This article was medically reviewed by Troy A. Miles, MD. Dr. Miles is an Orthopedic Surgeon specializing in Adult Joint Reconstruction in California. He received his MD from the Albert Einstein College of Medicine in 2010, followed by a residency at the Oregon Health & Science University and fellowship at the University of California, Davis. He is a Diplomat of the American Board of Orthopaedic Surgery and is a member of the American Association of Hip and Knee Surgeons, American Orthopaedic Association, American Association of Orthopaedic Surgery, and the North Pacific Orthopaedic Society.
There are 17 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 39,922 times.
Spondylosis is a term that refers to arthritis or osteoarthritis of the spine. It is a degenerative disorder and represents the accumulation of wear and tear on the joints, ligaments, and discs of the spine over an individual’s lifetime.[1] Spondylosis can affect the neck (cervical spondylosis), upper and middle back (thoracic spondylosis), or low back (lumbar spondylosis). Cervical and lumbar spondylosis are the most common forms. Spondylosis is very common, and it is estimated that 80% of individuals older than age 40 have evidence of spondylosis on x-ray imaging.[2] Learn how to treat spondylosis so you can alleviate some of your pain.
Steps
Using Home Remedies To Relieve Pain from Spondylosis
-
1Use cold therapy. Cold therapy reduces swelling by causing a decrease in the diameter of blood vessels (vasoconstriction). It can also numb deep pain. Cold therapy can be applied using cold packs, bags of ice, cold rags, or bags of frozen vegetables or fruit.[3]
- Do not use ice packs or other cold therapy methods on the area for more than 15 to 20 minutes at a time.
- Always place a towel between the skin and the cold source.
- Refrain from using topical pain relievers at the same time you are applying cold.
- Do not use cold therapy if you have poor circulation.
-
2Try heat therapy. Heat therapy increases the diameter of blood vessels (vasodilation), which increases circulation. It also reduces muscle spasms and alters the sensation of pain. Heat therapy can be applied using heat packs, heating pads, or hot water bottles, or soaking a washcloth in warm water and applying to affected area.[4]
- You can also soak in a hot bath or shower.
- Do not use heat therapy for more than 15 to 20 minutes.
- Put a cloth between the skin and the heat source.
- Do not use topical pain relievers at the same time you are applying heat.
- Test the temperature to avoid burns. Avoid hot tubs or spas if you have high blood pressure or heart disease.
Advertisement -
3Take it easy for a few days. Taking it easy and getting bed rest for a few days can be helpful in some cases of severe pain due to spondylosis; however, any bed rest should be restricted to no more than one to three days, because any longer may prolong recovery.[5]
- Long-term bed rest also increases an individual’s risk for deep vein thrombosis (DVT), or a blood clot in the lower extremities. A DVT can lead to a pulmonary embolus (PE), or a blood clot in the lungs, which can be life-threatening.
-
4Get regular exercise. Regular exercise, even if modified during a painful episode of spondylosis, can help speed recovery. It is recommended to continue normal or near normal activities. Low-impact exercises, such as walking or swimming, are good choices. Yoga is a good form of exercise too. It’s been noted that individuals who walk daily are less likely to experience neck or low back pain.[6]
- In addition to thirty minutes of cardio exercise three times a week, you should do core exercises, such as pelvic lifts. This helps strengthen the core to support the spine.
- You should always talk to your physiotherapist before starting a new exercise. You and your physiotherapist can come up with an exercise routine that will be right for your specific condition.
-
5Wear a neck or back brace. Temporary bracing may help relieve the pain of spondylosis. Make sure not to wear it any longer than one week. Bracing allows muscles to rest. Long-term bracing is discouraged since it can weaken muscles and lead to more pain in the neck or low back.[7]
- You can obtain a soft neck brace from a pharmacy or doctor.
-
6Use a support pillow. Sleeping with a firm pillow below the neck or between the legs may help relieve the pain of spondylosis, especially if your pain is in the mid to lower back. Special pillows have been developed for the cervical spine or neck, which offer additional support that may help relieve pain. The pillow changes the direction of your spine, giving it added support and keeping it straighter while you rest.[8]
- There are special pillows designed for this function, but if you cannot locate one of these pillows, simply use the fullest pillow on your bed.
-
7Change your lifestyle. Lifestyle modification may be helpful for the spine at any age. Consider less strenuous work if your work entails an overabundance of bending or heavy lifting. If you are overweight or obese, losing weight can reduce stress on the spine. Quitting smoking can improve bone health, especially in the spine.[9]
- You should also consider your posture. If you slouch while sitting or standing, put more effort into correcting your posture and keeping your back and neck straight.
- There are additional natural methods you can try, though not all are backed up by good evidence.
Treating Spondylosis Medically
-
1Try over-the-counter pain relievers. The pain and other symptoms of spondylosis, whether acute or chronic, can be treated with home methods. Generally, the pain caused by spondylosis frequently improves after a few days. One good way to treat the pain is to use over-the-counter pain relievers.[10]
- Examples of OTC meds that help with this condition include non-steroidal anti-inflammatory drugs (NSAIDs), such as aspirin (Bayer, Ecotrin), ibuprofen (Motrin, Advil), and naproxen (Aleve). Acetaminophen (Tylenol) is another medicine that may also be helpful as a pain reliever.
