-pitched whistling when they exhale. This is caused by the constriction of airways.[19] Note when you hear the sound. If it's at the very end of exhalation, it's an early sign of mild asthma. But as the condition progresses from mild to moderate symptoms, you’ll wheeze or whistle throughout the entire exhalation.
-
4Take note of unusual shortness of breath. "Exercise-induced bronchoconstriction" is a type of asthma seen in those who've just done something strenuous, like exercising.[20] The airway constriction will leave you tired and gasping for air sooner than you should be, and you may have to give up the activity before you want to.[21] Compare how long you can normally exercise to instances when fatigue and shortness of breath limit you.
-
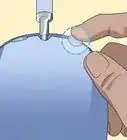
5Be on the watch for rapid breathing.[22] To get more oxygen in the constricted lungs, the body increases its respiration rate. Place your palm over your chest and count how many times your chest rise and falls in one minute. Use a stopwatch or clock with a second hand, so you can time out an accurate minute. A normal respiratory rate is between 12 and 20 breaths in 60 seconds.
- With moderate asthma, your respiratory rate can be from 20 to 30 breaths per minute.
-
6Don't ignore cold or flu symptoms. Though the coughing from asthma is different from that from a cold or flu, bacteria and viruses can trigger asthma. Look for signs of infection that may be causing the asthma symptoms: sneezing, runny nose, sore throat, and congestion.[23] If the coughing dark, green, or white mucus, the infection may be bacterial. If it's clear or white, it may be viral.[24]
- If you see these infection symptoms combined with noise on exhalation and gasping for breath, you likely have asthma triggered by an infection.
- See a doctor to find out exactly what's going on.
Recognizing Severe Symptoms
-
1Seek medical attention if you can't breathe, even without exertion.[25] Normally, the shortness of breath caused by activity in asthmatics gets better with rest. However, when severe symptoms are present or when you're experiencing an asthma attack, breathlessness occurs even when you're resting because of triggers activating the inflammatory process. If the inflammation is serious enough, you will suddenly find yourself severely short of breath or taking deep gasps of air.
- You may also feel like you can't fully exhale. When the body needs the oxygen from inhalation, it shortens exhalation so it can get to oxygen more quickly.
- You may find that you can’t speak in full sentences, but are using short words and sentences between gasps.
-
2Check your respiration rate. Even mild and moderate asthma attacks can make you breathe rapidly, but severe attacks are worse. The constriction in your airways is preventing you bringing enough fresh air into your body, starving it of oxygen. The rapid breathing is your body's attempt to get as much oxygen as possible to correct the situation before it suffers damage.
- Place your palm over your chest and note how many times your chest rises and falls in one minute. Use a stopwatch or clock with a second hand to time out an accurate minute.
- In severe episodes, your respiration rate will be over 30 breaths per minute.
-
3Take your pulse. To get oxygen to your tissues and organs, blood picks up oxygen from the air in your lungs and carries it to different parts of the body. During a severe attack, when there's not enough oxygen being brought in, the heart must pump blood faster to get as much oxygen to tissues and organs as possible. You may feel your heart racing without explanation during severe attacks.
- Hold your hand out, palm up.
- Place the tips of the index and middle fingers of your other hand on the outer part of your wrist, below the thumb.
- You will feel a rapid, beating pulse from the radial artery.
- Calculate your heart rate by counting how many times your heart beats in one minute. A normal heart rate is less than 100 beats per minute, but in severe asthma symptoms you may get rates over 120.[26]
- Some smart phones now have heartbeat monitors built right in. If yours does, you can use that.
-
4Look for a bluish tinge to your skin. Blood is only bright red when it's carrying oxygen — otherwise it's much darker. Whenever we see it, it's hit the open air outside of our bodies and turned bright with oxygen, so we're not used to thinking of it any other way. But during a severe asthma attack, you may experience "cyanosis" caused by dark, oxygen-starved blood traveling through your arteries.[27] This causes the skin to appear bluish or grayish, especially on the lips, fingers, nails, gums, or the thin skin around the eyes.[28]
-
5See if you're tensing your neck and chest muscles.[29] When we breathe heavily or are in respiratory distress, we engage accessory (not usually central to breathing) muscles. The muscles we bring into the breathing process in these situations are on the sides of the neck: the sternocleidomastoid and scalene muscles. Look for deep outlines in the neck muscles if you're having trouble breathing. Furthermore, the muscles between our ribs (the intercostals) get pulled inward. These muscles help lift the rib cage during inhalation, and may be able to see this retraction between your ribs in serious conditions.
