This article was medically reviewed by Lacy Windham, MD. Lacy Windham, MD, is a Board-Certified Obstetrician & Gynecologist in Cleveland, Tennessee. Dr. Windham attended medical school at the University of Tennessee Health Science Center in Memphis. Her residency was completed at Eastern Virginia Medical School in Norfolk, Virginia. She was the recipient of multiple awards during her residency training, including Most Outstanding Resident in Maternal Fetal Medicine, Most Outstanding Resident in Oncology, Most Outstanding Resident Overall, and Special Award in Minimally Invasive Surgery.
There are 10 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 180,527 times.
At the end of your third trimester, your body will begin to show signs that it is time for your baby to be born through labor and delivery. Although every birth is unique and hard to predict, adequate preparation can help you feel more confident when you go into labor and help your birthing experience go as smoothly as possible. As you prepare for labor and delivery, you should consult a healthcare professional every step of the way and prepare as much as possible for the new addition to your family.
Steps
Prepping Your Body for Delivery and Labor
-
1Understand the three stages of labor. Though the duration of each stage will vary for every mother, you will experience all three stages during your labor:[1]
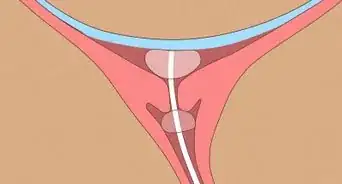
- The first stage of labor includes early labor and active labor. During stage one, the muscles of your uterus start to tighten, or contract, and then relax, which will help to thin and open the cervix so your baby can pass through the birth canal. Your labor will begin with early contractions that are irregular and last less than a minute. This early phase can last from a few hours to days. You will then experience active contractions that are regular and last about a minute. Once you experience active contractions, you will need to head to a hospital or birthing center. You will eventually transition to the second stage of labor, when your cervix opens completely and you are ready to give birth.
- The second stage lasts through the actual birth. During the second stage, your cervix is completely dilated and your baby travels down and out of the birth canal. Your baby will then be born.
- The third stage of labor occurs after your baby is born. You will have contractions until the placenta is delivered out of your birth canal.
-
2Do Kegel exercises in addition to daily exercise. You should maintain a daily exercise routine of light to mild exercise during your entire pregnancy and focus on doing Kegel exercises to strengthen your pelvic muscles and ligaments. These exercises will help your body prepare for labor and delivery.[2]
- To do Kegel exercises, squeeze the same muscles in your pelvic area that you would use to stop your urine. Do not move your belly or your thighs, just your pelvic muscles.
- Hold the squeeze for three seconds, then release them for three seconds.
- Begin with holding and releasing for three seconds. Gradually add one second to the hold and release time every week until you are able to squeeze for 10 seconds.
- Repeat the Kegel exercise 10 to 15 times per session. Do three or more sessions a day.
Advertisement -
3Take birthing and parenting classes with your partner. If you have a partner who is going to be part of the baby’s life, you should both attend birthing and parenting classes before you give birth. If you are having a hospital birth, your hospital can provide birthing classes and many medical clinics offer these classes as well.[3]
- During these classes, you will learn about how to breastfeed, how to care for your new baby, how to have a healthy pregnancy, and how to massage your infant.
-
4Ask your doctor about eating during labor. Most doctors will advise you to have clear liquids during labor and small snacks, like a piece of toast, applesauce, Jell-O, or popsicles, to keep your strength up as you go into delivery. However, you should avoid large, heavy meals (no steaks and no burgers) and only eat foods that will not upset your stomach as you will likely be feeling stomach pains already due to labor. [4]
- During labor, you should have liquids like clear chicken broth, made with low-sodium, fruit juice without pulp, tea, and sports drinks. You can also suck on ice chips to refresh you as you do your breathing exercises during labor.
- Some doctors may recommend clear liquids only, especially if they think you have a high likelihood of requiring a cesarean delivery.
Creating a Birth Plan
-
1Write down your birth plan with the assistance of your partner and your doctor. Though it is never possible to predict any delivery, having a written or typed birth plan can help you outline what you would like to occur during your labor and delivery. You should provide a copy of your birth plan to your partner, your doctor, and any staff at the hospital.
- Many hospitals will provide a standard birth plan that you can fill out and submit so they are aware of your wishes.
-
2Discuss your birthing options with your doctor. You can decide to have your baby at home (home birth), or in the hospital (hospital birth). You may decide to have your baby at a birthing center in your area, rather than at a hospital. It can be overwhelming to decide where you want your baby to be born, so discuss your options with your doctor and your partner before you make a decision. Ultimately, you should do what you feel is best for the health of you and your baby.[5]
- A hospital birth is a standard plan for many expecting women. You should look for a hospital that is located within driving distance to your home, and a doctor on staff that you feel comfortable with and trust. Many hospitals offer tours to expecting women, including the floor where you will likely give birth, so you are familiar with the environment before you deliver.
- A home birth is an alternative to a hospital birth and can provide you with comfortable atmosphere for your child’s birth.[6] There are risks involved with a home birth, however. You must carefully choose a midwife, being aware that the midwives that home birth in the US are not required to be certified and may not have any training. The mortality rate of newborns delivered during home birth is triple that of hospital births.[7]
-
3Decide at what point during your labor you are going to the hospital. If you are having a hospital birth, you should discuss at what stage of your labor you are going to plan to go the hospital. By the time you experience active contractions at the end of the first stage of labor, you should head to the hospital.
