This article was medically reviewed by Erik Kramer, DO, MPH. Dr. Erik Kramer is a Board-Certified Primary Care Physician at the University of Colorado. With over 15 years of experience, his clinical interests include obesity and weight management, diabetes care, and preventive care, as well as embracing a holistic approach to primary care. He received his Doctorate in Osteopathic Medicine (D.O.) from the Touro University Nevada College of Osteopathic Medicine and completed his residency at Central Maine Medical Center. Dr. Kramer is a Diplomate of the American Board of Obesity Medicine.
There are 17 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 10,780 times.
Rabies is a deadly disease, and while much progress has been made, it still largely remains a mystery. The good news is that if you've been exposed to the disease, you can be given a vaccine to help prevent the onset of the infection. While you can be tested for it, results will only show up after the incubation period, which is when the disease becomes untreatable. Therefore, if you suspect you've been exposed, it's best to go in the day you are bitten or wounded to start the vaccination process. In animals, the main diagnostic tactic is watching for symptoms, as tests for this disease in animals can only be performed after death.
Steps
Watching for Symptoms in Animals
-
1Pay attention if your pet gets suddenly aggressive. While this doesn't automatically indicate rabies, it's almost definitely a sign that something is wrong. An aggressive dog or other pet may growl or snarl at you unexpectedly or try to bite or scratch you. It's important to take your animal to the veterinarian if you notice this symptom, especially if it's possible it could have been exposed to rabies and it's not been vaccinated for it.[1]
- Mainly, the disease changes behavior, so if you notice bizarre changes in your pet's behavior, it may be time to talk to your veterinarian.
- Be as careful as you can when trying to get your pet to the vet. Put on gloves and place a blanket or towel over your pet to help get it into the carrier.[2]
-
2Stay back if wild animals seem too friendly. Because this disease changes behavior, it may have the opposite effect in wild animals than it does in pets. They may wander up to you without any sign of fear, which is generally abnormal. If you notice this behavior, don't try to pet the animal or get near it. Stay as far back as possible.[3]
- While there are some exceptions to this rule, such as animals that have become accustomed to being fed in parks, it's still a good idea to stay back from wild animals. You never know what they're going to do.
Advertisement -
3Notice overreactions to light and sound. As the disease gets worse, animals may become oversensitive to stimuli. For instance, your pet may overreact to a loud noise, or they may be more affected than usual by bright lights.[4]
- In some cases, they may become very aggressive in reaction to sounds or lights.
-
4Look for animals that walk or move strangely. Because rabies is a neurological condition, it can change how an animal moves. If the animal looks clumsy or like it is unsteady on its feet, that's another indication it could have rabies.[5]
-
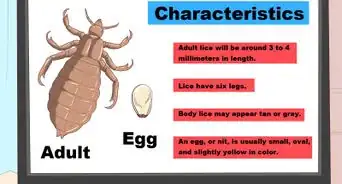
5Watch for too much saliva. This symptom is what is sometimes referred to as "foaming at the mouth." However, animals don't actually produce foam. Rather, they lose control of their facial muscles, and it causes them to hypersalivate.[6]
- They also won't be able to swallow, which makes this symptom worse.
- This is a late symptom of the disease, meaning the animal will die within a day or 2. Once an animal shows signs of rabies, though, there's nothing that can be done to save it.
Testing and Treating Animals
-
1Get your pet a booster vaccination within 5 days of exposure. If your pet has been exposed, a booster shot may help. Schedule a vet visit immediately to get a booster, but let your vet know that your pet may have been exposed to rabies so they can take extra precautions.[7]
- If your pet hasn't had the vaccination previously, the vet won't likely give the shot.
- Even if you can't get a booster shot, you still need to take your pet to the vet to have it checked out and possibly put it in quarantine.
-
2Expect a quarantine for your pet after a veterinarian visit. If you think your pet has rabies, the most likely course of action will be a quarantine if your veterinarian agrees with you. That's because there's no standard test for rabies in animals. The best the veterinarian can do is to have you isolate your pet and watch it for 10 days to see if more symptoms develop.[8]
- In some cities and states, the veterinarian may need to isolate your pet at the clinic away from other animals for the quarantine. In other areas, you may be able to take it home and confine it to an area where it can't get to other pets or humans. It depends on your local laws.
