Aprepitant
Aprepitant, sold under the brand name Emend among others, is a medication used to prevent chemotherapy-induced nausea and vomiting (CINV) and to prevent postoperative nausea and vomiting (PONV).[4] It may be used together with ondansetron and dexamethasone.[4] It is taken by mouth[4] or administered by intravenous injection.[3]
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Emend, Cinvanti, Aponvie |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a604003 |
| License data |
|
| Pregnancy category |
|
| Routes of administration | By mouth |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | 60–65% |
| Protein binding | >95% |
| Metabolism | Liver (mostly CYP3A4- mediated; some contributions by CYP2C19 & CYP1A2) |
| Elimination half-life | 9–13 hours |
| Excretion | Urine (57%), feces (45%) |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| ChEBI | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.202.762 |
| Chemical and physical data | |
| Formula | C23H21F7N4O3 |
| Molar mass | 534.435 g·mol−1 |
| 3D model (JSmol) | |
| |
| |
| (verify) | |
Common side effects include tiredness, loss of appetite, diarrhea, abdominal pain, hiccups, itchiness, pneumonia, and blood pressure changes.[4] Other severe side effects may include anaphylaxis.[4] While use in pregnancy does not appear to be harmful, such use has not been well studied.[5] Aprepitant belongs to the class of neurokinin-1 receptor antagonists medications.[4] It works by blocking substance P from attaching to the NK1 receptors.[6]
Aprepitant was approved for medical use in the European Union and the United States in 2003.[4][6] It is made by Merck & Co.[4] It is on the World Health Organization's List of Essential Medicines.[7][8]
Medical uses
Aprepitant is used to prevent chemotherapy-induced nausea and vomiting (CINV) and to prevent postoperative nausea and vomiting (PONV).[4] It may be used together with ondansetron and dexamethasone.[4]
Mechanism of action
Aprepitant is classified as an NK1 antagonist because it blocks signals given off by NK1 receptors. This, therefore, decreases the likelihood of vomiting in patients.
NK1 is a G protein-coupled receptor located in the central and peripheral nervous system. This receptor has a dominant ligand known as Substance P (SP). SP is a neuropeptide, composed of 11 amino acids, which sends impulses and messages from the brain. It is found in high concentrations in the vomiting center of the brain, and, when activated, it results in a vomiting reflex. In addition to this it also plays a key part in the transmission of pain impulses from the peripheral receptors to the central nervous system.
Aprepitant has been shown to inhibit both the acute and delayed emesis induced by cytotoxic chemotherapeutic drugs by blocking substance P landing on receptors in the brain's neurons. Positron emission tomography (PET) studies, have demonstrated that aprepitant can cross the blood brain barrier and bind to NK1 receptors in the human brain.[9] It has also been shown to increase the activity of the 5-HT3 receptor antagonists ondansetron and the corticosteroid dexamethasone, which are also used to prevent nausea and vomiting caused by chemotherapy.[10]
Pharmacokinetics
Before clinical testing, a new class of therapeutic agent has to be characterized in terms of preclinical metabolism and excretion studies. Average bioavailability is found to be around 60-65%. Aprepitant is metabolized primarily by CYP3A4 with minor metabolism by CYP1A2 and CYP2C19. Seven metabolites of aprepitant, which are only weakly active, have been identified in human plasma. As a moderate inhibitor of CYP3A4, aprepitant can increase plasma concentrations of co-administered medicinal products that are metabolized through CYP3A4. Specific interaction has been demonstrated with oxycodone, where aprepitant both increased the efficacy and worsened the side effects of oxycodone; however it is unclear whether this is due to CYP3A4 inhibition or through its NK-1 antagonist action.[11] Following IV administration of a 14C-labeled prodrug of aprepitant (L-758298), which is converted rapidly and completely to aprepitant, approximately 57% of the total radioactivity is excreted in the urine and 45% in feces. No unchanged substance is excreted in urine.[12]
Structure and properties
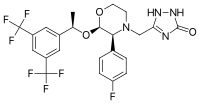
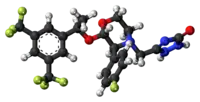
Aprepitant is made up of a morpholine core with two substituents attached to adjacent ring carbons. These substitute groups are trifluoromethylated 1-phenylethanol and fluorophenyl group. Aprepitant also has a third substituent (triazolinone), which is joined to the morpholine ring nitrogen. It has three chiral centres very close together, which combine to produce an amino acetal arrangement. Its empirical formula is C23H21F7N4O3.
