This article was medically reviewed by Shari Forschen, NP, MA. Shari Forschen is a Registered Nurse at Sanford Health in North Dakota. Shari has worked in healthcare since 1996 and her expertise lies in acute care bedside nursing on a medical oncology floor. She received her degree from Medcenter one College of Nursing in 2003 and her Family Nurse Practitioner Masters from the University of North Dakota in 2014. Shari is a member of the American Nurses Association.
There are 13 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 37,582 times.
An aneroid manometer is a device used by medical professionals to measure blood pressure, which is the force exerted on the walls of the arteries as the heart pumps blood around the body. The aneroid manometer is one of three main types of sphygmomanometer; both aneroid manometers and mercury manometers must be read manually and are used pretty much the same way, while the third, a digital sphygmomanometer, is automatic. Digital manometers are easier to use, but mercury and aneroid manometers are more accurate, though aneroid manometers need to be calibrated more often.[1] Blood pressure is recorded in millimeters of mercury (or mmHg) and varies depending on the patient's age, activity, posture, medication or any pre-existing diseases.
Steps
Preparing the Patient and the Equipment
-
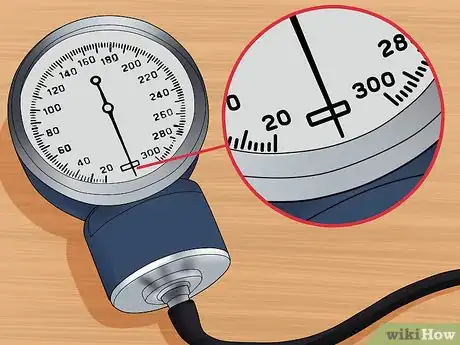
1Check to make sure the aneroid manometer is calibrated correctly. When you look at the dial, make sure it is at the zero baseline before starting. If it isn't, you need to calibrate it using a mercury manometer. Connect it with a Y connector, and once you move the dial over, check the pressure at several readings on both meters to make sure the aneroid manometer matches the mercury manometer.[2]
-
2Pick a cuff that is an appropriate size. Larger patients will need larger cuffs; otherwise, their blood pressure will read higher than it actually is. Similarly, smaller patients will need smaller cuffs; otherwise, their blood pressure will read lower than it actually is.[3]
- To pick the right size cuff, measure the bladder of the cuff against your patient's arm. The bladder is the part of the cuff where the air enters it. The bladder should go at least 80 percent of the way around the patient's arm.
Advertisement -
3Tell the patient what you are doing. You should perform this step even if you think the patient can't hear you due to unconsciousness. Tell the patient that you are going to use a cuff to take his blood pressure, and that he will feel some pressure from the cuff.[4]
- Remind the patient that he should not talk while you are taking his blood pressure.
- Try to calm down an anxious patient by asking about his day or something he enjoys. You can also ask him to take a few deep breaths to relax him. If you take the reading while he is still anxious, it can give a falsely high reading.Nonetheless, some patients will always be nervous in a doctor's office.
- If the patient is very anxious, try giving him five minutes to relax and calm down.
-
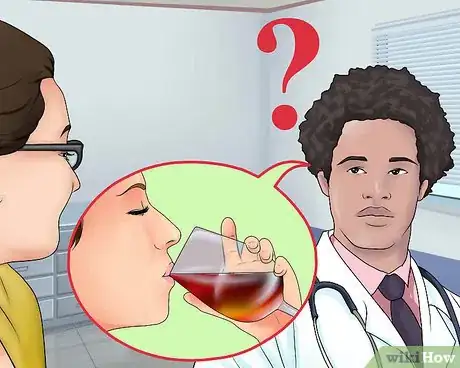
4Ask the patient questions. Ask if the patient has had an alcoholic beverage or smoked a cigarette in the 15 minutes prior to the test. Those two actions can affect the reading. Also ask the patient if she is on any medications that may affect blood pressure readings.[5]
-
5Get the patient into position. The patient can be standing, sitting, or lying down. If the patient is sitting, the arm should be bent at the elbow and his feet should be flat on the floor. Ensure that the arm is resting at the same level at the heart. If the patient supports his own arm, it can lead to a false reading.[6]
- The patient's arm should be bare of restrictive clothing with the sleeves of any clothing comfortably rolled up. However, ensure that the rolled-up clothing isn't cutting off the blood supply.
- The arm should be slightly flexed at the elbow, and supported throughout the reading on a flat, stable surface.
- Make sure the patient is comfortable in this position. If he's not, it can give a falsely high reading.
-
6Center the cuff over the brachial artery. Find the middle of the bladder by folding it in half.Make sure it doesn't have air in it already.[7] Palpate the brachial artery (the large artery on the inside of the elbow) with your fingers. Place the center of the bladder directly over the brachial artery.