- With larger domestic animals, such as cows or horses, call your veterinarian about the animal, as they may want to come see it or they may have suggestions on how you can isolate it.
-
3Reintroduce your pet to its normal routine if it doesn't exhibit symptoms for 10 days. If your pet goes 10 days without showing symptoms, then congratulations, it is rabies-free! You'll be able to take the pet out of confinement and back into its regular routine.[9]
- This quarantine only applies to cats, dogs, and birds. With other animals, it's generally decided on the individual case.
- Unfortunately, if your pet exhibits signs of rabies within the 10 days, the condition is terminal. Though difficult, the humane thing to do is euthanize your pet at this point.[10]
-
4Be ready for a post-mortem test if your pet exhibits signs of rabies. In many cases, the veterinarian or your local government may want to perform a rabies test after the animal dies. This is the only way to test for rabies in animals, as it requires that small samples of brain tissue be taken and analyzed.[11]
- The reason they will want to confirm rabies is to be able to track the spread of disease in the area.
-
5Call animal control to capture a wild animal. If a wild animal is exhibiting behavior that's likely due to a rabies infection, it's important to call local animal control authorities. They will try to capture the animal and take it in to be euthanized. Then, the animal will be tested for rabies.[12]
Testing for and Treating Rabies in Humans
-
1Treat bites from wild animals seriously. Any warm-blooded animal can transmit rabies, including foxes, raccoons, skunks, bobcats, wolves, and coyotes. Bats are actually one of the most common animals to infect humans.[13]
- Bats can come in through open windows. If you wake up and a bat is in your room, you should see your doctor. They can actually bite you while you sleep without your realizing it.[14]
- Smaller animals can also transmit the disease, including squirrels, chipmunks, mice, and rats, but they are less likely to carry the disease.
-
2Capture the animal if you can. Don't try to kill it, as you may injure the head to the point that they can't test for rabies. If you don't think you can capture the animal safely, don't attempt it. Call animal control if it's a wild animal.[15]
- Tell your doctor you've done this so they can contact the local health department.
- If it's your pet, try to get it into a pet carrier to take to the veterinarian.
-
3Wash the wounded area immediately. Use soap and running water to thoroughly clean the wound, whether it's a bite or scratch. Because the virus is fragile, it's possible to wash it out of the wound, though you still want to take other actions to ensure you don't have the virus. You won't know for sure unless you see a doctor.[16]
- Wash and flush the wound for at least 5 minutes to make sure it's as clean as possible. You can use any hand soap for this process, though an antibacterial soap may help keep the wound from becoming infected.
-
4See your doctor for the wound the day you get the bite. Even if the wound isn't caused by a rabies-infected animal, it's still a good idea to see a doctor. Urgent care is likely the best option. While it isn't an emergency, you should have it looked at as soon as you can.[17]
- Alternatively, call your doctor the day it happens to see if they can fit you in.
- When you're bitten, the initial tests may come back as negative since the incubation period has just started and signs of rabies won't show until it has progressed to an infection. Your doctor may be able to test multiple ways, such as a skin biopsy, spinal tap, and saliva test to determine if you're infected.
- The incubation period for the virus is usually 20-60 days, but it may last longer than 6 months in very rare cases. You won't show symptoms until this incubation period is up.
-
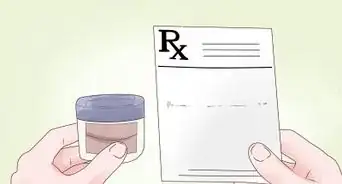
5Get the human rabies immunoglobin the day the bite occurs. This shot is fast-acting, and its purpose is to stop the virus from taking hold in your body. You should get this shot as soon as possible if you think you've been exposed.[18]
- In some cases, this might be more than one shot, as sometimes a portion of it is given near the bite wound.