Synthesis
Shortly after Merck initiated research into reducing the severity and likelihood of CINV, researchers discovered that aprepitant is effective in prevention. Researchers worked on coming up with a process to create aprepitant, and within a short period they came up with effective synthesis of the substance. This original synthesis was deemed to be workable and proved to be a crucial step in achieving commercialization; however, Merck decided that the process was not environmentally sustainable. This was due to the original synthesis requiring six steps, many of which needed dangerous chemicals such as sodium cyanide, dimethyltitanocene, and gaseous ammonia. In addition to this, for the process to be effective cryogenic temperatures were needed for some of the steps and other steps produced hazardous byproducts such as methane.[13] The environmental concerns of the synthesis of aprepitant became so great that Merck research team decided to withdraw the drug from clinical trials and attempt to create a different synthesis of aprepitant.[14]
The gamble of taking the drug out of clinical trials proved to be successful when shortly afterwards the team of Merck researchers came up with an alternative and more environmentally friendly synthesis of aprepitant. The new process works by four compounds of similar size and complexity being fused together. This therefore is a much simpler process and requires only three steps, half the number of the original synthesis.
The new process begins by enantiopure trifluoromethylated phenyl ethanol being joined to a racemic morpholine precursor. This results in the desired isomer crystallizing on the top of the solution and the unwanted isomer remaining in the solution. The unwanted isomer is then converted to the desired isomer through a crystallization-induced asymmetric transformation. By the end of this step a secondary amine, the base of the drug, is formed.
The second step involves the fluorophenyl group being attached to the morpholine ring. Once this has been achieved the third and final step can initiated. This step involved a side chain of triazolinone being added to the ring. Once this step has been successfully completed a stable molecule of aprepitant has been produced.[15]
This more streamlined route yields around 76% more aprepitant than the original process and reduces the operating cost by a significant amount. In addition, the new process also reduces the amount of solvent and reagents required by about 80% and saving an estimated 340,000L per ton of aprepitant produced.[14]
The improvements in the synthesis process have also decreased the long-term detriment to the natural environment associated with the original procedure, due to eliminating the use of several hazardous chemicals.
History
It was approved by the US Food and Drug Administration (FDA) in 2003.[16] In 2008, fosaprepitant, an intravenous form of aprepitant was approved in the United States.
Research
Major depression
Plans to develop aprepitant as an antidepressant have been withdrawn.[17] Subsequently, other trials with NK1 receptor antagonists, casopitant and orvepitant, have shown promising results.[18][19][20]
Beyond suggestions that PET receptor occupancy must not be used routinely to cap dosing for new medical indications for this class,[21] or that > 99% human receptor occupancy might be required for consistent psycho-pharmacological or other therapeutic effects,[20] critical scientific dissection and debate of the above data might be needed to enable aprepitant, and the class of NK1 antagonists as a whole, to fulfill preclinically predicted utilities beyond CINV (i.e., for other psychiatric disorders, addictions, neuropathic pain, migraine, osteoarthritis, overactive bladder, inflammatory bowel disease and other disorders with suspected inflammatory or immunological components. However, most data remain proprietary and thus reviews on the expanded clinical potential for drugs like aprepitant range from optimistic[22] to poor.[23]
Cannabinoid hyperemesis syndrome
Aprepitant has been identified as an extraordinarily effective rescue anti-emetic for hyperemesis[24] due to cannabinoid hyperemesis syndrome: nausea, severe cyclical vomiting, and cramping abdominal pain that can occur due to prolonged, high-dose cannabis use.
Standard first line anti-emetics such as Zofran and Compazine are often ineffective in cannabinoid hyperemesis syndrome.[25] and second-line treatments like haloperidol and droperidol have limited effectiveness, i.e., they may control vomiting while nausea remains in many patients. A Published case study reported 100% elimination of nausea and vomiting in a hospitalized patient who had previously not responded to ondansetron, metoclopramide, prochlorperazine, omeprazole, ranitidine, promethazine, and haloperidol.
Cannabinoid hyperemesis syndrome has two unusual features: Both 1) compulsive hot showering,[26] and/or 2) application of topical capsaicin cream[27] relieve nausea and vomiting in a large percentage of patients. Both capsaicin and hot showers are thought to work by modulating the TRPV1 receptor pathway, which in turn reduces the release of Substance P.[28][29] It would then follow that NK1 antagonists like aprepitant would also be effective via decreased Substance P activity.
