This article was co-authored by Marc Kayem, MD. Dr. Marc Kayem is a board certified Otolaryngologist and Facial Plastic Surgeon based in Beverly Hills, California. He practices and specializes in cosmetic services and sleep-related disorders. He received his Doctorate in Medicine from the University of Ottawa, is board certified by the American Board of Otolaryngology, and is a Fellow of the Royal College of Surgeons of Canada.
There are 11 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 67,213 times.
Wearing an insulin pump 24/7 can be a daunting experience at first, and perhaps the part that new pumpers dread the most is wearing it in bed. Sleeping with a medical device attached to you brings its challenges, especially if there is more than one of you in the bed, but these challenges are not as difficult to overcome as they first appear. Those accustomed to wearing a pump report fewer episodes of nocturnal hypoglycemia than injection users, so while it may seem unusual at first, you'll soon learn to appreciate the benefits of sleeping with your insulin pump.
Steps
Getting Comfortable with Your Insulin Pump
-
1Try to forget it’s there. Much of the struggle of sleeping with an insulin pump is psychological.[1] Keep in mind that it's only about the size of a cell phone. Trying to forget it’s there or to keep it from your mind may help aid the sleeping process. As long as you’re thinking about the pump, it will be difficult for you to get restful sleep.
- Establish a safe and secure place for your insulin pump before going to bed so you don’t have to worry about its location while you’re trying to sleep.
- Try not to let your mind focus on the feeling of the pump or accessories. Instead focus on things that help you sleep, such as the things found in How to fall asleep.
- Give yourself time to get accustomed to using your insulin pump, changes take time to get used to, but most people find they can sleep easily with one after a short transition.[2]
- Set aside some time before you go to sleep to do something relaxing, like read a book or go for a walk. If you can calm your mind and reduce your stress before bed, you’ll have an easier time falling asleep.[3]
-
2Prepare those you share a bed with ahead of time. Part of the stress of sleeping with an insulin pump is based on how it may affect those you share your bed with. The easiest way to overcome this stressor is to speak openly with your family about your insulin pump.
- Discuss the insulin pump with your significant other so you can both address any questions that may arise.
- If you share a bed with your children it might be time to have them sleep in their own beds. Insulin pumps are resilient pieces of equipment but children could easily get tangled up in the tubes or play with the pump as you sleep.
Advertisement -
3Don’t be afraid of your insulin pump. Insulin pumps are designed for everyday use and are surprisingly resilient. The longer you live with your pump, the more familiar you will become with it and how it works. Spend some time familiarizing yourself with it and learning what it’s capable of.[4]
- Insulin pumps are built to be worn all day and slept with, so they can take a decent amount of punishment with little to no issue.
- If you roll onto your insulin pump, it will not damage it. It may make you a bit uncomfortable, so you may wake up to roll over.
- Insulin pump buttons are designed to be very difficult to press by accident, so even if you sleep on the pump, the chances of causing any issues are very low.
-
4Learn the risks. Sleeping with an insulin pump is extremely safe. The pumps have been designed to be worn 24 hours a day and are very resistant to issues like crimped tubes or accidentally pressing a button, but you should still be aware of the risks and how to address an emergency if it were to arise. The biggest risk associated with sleeping with an insulin pump is if it were to stop working overnight for some reason.[5]
- Keep the materials nearby that you will need to test your blood glucose levels and administer insulin via an injection if your pump were to stop working.
- The pump is fitted with an alarm in the event there is an issue, such as a blockage (occlusion) or low battery. However, a cannula coming off in the middle of the night will not set off an alarm. Thankfully, you should be able to feel the painful ripping of the adhesive.
Choosing Placement of the Pump
-
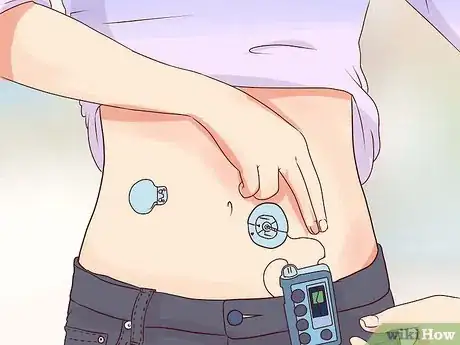
1Clip your pump to you. You have a number of options when it comes to where to place your insulin pump for bed. One way you may find comfortable is clipped to the waistband of your pants or shorts.[6]
- This method keeps the insulin pump close to you and reduces the chances of you getting tangled up in the hoses.
- You may roll onto the pump, but once people get used to it, they tend to roll back over without waking up.
- It is very unlikely that rolling onto your insulin pump will cause any issues, but be aware that it is possible.
