This article was co-authored by Shaun Berger, MD and by wikiHow staff writer, Jessica Gibson. Dr. Shaun Berger is a board certified Pediatrician based in the San Diego, California metro area. Dr. Berger provides comprehensive primary care for newborns, children, and adolescents, focusing on preventive medicine. Dr. Berger earned a BA in Psychology from the University of California, San Diego and an MD from the University of Illinois at Chicago. Dr. Berger then completed a residency at the UCSF/Fresno Community Medical Centers/Valley Children’s Hospital where he was elected Chief Resident. He has been awarded the UCSF Foundation Award and is a Fellow of the American Academy of Pediatrics.
There are 16 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 103,418 times.
Many people are familiar with common asthma symptoms like tightness in the chest and difficulty breathing. Coughing is another troublesome symptom of asthma, the inflammatory lung disease which narrows the breathing airways. To stop an asthma-related cough, identify and avoid your triggers, take medication to treat your asthma, and make yourself comfortable.
Steps
Identifying Your Asthma Triggers
-
1Learn about common triggers. Coughing can be triggered by a variety of substances like allergens (dust, animal fur, cockroaches, mold, and pollens) and irritants (like chemicals in the air, cigarette smoke, air pollution, and beauty products). Other common asthma triggers include:[1]
- Medications: these may include aspirin, other nonsteroidal anti-inflammatory drugs (NSAIDs) and nonselective beta-blockers (often used for heart disease)
- Chemicals used to preserve foods: usually the sulfites found in a number of foods and drinks
- Upper respiratory infections: such as colds and other viral infections of the lungs[2]
- Exercise and other physical activities[3]
- Cold or dry air
- Other health conditions: such as heartburn (acid reflux), stress and sleep apnea
-
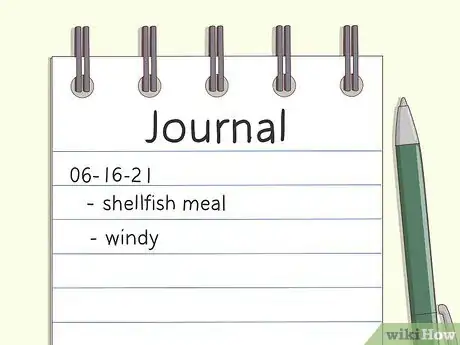
2Keep a diary to identify any unknown triggers. After you have a coughing fit, ask yourself what triggered it. If you're having trouble identifying common triggers, you may have to consider if there's an unknown trigger that you need to find. Keep a journal of your daily routine so you can determine what you experienced right before the coughing attack. Ask yourself:[4]
- Has the season changed? Are there new environmental factors triggering my asthma?
- Is there a new industry nearby that may be spilling pollutants into the air?
- Have I added a new food into my diet? Am I taking any new medications that might be interfering with my asthma medication?
- Has the weather changed suddenly? Was it warm and it is now cool and damp? Is it windy or has the wind changed direction? The wind may be bringing in new irritants.
Advertisement -
3Get tested for food allergies. If you suspect that a food allergy is triggering your asthma cough, don't simply cut the food from your diet. This could lead to a nutritional deficiency. Instead, talk to your doctor about getting skin prick testing to determine what you're allergic to. Your doctor can then recommend strategies for managing the allergy. Common food allergies include:[5]
- Gluten (a protein found in any wheat product)
- Casein (a protein found in dairy products)
- Eggs
- Citrus
- Fish and shellfish
- Peanuts
-
4Monitor your lung function. If you're having trouble identifying your asthma triggers, talk with your doctor about monitoring your peak expiratory flow rate (PEF) using a small portable tool. This will show how effective your lungs are at pushing air out. As your airways narrow your PEF will drop. Regularly checking your peak function and tracking your daily activities/foods can help you and your doctor determine your asthma triggers.[6] [7]
- Measuring your lung function is especially helpful if your triggers don't cause an immediate coughing fit. Some people find that their triggers take some time before an attack comes on.
Getting Comfortable
-
1Drink plenty of water. Keep the mucus in your throat loose by drinking six to eight 8-ounce glasses of water every day. If you have a dry cough that doesn't produce anything, you need to stay hydrated so the coughing doesn't irritate your throat. This is especially important if colds and flu are triggers for your asthma symptoms.[8]
- Increase your fluid intake if you're coughing up yellow or green mucus.
-
2Purify the air. Keep the air in your home as pure as possible. Check any air filters in your home and avoid smokers. Since smoke is a common asthma trigger, talk to any smokers about not smoking around you. You should also avoid spraying hairspray and perfume.[9]
- Since pollen can trigger your asthma, you should consider running an air conditioner on days when the pollen count is high. Just take care to regularly clean the air vents in your home so dust and mold isn't blown around.