References
- "Emend- aprepitant capsule Emend- aprepitant kit Emend- aprepitant powder, for suspension". DailyMed. 6 May 2022. Archived from the original on 9 March 2022. Retrieved 27 September 2022.
- "Cinvanti- aprepitant injection, emulsion". DailyMed. 24 March 2022. Archived from the original on 31 August 2022. Retrieved 27 September 2022.
- "APONVIETM (aprepitant) injectable emulsion, for intravenous use Initial U.S. Approval: 2003" (PDF). Archived (PDF) from the original on 28 September 2022. Retrieved 28 September 2022.
- "Aprepitant/Fosaprepitant Dimeglumine Monograph for Professionals". Drugs.com. Archived from the original on 13 August 2020. Retrieved 13 October 2019.
- "Aprepitant Use During Pregnancy". Drugs.com. Archived from the original on 28 October 2020. Retrieved 13 October 2019.
- "Emend". European Medicines Agency. 17 September 2018. Archived from the original on 12 November 2020. Retrieved 13 October 2019.
- World Health Organization (2019). World Health Organization model list of essential medicines: 21st list 2019. Geneva: World Health Organization. hdl:10665/325771. WHO/MVP/EMP/IAU/2019.06. License: CC BY-NC-SA 3.0 IGO.
- World Health Organization (2021). World Health Organization model list of essential medicines: 22nd list (2021). Geneva: World Health Organization. hdl:10665/345533. WHO/MHP/HPS/EML/2021.02.
- Bergström M, Hargreaves RJ, Burns HD, Goldberg MR, Sciberras D, Reines SA, et al. (May 2004). "Human positron emission tomography studies of brain neurokinin 1 receptor occupancy by aprepitant". Biological Psychiatry. 55 (10): 1007–1012. doi:10.1016/j.biopsych.2004.02.007. PMID 15121485. S2CID 21071199.
- Gralla RJ, de Wit R, Herrstedt J, Carides AD, Ianus J, Guoguang-Ma J, et al. (August 2005). "Antiemetic efficacy of the neurokinin-1 antagonist, aprepitant, plus a 5HT3 antagonist and a corticosteroid in patients receiving anthracyclines or cyclophosphamide in addition to high-dose cisplatin: analysis of combined data from two Phase III randomized clinical trials". Cancer. 104 (4): 864–868. doi:10.1002/cncr.21222. PMID 15973669. S2CID 24860776.
- Walsh SL, Heilig M, Nuzzo PA, Henderson P, Lofwall MR (March 2013). "Effects of the NK1 antagonist, aprepitant, on response to oral and intranasal oxycodone in prescription opioid abusers". Addiction Biology. 18 (2): 332–343. doi:10.1111/j.1369-1600.2011.00419.x. PMC 4354863. PMID 22260216.
- "FDA Advisory Committee Background Package" (PDF). Food and Drug Administration. Archived (PDF) from the original on 16 May 2017. Retrieved 16 December 2019.
- Hale JJ, Mills SG, MacCoss M, Finke PE, Cascieri MA, Sadowski S, et al. (November 1998). "Structural optimization affording 2-(R)-(1-(R)-3, 5-bis(trifluoromethyl)phenylethoxy)-3-(S)-(4-fluoro)phenyl-4- (3-oxo-1,2,4-triazol-5-yl)methylmorpholine, a potent, orally active, long-acting morpholine acetal human NK-1 receptor antagonist". Journal of Medicinal Chemistry. 41 (23): 4607–4614. doi:10.1021/jm980299k. PMID 9804700.
- Hargreaves R, Ferreira JC, Hughes D, Brands J, Hale J, Mattson B, Mills S (March 2011). "Development of aprepitant, the first neurokinin-1 receptor antagonist for the prevention of chemotherapy-induced nausea and vomiting". Annals of the New York Academy of Sciences. 1222 (1): 40–48. Bibcode:2011NYASA1222...40H. doi:10.1111/j.1749-6632.2011.05961.x. PMID 21434941. S2CID 21202644.
- Brands KM, Payack JF, Rosen JD, Nelson TD, Candelario A, Huffman MA, et al. (February 2003). "Efficient synthesis of NK(1) receptor antagonist aprepitant using a crystallization-induced diastereoselective transformation". Journal of the American Chemical Society. 125 (8): 2129–2135. doi:10.1021/ja027458g. PMID 12590540.
- "Drug Approval Package: Emend (Aprepitant) NDA #21-549". Archived from the original on 24 March 2017. Retrieved 19 April 2011.