- Look in the mirror to see both the deeply outlined neck muscles and the retracted muscles between your ribs.
-
6Check for chest tightness or pain. When you're working too hard to breathe, the muscles involved with respiration get overworked. This results in muscle fatigue in the chest, which feels like tightness and pain. The pain might feel dull, sharp, or stabbing, and can around the middle of the chest (sternal) or slightly off center (parasternal). This requires immediate medical attention and a visit to the emergency room to rule out heart issues.
-
7Listen for worsening noise during respiration.[30] In mild and moderate symptoms, the whistling and wheezing is only heard on exhalation. However, in severe episodes, you can hear it both on exhalation and inhalation. The whistling noise we hear on inhalation is known as "stridor," and is caused by constriction of the throat muscles in the upper respiratory tract. Wheezing tends to occur on exhalation, and is caused by constriction of muscles in the lower respiratory tract.
- Noise on inhalation can be a symptom both of asthma and of severe allergic reaction. You need to be able to distinguish between them so you can treat the cause appropriately.
- Look for hives or red rashes on the chest, which indicate an allergic reaction instead of an asthma attack. Swelling of the lips or tongue also point to allergies.
-
8Treat asthma symptoms as soon as possible. If you have a severe attack that makes it hard to breathe, call 911 and get to an emergency room immediately. If you're undiagnosed, you likely don't have a rescue inhaler. If you have one, though, use it.
- Albuterol inhaler pumps should only be used 4 times a day, but in an attack it's ok to use it as often as every 20 minutes for 2 hours.[31]
- Take slow deep breaths, counting to 3 in your head on inhalation and exhalation. This can help reduce stress and your breathing rate.
- Remove the trigger if you can identify it.
- Asthma will get better when you use steroids prescribed by your physician. These drugs can be inhaled through a pump or taken as a tablet. Take a puff of the medication or a tablet with water. It takes a few hours to start working, but will control asthma symptoms.
-
9Seek emergency attention for severe asthma symptoms.[32] These symptoms suggest you're having an acute attack, and your body is struggling to draw enough air to function. This is considered a medical emergency that could prove potentially fatal if not treated immediately.
Getting Diagnosed
-
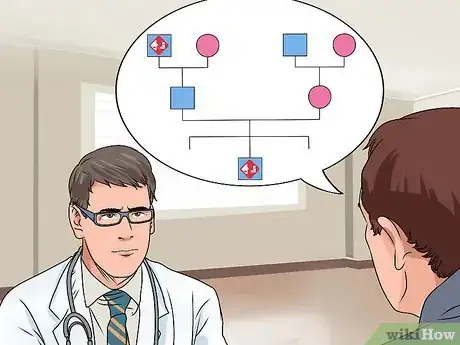
1Provide your doctor with your medical history. The information you give should be as accurate as possible. This will allow the doctor to get an overall picture about the issues affecting you. Prepare the information beforehand so you don't have to think of it off the top of your head at the doctor's office:
- Any signs and symptoms of asthma (coughing, shortness of breath, noises during breathing, etc.)
- Past medical history (previous allergies, etc.)
- Family history (history of lung diseases or allergies with your parents, siblings, etc.)
- Your social history (tobacco use, diet and exercise, environment)
- Any medications you may be on (such as aspirin) and any supplements or vitamins you're taking
-
2Submit to a physical examination.[33] The doctor might examine some or all of the following during your exam: your ears, eyes, nose, throat, skin, chest and lungs during the exam. This may include using the stethoscope on the front and back of your chest to listen for breathing noises or absence of lung sounds.
- Because asthma is related to allergies, he or she will also look for runny nose, red eyes, watery eyes and skin rashes.
- Finally, the doctor will inspect the throat for swelling and your ability to breathe, as well as any abnormal sounds that may indicate constricted airways.