-
2Lie the pump on the bed beside you. If you are uncomfortable with sleeping with your insulin pump attached to your clothing, you may choose to sleep with it on the bed beside you. Depending on the length of the tubes, you may want to inform your partner about where you place it.
- This may be more comfortable as you are less likely to roll onto the pump as you sleep.
- Be careful not to place your pump somewhere where it could easily fall off the bed.
-
3Protect your skin from irritation. If you sleep with the insulin pump clipped to your clothing or near you in bed, you may want to take steps to ensure it won't irritate your skin. Bare plastic can cause you to itch or even create a rash.
- Place the pump in a sock so the material of the pump can’t bother your bare skin.
- Use an armband designed for iPhones or other large smartphones to cover the pump and even to wear it on your arm. Some people wear them on a wristband, in their underwear, shorts, or bra.
- If you get up frequently at night, it may be best to wear your pump in this fashion or to clip it to your clothes to prevent dropping it.
-
4Place the pump near your bed. If you are nervous about rolling onto your insulin pump or pushing it off the bed, placing it near your bed on a nightstand or something similar may be best for you.[7]
- Placing the pump on your nightstand may require longer tubing.
- You will not roll over the pump nor will you knock it off the bed.
- You run an increased chance of getting tangled up in the hoses, but chances of a malfunction are still low.
Keeping Your Glucose Levels Within the Target Range
-
1Check your Blood Glucose levels frequently at first. For the first week or two, you will need to check your glucose levels very often to help you fine tune your insulin pump for your needs.[8]
- Check your BG (Blood Glucose) levels eight to ten times per day for the first one to two weeks.
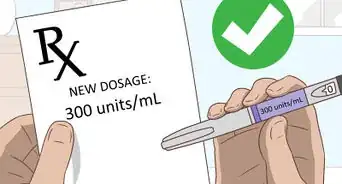
- You or your doctor may need to adjust settings like your basal rate, target ranges or sensitivity factor to treatment based on your checks.
- Your doctor may be able to give you a glucometer and prescribe you test strips in order for you to check you blood glucose levels frequently.
-
2Pay special attention to your blood glucose levels at night. Your body handles insulin treatment differently while you’re sleeping, so you need to check your levels often until you have your settings just right.[9] Some people have hyperglycemia at night. One symptom of this is nocturia, which is increased nighttime urination.
- Check your blood glucose levels right before bed and again when you wake up.
- Check your levels midway through your night’s sleep or every three to four hours of sleep.
- Discuss your readings with your doctor to ensure your overnight basal rates are set correctly.
-
3Continue to check your night levels often. Even after you have your settings right, you should still check your blood glucose levels in evenings. Your body may change how well it handles the treatment and you may require alterations to your dosages or treatment plan. [10]
- Check your blood glucose levels before you go to bed to help prevent high or low blood glucose levels while you’re asleep.
- Check your levels when you first get up to make sure your blood glucose levels are high enough.
- Occasionally check your blood glucose levels in the middle of the night to make sure you are still on the right course of treatment.
-
4Understand what causes low blood glucose levels. Low blood glucose can occur when you make changes from the normal activity accounted for in your treatment plan. Be conscious of the things you do that may affect your body’s insulin levels.
- Accidentally taking too much medication designed for diabetes treatment can dramatically lower BC levels.[11]
- Skipping meals or eating less than usual can cause your blood glucose level to be lower than intended.
- Exercising more than normal or right before bed can cause your blood glucose levels to drop while you sleep.[12]
-
5Look for the symptoms of nighttime hypoglycemia. You can identify problems before checking your blood glucose levels by learning what symptoms to look for when your blood glucose level drops dangerously.[13]
- Waking up sweating can indicate that your blood glucose level is too low.
- Waking up with a headache can also indicate low blood glucose levels.
- Waking up as a result of a sudden nightmare may indicate your blood glucose levels are low.
- Other symptoms include tremor, palpitations, anxiety, and seizure.
-
6Think about what you eat and drink. Some nights are bound to break the norm and involve different levels of eating or drinking, just make sure you take that into account before bed.[14]
- Don’t forget about what insulin you’ve already taken. Even fast acting insulin can remain in your system for up to four hours, so take all insulin you’ve taken recently into account when determining your dosage.
- Don’t have midnight snacks. If you snack regularly, make a habit of adjusting your boluses to reflect your snacks.
- Remember that alcohol can suppress a liver’s secretion of glucose, so have an extra snack (without insulin) at bedtime after drinking.
Expert Q&A
-
QuestionWhat happens if I don't get enough sleep?
