This article was co-authored by Laura Marusinec, MD. Dr. Marusinec is a board certified Pediatrician at the Children's Hospital of Wisconsin, where she is on the Clinical Practice Council. She received her M.D. from the Medical College of Wisconsin School of Medicine in 1995 and completed her residency at the Medical College of Wisconsin in Pediatrics in 1998. She is a member of the American Medical Writers Association and the Society for Pediatric Urgent Care.
This article has been viewed 53,697 times.
If a child is unconscious and not breathing, it is critical that they receive help immediately. If the brain does not get oxygen, brain damage begins after only four minutes. The child may die within four to six minutes. CPR, or cardiopulmonary resuscitation, is a procedure in which you help the child breathe and provide chest compressions to make the heart beat until help arrives. If the child has a pulse, you should only provide rescue breathing. Do not perform chest compressions on a child over the age of one with a pulse.[1] Infants may require chest compressions if their heart rate is present but too low.
Steps
Determining What Is Needed
-
1Assess the situation. This stage is critical for determining what kind of assistance the child needs and if the assistance can be provided safely. You should:[2] [3]
- Check the area to make sure it is safe to provide rescue breathing. Make sure you are not in an area where you and the child are in danger of being hit by a car or coming in contact with live electrical wires.
- Check the child. Gently touch the child and ask loudly if the child is ok. Do not shake or move the child because if she has a neck or spinal injury, this could cause more damage.
- If the child does not respond shout for a bystander to call emergency responders. If people are standing around watching you, point to someone specifically and tell that person to call for help. If you are alone, perform rescue breathing for two minutes and then call 911.
-
2Determine what the child needs. At this point it is critical to assess whether the child is breathing and has a pulse:[4] [5]
- Check for breathing. Lean over the child so that your ear is near the child’s nose and mouth. Watch the child’s chest for breathing movements, listen for sounds of breathing, and notice whether you feel the child’s breath on your cheek. Check for breathing for no more than 10 seconds.
- Feel for a pulse. Press your index and middle finger on the side of the child’s neck, under the jaw.
Advertisement -
3Position the child for CPR. It is important that this step be done carefully, especially if there is the possibility that the child might have a spinal or neck injury. Avoid causing the child’s neck or body to twist. Position the child so he is lying flat on her back.
- If necessary, ask someone to help you gently roll the child onto his back. Coordinate your movements so that the spine is not twisted during the movement.
Providing Rescue Breathing for a Child with a Pulse
-
1Position the head for rescue breathing. The head should be straight and not tilted to either side. Perform the following movements to open the airway and make the rescue breaths as effective as possible:[6] [7]
- Put one hand under the child’s chin and the other on the top of the head. Gently tilt the head back and lift the chin.
- Use your thumb and forefinger to close the child’s nose. If the child is younger than one year, you don’t need to do this because you will breathe into both the child’s nose and mouth.
- Do not move the head more than necessary if you think the child may have a spinal cord injury.
-
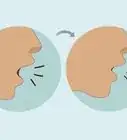
2Provide rescue breaths. Take breath and lean over the child so that your lips are over her mouth and form an airtight seal. If the child is younger than one year, cover both the nose and the mouth with your mouth. Breathe gently and steadily into the child’s mouth for one to one and a half seconds, watching for the chest to rise.[8] [9]
- After exhaling into the child’s mouth turn your head and watch to see if the chest deflates as it would during natural breathing. If so, this suggests that the breath was effective and the airway is not blocked.
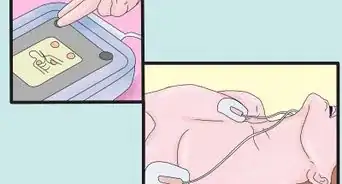
- If you have a barrier mask with a one-way valve, wear it while providing breathing assistance. This will protect you from any infections that the child may have.
-
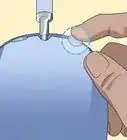
3Clear the airway if necessary. If the airway is obstructed, you may see that the breath you exhale doesn’t inflate the lungs. You may also feel that it blows back in your face instead of going into the child’s body. If this is the case, you need to check for an obstruction.[10] [11]
- Open the child’s mouth. Look inside to see if you see any pieces of food or objects that the child may have choked on. If so, remove them.
- Do not poke your fingers or any other object deep into the child’s throat. If you do, you run the risk of pushing an object further in.
- If you don't see an object, reposition the child's head and try another rescue breath. Consider performing maneuvers for possible choking or foreign bodies if you cannot get air in.
-
4Continue rescue breathing. Continue rescue breathing, giving one breath every three seconds for the child. Check for a pulse every two minutes while doing rescue breathing, and to perform regular CPR with chest compressions if the child loses her pulse. Continue with rescue breathing until one of the following occurs:[12]
- The child begins breathing on her own. You will notice that she is improving if she starts coughing or moving.
- Emergency responders arrive. At that point, they will take over.
References
- ↑ https://www.nlm.nih.gov/medlineplus/ency/article/000012.htm
- ↑ http://www.nhs.uk/conditions/pregnancy-and-baby/pages/resuscitating-a-baby.aspx
- ↑ https://www.nlm.nih.gov/medlineplus/ency/article/000012.htm
- ↑ https://www.nlm.nih.gov/medlineplus/ency/article/000012.htm
- ↑ http://www.nhs.uk/chq/Pages/2314.aspx?CategoryID=72&SubCategoryID=725
- ↑ http://www.nhs.uk/conditions/pregnancy-and-baby/pages/resuscitating-a-baby.aspx
- ↑ http://www.mayoclinic.org/first-aid/first-aid-cpr/basics/art-20056600
- ↑ http://www.nhs.uk/conditions/pregnancy-and-baby/pages/resuscitating-a-baby.aspx
- ↑ http://www.mayoclinic.org/first-aid/first-aid-cpr/basics/art-20056600
About This Article
To provide rescue breathing for a child, gently touch the child and ask loudly if they're ok. If they don't respond, ask someone to call 911 immediately. Then, check if they're breathing by placing your ear close to their mouth. You should also place 2 fingers on their neck to confirm if they have a pulse. After you've confirmed they have a pulse, carefully position the child on their back, and tilt their head back slightly by putting one hand under their chin. Next, hold the child’s nose closed with your thumb and forefinger, and place your lips over their mouth. Once you've exhaled into the child’s mouth, watch to see if their chest deflates, which indicates that the airway isn’t blocked. Continue providing 1 rescue breath every 3 seconds, so long as their chest deflates. However, if their chest doesn’t deflate, open their mouth to check for an obstruction, such as food they’ve choked on, and remove it. For tips from our Medical co-author, including what to do if the child loses its pulse, keep reading!