-
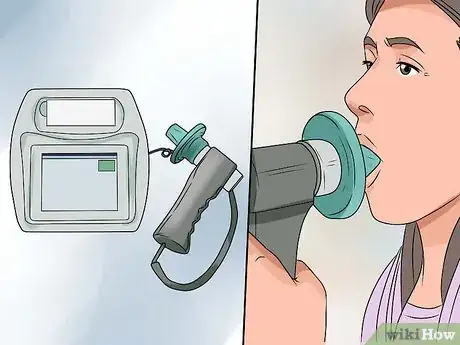
3Allow the doctor to confirm the diagnosis with a spirometry test. During this test, you will breathe into a mouthpiece connected to a spirometer that measures your air flow rate and how much air you can breathe in and out. Take a deep breath and exhale forcefully for as long as possible while the device takes the measurement.[34] While a positive result confirms asthma, a negative result doesn't rule it out.[35]
-
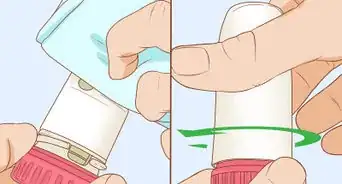
4Do a peak air flow test.[36] This is similar to spirometry, and measures how much air you can exhale. Your doctor or a lung specialist may recommend this test to help confirm the diagnosis. To take the test, place your lips over the opening of the device and set the device to zero. Stand up straight and take a deep breath, then blow as hard and fast as you can in one breath. Repeat this a few times so you can get consistent results. Take the largest of these numbers — this is your peak flow. When you feel asthma symptoms coming on, repeat the test and compare your airflow to your peak flow.[37]
- If your value is over 80% of your best peak flow, you're in a safe range.
- If your value is between 50 and 80% of your best peak flow, your asthma is not being well-managed and your physician will likely adjust medication for you. You're at moderate risk of experiencing an asthma attack if you're in this range.
- If your value is less than 50% of your best peak flow, you're experiencing a severe decrease in breathing function that likely needs to be addressed with medication.
-
5Ask the doctor to do a methacholine challenge test. If you're not presenting with symptoms when you see the doctor, it can be hard for him or her to diagnose you accurately. He or she may recommend a methacholine challenge test. He or she will provide you with an inhaler you'll use to inhale methacholine. The methacholine will cause airway constriction if you have asthma, and trigger symptoms that can be measured with spirometry and peak air flow tests.[38]
-
6Test your response to asthma medication.[39] Sometimes your doctor will forgo these tests and just provide asthma medication to see if you get better. If symptoms reverse, chances are you have asthma. Symptom severity will help your doctor choose what medications to use, but a full history and physical exam will also factor into the decision.
- A common medication is an albuterol/salbutamol inhaler pump, which you use by pursing your lips over the opening and pumping the medication in your lungs while you inhale.
- Bronchodilator medications help open constricted airways by dilating them.
Expert Q&A
-
QuestionWhat are the potential triggers for childhood asthma?
 Shaun Berger, MDDr. Shaun Berger is a board certified Pediatrician based in the San Diego, California metro area. Dr. Berger provides comprehensive primary care for newborns, children, and adolescents, focusing on preventive medicine. Dr. Berger earned a BA in Psychology from the University of California, San Diego and an MD from the University of Illinois at Chicago. Dr. Berger then completed a residency at the UCSF/Fresno Community Medical Centers/Valley Children’s Hospital where he was elected Chief Resident. He has been awarded the UCSF Foundation Award and is a Fellow of the American Academy of Pediatrics.
Shaun Berger, MDDr. Shaun Berger is a board certified Pediatrician based in the San Diego, California metro area. Dr. Berger provides comprehensive primary care for newborns, children, and adolescents, focusing on preventive medicine. Dr. Berger earned a BA in Psychology from the University of California, San Diego and an MD from the University of Illinois at Chicago. Dr. Berger then completed a residency at the UCSF/Fresno Community Medical Centers/Valley Children’s Hospital where he was elected Chief Resident. He has been awarded the UCSF Foundation Award and is a Fellow of the American Academy of Pediatrics.
Board Certified Pediatrician It really depends on the patient and what type of asthma they have. One child may only cough when they have a cold, and their triggers are colds are viruses. Another child may be triggered by pollen that starts blowing in the air every spring. There are children who are triggered by changes in the air temperature or stress. A big trigger for many children is exercise. It really depends on the individual child.
It really depends on the patient and what type of asthma they have. One child may only cough when they have a cold, and their triggers are colds are viruses. Another child may be triggered by pollen that starts blowing in the air every spring. There are children who are triggered by changes in the air temperature or stress. A big trigger for many children is exercise. It really depends on the individual child. -
QuestionIs it okay if my child uses an inhaler but I don't think they have asthma?