- Consider running a humidifier or leaving bowls of water around your home. This will add moisture to the air which can improve your breathing.
-
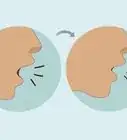
3Relax your breathing. Avoid deep over breathing when you have an asthma cough. Some doctors believe that this can irritate your lungs even more. Instead, slowly breath only through your nose, keeping your inhalations and exhalations the same length. For example, breathe in through your nose while counting to 8. Hold your breath for as long as you can and breathe out for 8 counts. Stay calm, relaxed and still while you breathe.
- While you'll be getting a little less oxygen during this exercise, it's about the same amount you'd be getting if you were coughing. Controlling your breathing by counting can decrease the cough and other symptoms of asthma.[10]
-
4Try yogic breathing. A coughing fit brought on by asthma can make you feel panicked or out of control. Calm yourself and your breathing by practicing a relaxing breathing pose. Lay on your back and bend your knees so that your feet are still flat on the floor. Place your hands on your belly put a pillow under your head so you're more comfortable. Close your eyes and let your belly sink down with each breath.[11]
- The goal of this exercise is to relax your breathing which can calm coughing. While you slowly breathe, try to calm your mind and your thoughts.
-
5Remove yourself from an uncomfortable environment. Emotions do not directly cause asthma, but the changes in your rate and rhythm of breathing that accompany emotions can trigger an attack. Severe anxiety and actions like crying and yelling can affect your breathing and bring on an attack. Even emotional distress brought on by an attack itself can worsen your symptoms. Learning techniques to cope with stress and anxiety may help prevent these episodes.[12]
Taking Medications
-
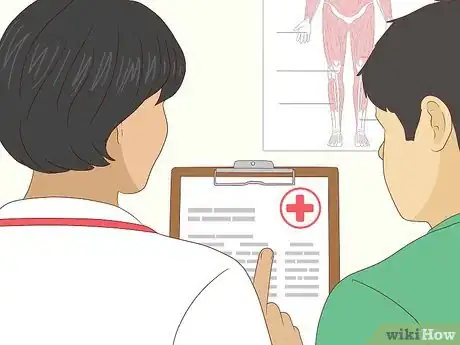
1Create an action plan with your doctor. Your doctor will work with you to create a written plan that you can follow when you start having an asthma attack or coughing fit. The action plan should give you a list of steps to follow to get your breathing back to normal. It should also list emergency and medical contacts.[13]
- The doctor will explain how the action plan moves from green to yellow to red. Each colored section should list symptoms you should look for, your medication and treatments, and a place for you to record your lung function.
-
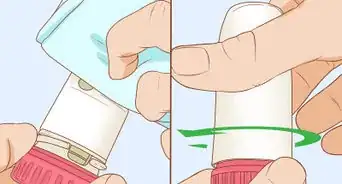
2Control your asthma with short-term medication. If you're having a coughing attack, you'll probably be advised to use an inhaler. Your inhaler is designed to quickly get medication (like short acting beta agonists) into your airways so they open.[14] Your doctor may prescribe[15] [16] albuterol, levalbuterol, pirbuterol, ipratropium, or corticosteroids[17] .
- To use an inhaler, take off the cap and shake the inhaler. Three or four good shakes should work. Remove the cap and breathe out.
- Put the inhaler mouthpiece to your mouth and breathe in slowly. Press down once on the inhaler's button, and continue taking in one long, slow breath.
- Take the inhaler out of your mouth. Hold your breath for ten seconds, and then breathe out.
-
3Treat asthma with long-term medication. These medications are used every day to prevent coughing and other asthma symptoms. They won't give immediate relief (you should use your inhaler or other short-term medication for that). Instead, long-term medications can reduce inflammation, open your airways, and reduce your body's response to triggers. You may also need treatments for allergies that trigger asthma attacks. Long-term medications or treatments include:[18]
- Allergy shots
- Inhaled corticosteroids like fluticasone, budesonide, flunisolide, ciclesonide, beclomethasone and mometasone
- Anti-inflammatory medicines like cromolyn
- Long-acting beta agonists like salmeterol and formoterol
- Biological medicines like omalizumab and leukotriene modulators
- Theophylline
-
4Get immediate medical attention. An important part of managing your asthma cough is knowing when to get medical treatment for it. Besides cough one hallmark sign of worsening asthma is wheezing. Wheezing is a high pitched whistling sound produced when air is forced through narrowed airways. Usually a wheezing sound is created when breathing out but can also occur when breathing in.[19] Call your doctor immediately if you have to take more medication than advised, your coughing (or other) symptoms get worse, you have trouble breathing while talking, or your peak flow measurement is only 50 to 80% of your personal best measurement. You should go to the emergency room for help if:[20]
- You feel sleepy or confused
- You have severe shortness of breath while resting
- Your peak flow measurement is less than 50% of your personal best
- You have severe chest pain
- Your lips and face look blue
- You have extreme difficulty breathing
- Your pulse is rapid
- You have severe anxiety because of shortness of breath
Expert Q&A
Did you know you can get expert answers for this article?