- Acetaminophen is a safer option for individuals with a history of asthma, high blood pressure, liver disease, heart disease, or stomach ulcers.
-
2Use a topical pain reliever. Topical pain relievers can complement or be used an alternative to oral pain relievers. They can be administered in multiple ways, such as in creams, foams, gels, roll-ons, sprays, and sticks. The most common ingredients found in this class of medication are:[11] [12]
- Counterirritants. Examples of counterirritants include camphor, menthol, and methyl salicylate (oil of wintergreen). They work by creating a cooling or burning sensation that distracts an individual’s mind away from the pain. Popular brands include Bengay, IcyHot, and Tiger Balm.
- Capsaicin. Capsaicin is obtained from chili peppers and has been found to be very effective for topical pain relief. It causes a tingling or burning sensation upon the skin and may take several days before it actually relieves pain. Popular brands include Capzasin and Zostrix.
- Salicylates. Salicylates give aspirin its pain relieving qualities. They may be absorbed into the skin for local pain relief. A popular brand of topical salicylate is Aspercreme.
-
3Get a prescription medication. There are several varieties of prescription-strength pain medications that your doctor may give you to treat the pain associated with this condition when non-prescription drugs are no longer sufficient. Your doctor may prescribe prescription-strength NSAIDs that will reduce any inflammation associated with spondylosis.[13]
- Popular prescription NSAIDs include diclofenac (Voltaren), meloxicam (Mobic), nabumetone (Relafen), etodolac (Lodine), and oxaprozin (Daypro). Common side effects of NSAIDs may include dizziness, headache, nausea, diarrhea, and excess gas. Caution should be used if taking NSAIDs for longer than one week, as prolonged use increases the risk of stomach ulcers, kidney damage, and heart attacks.[14]
-
4Try muscle relaxants. Muscle relaxants may be prescribed to treat muscle spasm associated with spondylosis. Popular muscle relaxants include carisoprodol (Soma), cyclobenzaprine (Flexeril), methocarbamol (Robaxin), and metaxalone (Skelaxin).[15]
- Common side effects of muscle relaxants may include drowsiness, dizziness, dry mouth, and difficulty urinating.
- The use of muscle relaxants should be restricted to short-term due to their high risk for dependence or addiction.
-
5Talk to your doctor about a narcotic pain medicine. Depending on your level of pain, your doctor may choose to prescribe a narcotic pain medicine. Commonly prescribed narcotic pain medications include codeine, hydrocodone, and oxycodone.
- Common side effects of this class of medication may include drowsiness, constipation, dry mouth, and difficulty urinating.
- Narcotic pain medications should not be mixed with alcohol or other medications containing acetaminophen (Tylenol), as the combination can greatly increase the risk of liver damage.
- Use of narcotic pain medications should be curtailed to less than two weeks, because of the increased risks of tolerance, dependence, and addiction.[16]
-
6Ask about anti-seizure or antidepressant medications. Medications originally used to treat seizures, or epilepsy, have been found to be helpful in the treatment of chronic pain. Low doses of antidepressants have been used for years to treat chronic neck and back pain. Spondylosis can in a minority of cases lead to chronic neck or back pain.[17]
- The most commonly prescribed anti-seizure medications used to treat chronic pain are gabapentin (Neurontin) and pregabalin (Lyrica). It remains unclear how these medications control pain. Drowsiness and weight gain are common side effects of gabapentin. Common side effects of pregabalin may include drowsiness, dizziness, dry mouth, and constipation.
- Commonly prescribed tricyclic antidepressants (TCAs) helpful in the treatment of chronic pain include amitriptyline (Elavil), imipramine (Tofranil), and nortriptyline (Pamelor). Duloxetine (Cymbalta) is a novel antidepressant used in the treatment of chronic pain. Both TCAs and duloxetine work by increasing levels of the brain neurotransmitters norepinephrine and serotonin, which are instrumental in blocking the transmission of pain signals in the brain. Common side effects of these antidepressants may include drowsiness, weight gain, dry mouth, constipation, and difficulty urinating.
-
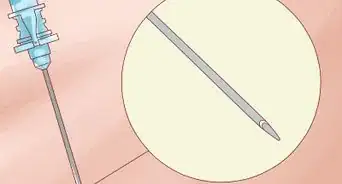
7Get an epidural steroid injection. An epidural steroid injection (ESI) is a minimally invasive procedure that may be used to treat pain caused by spondylosis. The injection is a combination of a long-acting steroid (triamcinolone, betamethasone) and an anesthetic agent (lidocaine, bupivacaine). The medications are injected into the epidural space of the spine, which is the area between the protective covering of the spinal cord (dura) and the backbone (vertebra). The duration of pain relief from an ESI varies and can last weeks, months, and sometimes even years.[18]
- It is recommended no more than three ESIs be performed in a 12-month period because exceeding this limit could weaken the spine.
- Potential complications of ESIs include infection, bleeding, and nerve damage.
- Types of physicians qualified to administer ESIs include physiatrists, anesthesiologists, radiologists, neurologists, and surgeons.