 Marc Kayem, MDDr. Marc Kayem is a board certified Otolaryngologist and Facial Plastic Surgeon based in Beverly Hills, California. He practices and specializes in cosmetic services and sleep-related disorders. He received his Doctorate in Medicine from the University of Ottawa, is board certified by the American Board of Otolaryngology, and is a Fellow of the Royal College of Surgeons of Canada.
Marc Kayem, MDDr. Marc Kayem is a board certified Otolaryngologist and Facial Plastic Surgeon based in Beverly Hills, California. He practices and specializes in cosmetic services and sleep-related disorders. He received his Doctorate in Medicine from the University of Ottawa, is board certified by the American Board of Otolaryngology, and is a Fellow of the Royal College of Surgeons of Canada.
Sleep Specialist You're almost certainly going to end up tired and irritable on the days you don't nearly enough a sleep. If you consistently struggle to fall asleep even when you're relaxed, haven't had any caffeine, and you've been up for some time, you may have insomnia. See a doctor to get evaluated.
You're almost certainly going to end up tired and irritable on the days you don't nearly enough a sleep. If you consistently struggle to fall asleep even when you're relaxed, haven't had any caffeine, and you've been up for some time, you may have insomnia. See a doctor to get evaluated. -
QuestionCan you swim with an insulin pump?
 Chris M. Matsko, MDDr. Chris M. Matsko is a retired physician based in Pittsburgh, Pennsylvania. With over 25 years of medical research experience, Dr. Matsko was awarded the Pittsburgh Cornell University Leadership Award for Excellence. He holds a BS in Nutritional Science from Cornell University and an MD from the Temple University School of Medicine in 2007. Dr. Matsko earned a Research Writing Certification from the American Medical Writers Association (AMWA) in 2016 and a Medical Writing & Editing Certification from the University of Chicago in 2017.
Chris M. Matsko, MDDr. Chris M. Matsko is a retired physician based in Pittsburgh, Pennsylvania. With over 25 years of medical research experience, Dr. Matsko was awarded the Pittsburgh Cornell University Leadership Award for Excellence. He holds a BS in Nutritional Science from Cornell University and an MD from the Temple University School of Medicine in 2007. Dr. Matsko earned a Research Writing Certification from the American Medical Writers Association (AMWA) in 2016 and a Medical Writing & Editing Certification from the University of Chicago in 2017.
Family Medicine Physician No you should not swim with and insulin pump. Talk to your endocrinologist to see if there is a special insulin pump that you can swim with.
No you should not swim with and insulin pump. Talk to your endocrinologist to see if there is a special insulin pump that you can swim with.
Warnings
- If you have a curious pet that shares the bed with you, just be careful of your pet's interest in chewing or pulling at the pump.⧼thumbs_response⧽
- If you have a tendency to wake up before you change positions in the bed, worried about the pump's position or just because you're a light sleeper, you may suffer from sleep deprivation. It is recommended that you discuss this issue with your doctor if it is causing you sleep problems.⧼thumbs_response⧽
References
- ↑ Marc Kayem, MD. Sleep Specialist. Expert Interview. 24 October 2019.
- ↑ http://www.libertymedical.com/diabetes/article/living-with-a-pump/
- ↑ Marc Kayem, MD. Sleep Specialist. Expert Interview. 24 October 2019.
- ↑ http://www.diabetes.co.uk/insulin-pumps/sleep-and-insulin-pumps.html
- ↑ https://www.tandemdiabetes.com/important-safety-information
- ↑ http://www.diabetes.co.uk/insulin-pumps/sleep-and-insulin-pumps.html#where
- ↑ http://www.diabetes.co.uk/insulin-pumps/sleep-and-insulin-pumps.html#where
- ↑ https://www.medtronicdiabetes.com/sites/default/files/library/support/Basics%20of%20Insulin%20Pump%20Therapy.pdf
- ↑ https://www.medtronicdiabetes.com/sites/default/files/library/support/Basics%20of%20Insulin%20Pump%20Therapy.pdf
- ↑ #https://www.medtronicdiabetes.com/sites/default/files/library/support/Basics%20of%20Insulin%20Pump%20Therapy.pdf
- ↑ https://medlineplus.gov/ency/article/000310.htm
- ↑ http://www.joslin.org/info/avoiding_nighttime_lows.html
- ↑ http://www.joslin.org/info/avoiding_nighttime_lows.html
- ↑ http://www.diabetesselfmanagement.com/managing-diabetes/blood-glucose-management/exorcising-the-specter-of-nighttime-hypoglycemia/





































































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...