-
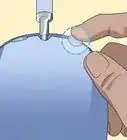
7Wrap the cuff around the patient's arm. Wrap the cuff of the manometer snugly around the patient's exposed upper arm. The bottom edge of the cuff should be approximately one inch above the bend of the elbow.[8]
- The cuff should be fairly tight to get an accurate reading. It should be tight enough that it should be hard for you to get two fingers under the edge of the cuff.
Taking a Reading
-
1Feel for a pulse. Put your fingers over the brachial artery. Hold them there until you can feel a pulse, called the radial pulse.[9]
-
2Pump air into the cuff. This step should be done quickly. You should let the cuff reach a point where you can't feel the radial pulse anymore. Note the pressure in mmHg.That pressure is a general guide for the systolic pressure.[10]
-
3Take the air out of the cuff. Release the air from the cuff. Add 30 mmHg to your previous reading. That is, if you lost the pulse at 120 mmHg, add 30 to reach 150 mmHg.
- If you don't want to take it twice, a standard recommendation is to inflate to 180 mmHg.
-
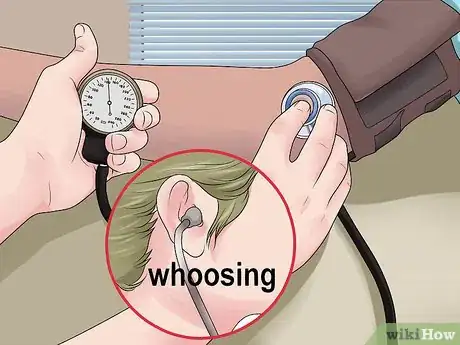
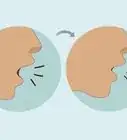
4Place the stethoscope bell on the brachial artery. You should hold the bell of the stethoscope on the patient's skin just below the edge of the cuff. It should center on the brachial artery so that you can hear the blood flow.[11]
- Never use your thumb to hold the head of the stethoscope in place. The thumb has a pulse of its own which can interfere with your ability to hear the patient's pulse. Hold the stethoscope in place with your index and middle fingers instead.
-
5Re-inflate the cuff. Add air into the cuff rapidly, until it reaches the number you found by adding 30 mmHg. Once you've hit that number, stop adding air.[12]
-
6Slowly let the air out. Let the air deflate from the cuff at a rate of 2 to 3 mmHg a second. While it is deflating, make sure you are listening in the stethoscope.[13]
-
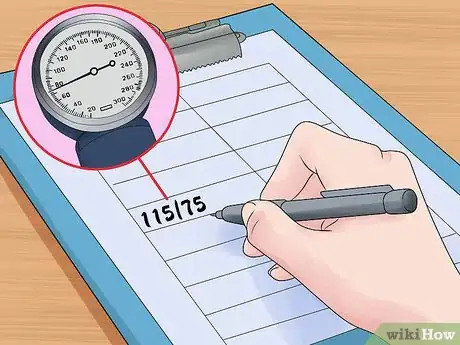
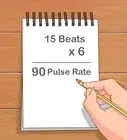
7Note when the sound begins. You should hear a knocking or beating sound, called "Korotkoff" sounds. When that sound begins, note the reading on the dial. That reading is the systolic pressure.[14]
- The systolic number represents the pressure that blood exerts against the walls of an artery following a heart beat or contraction.
-
8Note when the sound stops. After the beating starts, at some point you'll hear a rushing or "whooshing" noise. Once you can't hear that sound anymore, that reading is the diastolic pressure. Note that number, too. Release the rest of the air.[15]
- The diastolic number represents the pressure that blood exerts on the walls of an artery when the heart relaxes between contractions.
-
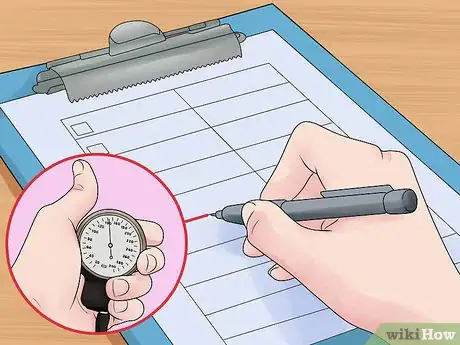
9Record the measurements. Write down the high and low numbers, as well as what size cuff you used. Also, write what arm was used and the position the patient was in.[16]
-
10Take the pressure again if it's high. You should take the blood pressure an additional two times if it's high; wait a couple of minutes between readings. Take the average of the last two readings as the final reading. If the final reading is high, you will want the patient to monitor her blood pressure to determine if she may have hypertension.[17] Keep in mind that two to three tests are not enough to determine hypertension.