 Shaun Berger, MDDr. Shaun Berger is a board certified Pediatrician based in the San Diego, California metro area. Dr. Berger provides comprehensive primary care for newborns, children, and adolescents, focusing on preventive medicine. Dr. Berger earned a BA in Psychology from the University of California, San Diego and an MD from the University of Illinois at Chicago. Dr. Berger then completed a residency at the UCSF/Fresno Community Medical Centers/Valley Children’s Hospital where he was elected Chief Resident. He has been awarded the UCSF Foundation Award and is a Fellow of the American Academy of Pediatrics.
Shaun Berger, MDDr. Shaun Berger is a board certified Pediatrician based in the San Diego, California metro area. Dr. Berger provides comprehensive primary care for newborns, children, and adolescents, focusing on preventive medicine. Dr. Berger earned a BA in Psychology from the University of California, San Diego and an MD from the University of Illinois at Chicago. Dr. Berger then completed a residency at the UCSF/Fresno Community Medical Centers/Valley Children’s Hospital where he was elected Chief Resident. He has been awarded the UCSF Foundation Award and is a Fellow of the American Academy of Pediatrics.
Board Certified Pediatrician There's a classification of asthma symptoms. It's important to start with the premise that you need to control the problem instead of letting the problem control you. There are some children that get diagnosed with asthma that the parents didn't really think they have asthma, but they notice that their child's colds always last longer than everyone else in the family. Or even on another level, they only need to use an inhaler when they're sick, but they don't have asthma. So a lot of times the actual labeling of it is not really the issue; it's more what's going on in the lungs and if the child is going to respond to the inhaler.
There's a classification of asthma symptoms. It's important to start with the premise that you need to control the problem instead of letting the problem control you. There are some children that get diagnosed with asthma that the parents didn't really think they have asthma, but they notice that their child's colds always last longer than everyone else in the family. Or even on another level, they only need to use an inhaler when they're sick, but they don't have asthma. So a lot of times the actual labeling of it is not really the issue; it's more what's going on in the lungs and if the child is going to respond to the inhaler. -
QuestionWhat are things that may induce asthma?
 Shaun Berger, MDDr. Shaun Berger is a board certified Pediatrician based in the San Diego, California metro area. Dr. Berger provides comprehensive primary care for newborns, children, and adolescents, focusing on preventive medicine. Dr. Berger earned a BA in Psychology from the University of California, San Diego and an MD from the University of Illinois at Chicago. Dr. Berger then completed a residency at the UCSF/Fresno Community Medical Centers/Valley Children’s Hospital where he was elected Chief Resident. He has been awarded the UCSF Foundation Award and is a Fellow of the American Academy of Pediatrics.
Shaun Berger, MDDr. Shaun Berger is a board certified Pediatrician based in the San Diego, California metro area. Dr. Berger provides comprehensive primary care for newborns, children, and adolescents, focusing on preventive medicine. Dr. Berger earned a BA in Psychology from the University of California, San Diego and an MD from the University of Illinois at Chicago. Dr. Berger then completed a residency at the UCSF/Fresno Community Medical Centers/Valley Children’s Hospital where he was elected Chief Resident. He has been awarded the UCSF Foundation Award and is a Fellow of the American Academy of Pediatrics.
Board Certified Pediatrician There are many triggers that could bring on asthmatic symptoms, including dust, pet allergies, exercise, and respiratory infections.
There are many triggers that could bring on asthmatic symptoms, including dust, pet allergies, exercise, and respiratory infections.
Warnings
- If you begin experiencing any of these symptoms, see your doctor immediately.⧼thumbs_response⧽
References
- ↑ http://www.nhlbi.nih.gov/health/health-topics/topics/asthma
- ↑ Kynk J, Mastronarde J, McCallister J. Asthma the sex difference. Menopause and hormone replacement therapy. Current opinion in Pulmonary Medicine. 2011;17(1):6-11.
- ↑ http://www.uptodate.com/contents/risk-factors-for-asthma
- ↑ Liu T. The association between family history of asthma and the prevalence of asthma among US adults: National Health and Nutrition Examination Survey, 1999-2004. Genetics in Medicine Journal. 2009 May;11(5):323-8.
- ↑ Subbarao P. et al. Asthma: epidemiology, etiology and risk factors. Canadian Medical Association Journal. 2009 Oct 27; 181(9): E181–E190.
- ↑ Shaun Berger, MD. Board Certified Pediatrician. Expert Interview. 17 April 2020.