- Rupniak NM, Kramer MS (December 2017). "NK1 receptor antagonists for depression: Why a validated concept was abandoned". Journal of Affective Disorders. 223: 121–125. doi:10.1016/j.jad.2017.07.042. PMID 28753469.
- Ratti E, Bellew K, Bettica P, Bryson H, Zamuner S, Archer G, et al. (December 2011). "Results from 2 randomized, double-blind, placebo-controlled studies of the novel NK1 receptor antagonist casopitant in patients with major depressive disorder". Journal of Clinical Psychopharmacology. 31 (6): 727–733. doi:10.1097/JCP.0b013e31823608ca. PMID 22020354. S2CID 24609826.
- Trist DG, Ratti E, Bye A (December 2013). "Why receptor reserve matters for neurokinin1 (NK1) receptor antagonists". Journal of Receptor and Signal Transduction Research. 33 (6): 333–337. doi:10.3109/10799893.2013.843194. PMID 24106886. S2CID 21799710.
- Ratti E, Bettica P, Alexander R, Archer G, Carpenter D, Evoniuk G, et al. (May 2013). "Full central neurokinin-1 receptor blockade is required for efficacy in depression: evidence from orvepitant clinical studies". Journal of Psychopharmacology. 27 (5): 424–434. doi:10.1177/0269881113480990. PMID 23539641. S2CID 6523822.
- Barrett JS, McGuire J, Vezina H, Spitsin S, Douglas SD (December 2013). "PET measurement of receptor occupancy as a tool to guide dose selection in neuropharmacology: are we asking the right questions?". Journal of Clinical Psychopharmacology. 33 (6): 725–728. doi:10.1097/JCP.0b013e3182a88654. PMID 24100788.
- Herpfer I, Lieb K (2005). "Substance P receptor antagonists in psychiatry: rationale for development and therapeutic potential". CNS Drugs. 19 (4): 275–293. doi:10.2165/00023210-200519040-00001. PMID 15813642. S2CID 25497814.
- Griebel G, Holsboer F (May 2012). "Neuropeptide receptor ligands as drugs for psychiatric diseases: the end of the beginning?". Nature Reviews. Drug Discovery. 11 (6): 462–478. doi:10.1038/nrd3702. PMID 22596253. S2CID 10721248. Archived from the original on 5 March 2021. Retrieved 1 July 2019.
- Parvataneni S, Varela L, Vemuri-Reddy SM, Maneval ML (June 2019). "Emerging Role of Aprepitant in Cannabis Hyperemesis Syndrome". Cureus. 11 (6): e4825. doi:10.7759/cureus.4825. PMC 6682377. PMID 31403013.
- Ruberto AJ, Sivilotti ML, Forrester S, Hall AK, Crawford FM, Day AG (June 2021). "Intravenous Haloperidol Versus Ondansetron for Cannabis Hyperemesis Syndrome (HaVOC): A Randomized, Controlled Trial". Annals of Emergency Medicine. 77 (6): 613–619. doi:10.1016/j.annemergmed.2020.08.021. PMID 33160719.
- Perisetti A, Gajendran M, Dasari CS, Bansal P, Aziz M, Inamdar S, et al. (2020). "Cannabis hyperemesis syndrome: an update on the pathophysiology and management". Annals of Gastroenterology. 33 (6): 571–578. doi:10.20524/aog.2020.0528. PMC 7599351. PMID 33162734.
- Lee A, Coralic Z (February 2022). "Use of Capsaicin Cream in Cannabinoid Hyperemesis Syndrome in Patients Presenting to the Emergency Department". The Annals of Pharmacotherapy. 56 (2): 151–154. doi:10.1177/10600280211018516. PMID 33998315.
- Sorensen CJ, DeSanto K, Borgelt L, Phillips KT, Monte AA (March 2017). "Cannabinoid Hyperemesis Syndrome: Diagnosis, Pathophysiology, and Treatment-a Systematic Review". Journal of Medical Toxicology. 13 (1): 71–87. doi:10.1007/s13181-016-0595-z. PMC 5330965. PMID 28000146.
- Galli JA, Sawaya RA, Friedenberg FK (December 2011). "Cannabinoid hyperemesis syndrome". Current Drug Abuse Reviews. 4 (4): 241–249. doi:10.2174/1874473711104040241. PMC 3576702. PMID 22150623.
External links
- "Aprepitant". Drug Information Portal. U.S. National Library of Medicine.