- Your midwife should also be made aware of when you are going to call her for assistance at home during your labor. Depending on the policies of your midwife, you may both decide on a rough estimate of when she should expect a call from you to come over to your home and assist with the birth. It may be necessary for you to give birth in a hospital if there are complications.
-
4Discuss your pain management options. Labor is an intense and painful process. Your doctor should outline your pain management options and you should agree on what level of pain you are going to sustain without or with medication. You may choose one or several of these options: [8]
- Epidural: This anesthetic is injected directly into your spine, bypassing your bloodstream. This makes it safer for your baby and ensures you receive quick pain relief. It is a popular pain relief option for many women in labor. Though it can take 15 minutes or longer to kick in, epidurals can be administered as soon as you request it, even if you are not dilated to a certain amount. The anesthesia will numb your entire lower body, including the nerves of your uterus, thereby numbing the pain of your contractions.
- Pudendal block: This is used to relieve early second-stage labor pain and is usually reserved for when you are at the vaginal delivery stage. Your doctor may use this medication if he needs to use forceps or a vacuum vaginal extraction. It will reduce pain in your perineal or vaginal area but you will still feel your contractions.
- Spinal block or saddle block: These pain relievers are rarely used for vaginal births. They are given in a single dose right before delivery if you did not have an epidural during labor but want pain relief for your delivery. They are fast acting pain relievers and you will be numb during your delivery. If you get a spinal block, you will need to stay flat on your back for eight hours post delivery.
- Demerol: This pain-relieving drug can be administered via a shot in the buttocks or an IV. You can be given Demerol two to three hours before you give birth and then given doses every two to four hours. The drug will not interfere with your contractions, and some women are given Demerol to give their contractions a more normal rhythm.
- Nubain: This is another pain-relief drug that is administered via IV. It is a synthetic opioid that does not numb the body but can reduce pain and anxiety.[9]
- Some doctors may use nitrous oxide (like they use in dental offices).
- General and regional anesthesia: General anesthesia is rarely used for delivery and only used for emergency surgical births. You will inhale or receive it via injection and it will put your entire body to sleep as the doctor performs an emergency Cesarean. It may also be required if you have a difficult vaginal breech birth to help deliver your baby’s head. You will be knocked out for the entire birth on general anesthesia and it can cause you to feel queasy and nauseous once you wake up from the birth.
- Natural birth (drug free): If you are concerned about using pain medication during your labor, you may decide to go for a drug free natural birth. Talk to your doctor about going unmedicated during your labor, or using a combination of medication and natural birthing techniques.
-
5Determine if you are going to personalize the birthing environment. If you are giving birth in a hospital, you should discuss any specific requests for the birthing environment in your hospital room. This could include dimming the lights, playing music, or wearing your own clothes as you give birth. Your doctor should be made aware of any specific request for the birthing area before you give birth.
- If you are giving birth at home, you should discuss the birthing environment with your partner and your midwife. You may decide to give birth in your bathtub or in a special pool made for home births. You may also decide to have music playing, lighting and other calming elements in the environment during the birth.
-
6Ask your doctor about situations that may require a Cesarean delivery. It’s important that you prepare for the possibility of a C-section in your birth plan. Phrase this as: “In the event it is necessary to perform a Cesarean delivery…”. Depending on your pregnancy, your doctor may recommend a C-section for medical reasons or your doctor may be required to perform a C-section in an emergency situation during your labor. Your doctor may recommend a C-section if:[10]
- You have certain chronic medical conditions like heart disease, diabetes, high blood pressure, or kidney disease.
- You have an infection like HIV or active genital herpes.
- Your baby’s health is at risk due to an illness or a congenital condition. If your baby is too large to move safely through the birth canal, your doctor may advise a C-section.
- You are overweight, as being obese can cause other risk factors and may require a C-section.
- Your baby is in the breech position, where she is feet-first or butt-first and cannot be turned.
- You have had a C-section during your previous pregnancies.
-
7Decide if you are going to breastfeed soon after delivery. Skin-to-skin contact during your baby’s first hour in the world is important for your baby’s health and to help you and your baby bond. This is called the Golden Hour and it is often recommended that you have skin-to-skin contact with your baby as soon as possible post-delivery. You should also decide if you are going to breastfeed after your baby is born, as the hospital should be made aware of your wishes. [11]
- Keep in mind the American Academy of Pediatrics (AAP) recommends that mothers breastfeed their newborns for the first six months of life and continue to breastfeed for at least 12 months. Breastfeeding can protect your baby from infections and reduce her risk of health problems like diabetes, obesity, and asthma.[12]
References
- ↑ https://www.healthwise.net/cdphp/Content/StdDocument.aspx?DOCHWID=tn9759
- ↑ https://www.healthwise.net/cdphp/Content/StdDocument.aspx?DOCHWID=tn9759
- ↑ http://womens.memorialhermann.org/labor-delivery/preparing-for-childbirth-at-memorial-hermann/
- ↑ http://www.whattoexpect.com/pregnancy/eating-well/week-40/eating-well.aspx
- ↑ http://www.whattoexpect.com/pregnancylabor-and-delivery/delivery-options.aspx
- ↑ http://www.viha.ca/children/pregnancy/birth/home_birth.htm
- ↑ http://www.sciencedirect.com/science/article/pii/S000293781000671X
- ↑ http://www.whattoexpect.com/pregnancy/labor-pain/
- ↑ http://americanpregnancy.org/labor-and-birth/narcotics/