- The patient should record her blood pressure for two to three weeks and record the results and bring this information to her physician for a proper diagnosis.
Reading and Understanding the Results
-
1Understand the dial. The dial runs from 0 mmHg up to about 300 mmHg. You shouldn't need numbers much past 200, as even systolic pressures over 180 constitute an emergency.[18]
-
2
-
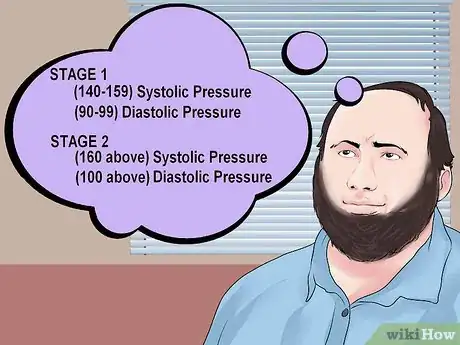
3Know what constitutes high blood pressure. Stage 1 high blood pressure (also called hypertension) is 140 to 159 in systolic pressure and 90 to 99 in diastolic pressure. Stage 2 high blood pressure is 160 or above in systolic pressure and 100 or above in diastolic pressure. If you're taking your own blood pressure, go to the emergency room if your systolic pressure is over 180 or your diastolic pressure is over 110.[21]
- Prehypertension runs from 120 to 139 in systolic pressure and 80 to 89 in diastolic pressure. A normal blood pressure range is anything under that, though your blood pressure can be too low.[22]
- Doctors do not have an exact range for low blood pressure. Generally, low blood pressure is only a problem if you're having symptoms. Symptoms include dizziness, an inability to concentrate, thirstiness, tiredness, nausea, fast breathing, and blurry vision.[23]
References
- ↑ http://www.practicalclinicalskills.com/sphygmomanometer.aspx
- ↑ http://www.steeles.com/catalog/takingBP.html
- ↑ http://www.steeles.com/catalog/takingBP.html
- ↑ https://www.nursingtimes.net/clinical-archive/assessment-skills/blood-pressure-monitoring-21-06-2007/
- ↑ https://www.nursingtimes.net/clinical-archive/assessment-skills/blood-pressure-monitoring-21-06-2007/
- ↑ https://www.cdc.gov/bloodpressure/measure.htm
- ↑ https://www.ncbi.nlm.nih.gov/books/NBK279251/
- ↑ http://www.practicalclinicalskills.com/blood-pressure-measurement.aspx
- ↑ https://www.nursingtimes.net/clinical-archive/assessment-skills/blood-pressure-monitoring-21-06-2007/
- ↑ https://www.ncbi.nlm.nih.gov/books/NBK279251/
- ↑ http://www.practicalclinicalskills.com/blood-pressure-measurement.aspx
- ↑ https://www.nursingtimes.net/clinical-archive/assessment-skills/blood-pressure-monitoring-21-06-2007/
- ↑ https://www.cdc.gov/bloodpressure/measure.htm
- ↑ https://www.ausmed.com/cpd/explainers/korotkoff-sounds
- ↑ http://www.practicalclinicalskills.com/blood-pressure-measurement.aspx
- ↑ http://www.steeles.com/catalog/takingBP.html
- ↑ http://www.steeles.com/catalog/takingBP.html
- ↑ https://www.ncbi.nlm.nih.gov/books/NBK279251/
- ↑ http://familydoctor.org/familydoctor/en/diseases-conditions/high-blood-pressure/diagnosis-tests/blood-pressure-monitoring-at-home.html
- ↑ http://www.heart.org/HEARTORG/Conditions/HighBloodPressure/AboutHighBloodPressure/Understanding-Blood-Pressure-Readings_UCM_301764_Article.jsp
- ↑ http://www.heart.org/HEARTORG/Conditions/HighBloodPressure/AboutHighBloodPressure/Understanding-Blood-Pressure-Readings_UCM_301764_Article.jsp
- ↑ http://www.heart.org/HEARTORG/Conditions/HighBloodPressure/AboutHighBloodPressure/Understanding-Blood-Pressure-Readings_UCM_301764_Article.jsp
- ↑ http://www.heart.org/HEARTORG/Conditions/HighBloodPressure/AboutHighBloodPressure/Low-Blood-Pressure_UCM_301785_Article.jsp
















-Step-3-Version-3.webp)

















































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...