- ↑ http://www.cdc.gov/tobacco/campaign/tips/diseases/secondhand-smoke-asthma.html
- ↑ Subbarao P. et al. Asthma: epidemiology, etiology and risk factors. Canadian Medical Association Journal. 2009 Oct 27; 181(9): E181–E190.
- ↑ Chen E, Miller G. Stress and Inflammation in Exacerbations of Asthma. Brain & Behavioral Immunology. 2007 Nov; 21(8): 993–999.
- ↑ http://my.clevelandclinic.org/health/diseases_conditions/hic_Asthma_An_Overview/hic_Understanding_Asthma_Triggers/hic_Stress_and_Asthma
- ↑ http://www.nrdc.org/health/effects/fasthma.asp
- ↑ http://www.epa.gov/airdata/ad_rep_aqi.html
- ↑ http://www.asthma.partners.org/NewFiles/AspirinSensitivity.html
- ↑ https://pubmed.ncbi.nlm.nih.gov/31352857/
- ↑ Delgado J, Barranco P, Quirce S. Obesity and Asthma. Journal of Investigational Allergology, & Clinical Immunology. 2008;18(6):420-5.
- ↑ http://www.nhlbi.nih.gov/health/health-topics/topics/asthma/signs
- ↑ http://www.health.harvard.edu/staying-healthy/that-nagging-cough
- ↑ http://www.nhlbi.nih.gov/health/health-topics/topics/asthma/signs
- ↑ http://my.clevelandclinic.org/health/diseases_conditions/hic_Asthma_An_Overview/hic_Symptoms_of_Asthma
- ↑ Shaun Berger, MD. Board Certified Pediatrician. Expert Interview. 17 April 2020.
- ↑ http://emedicine.medscape.com/article/296301-clinical
- ↑ http://www.aafp.org/afp/2013/0715/p130.html
- ↑ Shaun Berger, MD. Board Certified Pediatrician. Expert Interview. 17 April 2020.
- ↑ http://my.clevelandclinic.org/health/diseases_conditions/hic_Asthma_An_Overview/hic_Symptoms_of_Asthma
- ↑ http://www.nlm.nih.gov/medlineplus/ency/article/000141.htm
- ↑ http://emedicine.medscape.com/article/296301-clinical
- ↑ http://my.clevelandclinic.org/health/diseases_conditions/hic_Asthma_An_Overview/hic_Symptoms_of_Asthma
- ↑ http://www.nlm.nih.gov/medlineplus/ency/article/007198.htm
- ↑ Nurse's Five-minute Clinical Consult: Signs and Symptoms. Lippincott Williams & Wilkins. 2008.
- ↑ http://my.clevelandclinic.org/health/diseases_conditions/hic_Asthma_An_Overview/hic_Symptoms_of_Asthma
- ↑ http://www.asthma.partners.org/NewFiles/Lesson7.html
- ↑ http://www.nlm.nih.gov/medlineplus/ency/article/000141.htm
- ↑ http://www.mayoclinic.org/diseases-conditions/asthma/basics/tests-diagnosis/con-20026992
- ↑ https://www.aafa.org/using-spirometry-diagnose-asthma/
- ↑ BARREIRO T, PERILLO I. An Approach to Interpreting Spirometry. American family Physician Journal. 2004 Mar 1;69(5):1107-1115.
- ↑ http://www.mayoclinic.org/diseases-conditions/asthma/basics/tests-diagnosis/con-20026992
- ↑ http://www.asthma.partners.org/NewFiles/PeakFlow.html
- ↑ https://www.aafa.org/asthma/asthma-diagnosis/lung-function-tests/provocation-trigger-tests.aspx
- ↑ https://ginasthma.org/wp-content/uploads/2019/06/GINA-2019-main-report-June-2019-wms.pdf
About This Article
To know if you have asthma, look out for excessive dry coughing, which often begins soon after you wake up. Additionally, listen for a wheezing or high-pitched whistling noise when you exhale. You should also take note of any abnormal shortness of breath when you're performing activities, like exercise. If you notice your skin turning a blueish grey color or you're struggling to breathe even when resting, seek medical attention as these can be signs of a severe asthma attack. For tips on how to get an asthma diagnosis from a doctor, read on!








































































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...