- Start treatment immediately if you have a severe bite near your head, neck, or torso by a high-risk animal, such as a skunk, bat, or raccoon. You may be able to stop treatment after it's determined that the animal doesn't have rabies.
- If the animal didn't break skin when it bit your or its saliva didn't come into contact with an open wound, then you may not need any preventative treatment.
- Get yourself checked if you came into contact with a bat even if it didn't bite you since it may have possibly transferred the rabies virus to you.
-
6Expect a series of 4 shots over the next 14 days. The recommendations differ as to how many shots you receive. In some cases, it may be 4 shots over 14 days.[19] However, if you have a weakened immune system, you may get an additional shot on the 28th day.[20] Either way, your doctor will let you know the best course of action.
- These shots are given in the arm, and they aren't painful, except for the slight prick of the needle.[21]
-
7Expect a skin sample to be taken from your neck. This is one of the most common tests for rabies. The medical professional will take a small sample of skin to test. Don't worry; they will provide local anesthetics to numb the pain.[22]
- The same test that is performed on an animal's brain will be performed on your skin to look for the virus.
- You may also need to give saliva for the same reason.
-
8Be ready for a spinal tap to check for the virus. In a similar fashion as the skin sample, the medical professionals may take a spinal sample for testing. Like saliva, this isn't quite as reliable as the skin sample.[23]
- For a spinal tap, a medical professional will give you a local anesthetic with a needle to numb the area. Then, they'll insert a hollow needle into your spine between the vertebrae. They will withdraw a sample of fluid from this area and take the needle out. You may be sore in the area for a few days afterward.[24]
-
9Discuss diagnostic scans with your doctor. If your doctor suspects you have rabies, they might also perform scans of your brain, such as an MRI or a CT head scan. These aren't painful, but you will need to be completely still when having these scans done.[25]
References
- ↑ https://www.ndhealth.gov/disease/rabies/qanda.htm
- ↑ https://www.ncagr.gov/vet/FactSheets/Rabies.htm
- ↑ https://www.americanhumane.org/fact-sheet/rabies-facts-prevention-tips/
- ↑ https://www.americanhumane.org/fact-sheet/rabies-facts-prevention-tips/
- ↑ https://www.ndhealth.gov/disease/rabies/qanda.htm
- ↑ https://www.americanhumane.org/fact-sheet/rabies-facts-prevention-tips/
- ↑ https://www.ncagr.gov/vet/FactSheets/Rabies.htm
- ↑ https://www.ndhealth.gov/disease/rabies/qanda.htm
- ↑ https://www.mayoclinic.org/diseases-conditions/rabies/diagnosis-treatment/drc-20351826
- ↑ https://www.cdc.gov/rabies/specific_groups/veterinarians/potential_exposure.html
- ↑ https://www.americanhumane.org/fact-sheet/rabies-facts-prevention-tips/
- ↑ https://www.ndhealth.gov/disease/rabies/qanda.htm
- ↑ https://kidshealth.org/en/parents/rabies.html
- ↑ https://www.mayoclinic.org/diseases-conditions/rabies/symptoms-causes/syc-20351821
- ↑ https://www.mayoclinic.org/diseases-conditions/rabies/diagnosis-treatment/drc-20351826
- ↑ https://www.ndhealth.gov/disease/rabies/qanda.htm
- ↑ https://www.mayoclinic.org/diseases-conditions/rabies/diagnosis-treatment/drc-20351826
- ↑ https://www.mayoclinic.org/diseases-conditions/rabies/diagnosis-treatment/drc-20351826
- ↑ https://www.mayoclinic.org/diseases-conditions/rabies/diagnosis-treatment/drc-20351826
- ↑ https://kidshealth.org/en/parents/rabies.html
- ↑ https://www.cdc.gov/rabies/exposure/index.html
- ↑ https://medlineplus.gov/ency/article/001334.htm
- ↑ https://medlineplus.gov/ency/article/001334.htm
- ↑ https://www.mayoclinic.org/tests-procedures/lumbar-puncture/about/pac-20394631
- ↑ https://medlineplus.gov/ency/article/001334.htm