-
8Determine if you need surgery. The majority of patients suffering from spondylosis do not require spinal surgery. Nonsurgical treatment is successful in at least 75 percent of spondylosis cases, but in some instances, surgery does become a necessity. If you begin to experience neurologic deficits, like a loss of bowel or bladder control, surgery will likely be considered your best option. Loss of feeling or function in your arms, legs, feet, and fingers can be another sign of such deficits.[19]
- Under these circumstances, a nerve is being pinched or your spinal is being compressed. The underlying damage to your nervous system could worsen if these conditions are not fixed.
-
9Talk to your doctor about spinal decompression surgery. Spinal decompression surgery is a general term used to describe different surgical procedures that can relieve pressure on the spine. You will need to work with your doctor to determine the best technique for your circumstances.[20]
- During a laminectomy, bony arches of the spinal canal called lamina are removed, thereby increasing the size of the spinal canal.
- During a laminoplasty, the lamina are left in place but cut free along one side of your spinal cord.
- A discectomy is a technique that removes a portion of an intervertebral disc that has previously put pressure on a nerve root or on the spinal canal.
- With both the foraminotomy and the foraminectomy, the openings where the nerve roots exit the spinal canal are enlarged by the removal of tissue.
- You may undergo osteophyte removal, during which bone spurs are physically removed from areas in which they cause pinched nerves.
- During a corpectomy, a surgeon will remove an entire vertebral body and its discs.
Treating Spondylosis Using Other Methods
-
1Undergo physical therapy. Physical therapy (PT) may be prescribed by a physician for long-standing neck and back pain secondary to spondylosis. PT may combine passive treatments, such as ice and heat, ultrasound, and electrical stimulation, with therapeutic exercises to stretch and strengthen neck, abdominal, and back muscles.[21] [22]
- Physical therapy is usually prescribed for chronic pain that has lasted for several weeks without responding to other treatments.
- Massage therapy may also be introduced into your physical therapy routine. A professional massage therapist will work on the muscles in your back to soothe and relax them after you have exerted them.
- The goal of PT is to prevent recurring pain.
-
2Try spinal manipulation. Spinal manipulation performed by a chiropractor may also help relieve the pain of spondylosis, especially with the first month of pain. It works by realigning vertebrae, which have been misaligned due to weakness in the spine brought on by spondylosis. Overall, it is a safe procedure.[23]
- The most common side effects are generally minor and include fatigue and temporary muscle soreness. Extremely rare complications of spinal manipulation may include weakness, loss of feeling in legs or arms, and bowel or bladder problems.
References
- ↑ http://www.spineuniverse.com/conditions/spondylosis/what-spondylosis
- ↑ http://www.emedicinehealth.com/spondylosis/article_em.htm
- ↑ http://www.spine-health.com/treatment/heat-therapy-cold-therapy/ice-packs-back-pain-relief
- ↑ http://www.spine-health.com/treatment/heat-therapy-cold-therapy/how-apply-heat-therapy
- ↑ http://www.spineuniverse.com/conditions/spondylosis/spondylosis-spinal-arthritis-reduce-back-neck-pain
- ↑ https://www.mayoclinic.org/diseases-conditions/cervical-spondylosis/diagnosis-treatment/drc-20370792
- ↑ http://www.mayoclinic.org/diseases-conditions/cervical-spondylosis/basics/definition/con-20027408
- ↑ http://www.emedicinehealth.com/spondylosis/article_em.htm
- ↑ http://www.spineuniverse.com/conditions/spondylosis/spondylosis-spinal-arthritis-reduce-back-neck-pain
- ↑ http://www.emedicinehealth.com/spondylosis/article_em.htm
- ↑ http://www.consumerreports.org/cro/2014/01/pain-relief-without-pills/index.htm
- ↑ http://www.mayoclinic.org/diseases-conditions/osteoarthritis/in-depth/pain-medications/art-20045899
- ↑ http://familydoctor.org/familydoctor/en/drugs-procedures-devices/prescription-medicines/prescription-nonsteroidal-anti-inflammatory-medicines.html
- ↑ https://www.urmc.rochester.edu/encyclopedia/content.aspx?contenttypeid=1&contentid=4709
- ↑ https://www.aafp.org/afp/2008/0801/p365.html
- ↑ https://www.nlm.nih.gov/medlineplus/ency/article/007489.htm
- ↑ http://www.aafp.org/afp/2005/0201/p483.html#afp20050201p483-t2
- ↑ http://www.spine-health.com/treatment/injections/lumbar-epidural-steroid-injections-low-back-pain-and-sciatica
- ↑ http://www.emedicinehealth.com/spondylosis/article_em.htm
- ↑ https://my.clevelandclinic.org/health/treatments_and_procedures/hic_Spinal_Decompression_Surgery
- ↑ http://www.spineuniverse.com/conditions/spondylosis/what-spondylosis
- ↑ http://www.emedicinehealth.com/spondylosis/article_em.htm
- ↑ https://nccih.nih.gov/health/pain/spinemanipulation.htm









-Step-9.webp)































































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...