Unlock expert answers by supporting wikiHow
-
QuestionHow can I stop my asthma cough at night?
 Shaun Berger, MDDr. Shaun Berger is a board certified Pediatrician based in the San Diego, California metro area. Dr. Berger provides comprehensive primary care for newborns, children, and adolescents, focusing on preventive medicine. Dr. Berger earned a BA in Psychology from the University of California, San Diego and an MD from the University of Illinois at Chicago. Dr. Berger then completed a residency at the UCSF/Fresno Community Medical Centers/Valley Children’s Hospital where he was elected Chief Resident. He has been awarded the UCSF Foundation Award and is a Fellow of the American Academy of Pediatrics.
Shaun Berger, MDDr. Shaun Berger is a board certified Pediatrician based in the San Diego, California metro area. Dr. Berger provides comprehensive primary care for newborns, children, and adolescents, focusing on preventive medicine. Dr. Berger earned a BA in Psychology from the University of California, San Diego and an MD from the University of Illinois at Chicago. Dr. Berger then completed a residency at the UCSF/Fresno Community Medical Centers/Valley Children’s Hospital where he was elected Chief Resident. He has been awarded the UCSF Foundation Award and is a Fellow of the American Academy of Pediatrics.
Board Certified Pediatrician
-
QuestionWill my asthma get worse in cold, dry air?
 Shaun Berger, MDDr. Shaun Berger is a board certified Pediatrician based in the San Diego, California metro area. Dr. Berger provides comprehensive primary care for newborns, children, and adolescents, focusing on preventive medicine. Dr. Berger earned a BA in Psychology from the University of California, San Diego and an MD from the University of Illinois at Chicago. Dr. Berger then completed a residency at the UCSF/Fresno Community Medical Centers/Valley Children’s Hospital where he was elected Chief Resident. He has been awarded the UCSF Foundation Award and is a Fellow of the American Academy of Pediatrics.
Shaun Berger, MDDr. Shaun Berger is a board certified Pediatrician based in the San Diego, California metro area. Dr. Berger provides comprehensive primary care for newborns, children, and adolescents, focusing on preventive medicine. Dr. Berger earned a BA in Psychology from the University of California, San Diego and an MD from the University of Illinois at Chicago. Dr. Berger then completed a residency at the UCSF/Fresno Community Medical Centers/Valley Children’s Hospital where he was elected Chief Resident. He has been awarded the UCSF Foundation Award and is a Fellow of the American Academy of Pediatrics.
Board Certified Pediatrician
References
- ↑ http://www.nhlbi.nih.gov/health/health-topics/topics/asthma/signs
- ↑ Shaun Berger, MD. Board Certified Pediatrician. Expert Interview. 17 April 2020.
- ↑ Shaun Berger, MD. Board Certified Pediatrician. Expert Interview. 17 April 2020.
- ↑ https://www.thoracic.org/patients/patient-resources/resources/asthma.pdf
- ↑ https://www.asthma.org.uk/advice/triggers/food/
- ↑ https://www.ghc.org/kbase/topic.jhtml?docId=aa6768
- ↑ http://www.lung.org/lung-health-and-diseases/lung-disease-lookup/asthma/living-with-asthma/managing-asthma/measuring-your-peak-flow-rate.html
- ↑ http://getasthmahelp.org/asthma-triggers.aspx
- ↑ https://www.aafa.org/control-indoor-allergens/
- ↑ http://www.normalbreathing.com/diseases-Asthma.php
- ↑ http://www.yogajournal.com/article/health/asthma-answers/
- ↑ http://getasthmahelp.org/asthma-triggers.aspx
- ↑ http://www.lung.org/lung-health-and-diseases/lung-disease-lookup/asthma/living-with-asthma/managing-asthma/create-an-asthma-action-plan.html
- ↑ Shaun Berger, MD. Board Certified Pediatrician. Expert Interview. 17 April 2020.
- ↑ http://www.medicinenet.com/asthma_medications/article.htm
- ↑ https://www.nlm.nih.gov/medlineplus/ency/article/000141.htm
- ↑ http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4166064/
- ↑ http://www.nhlbi.nih.gov/health/health-topics/topics/asthma/treatment
- ↑ http://www.mayoclinic.org/symptoms/wheezing/basics/definition/sym-20050764
- ↑ https://www.nlm.nih.gov/medlineplus/ency/article/000141.htm





























































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...