Global health
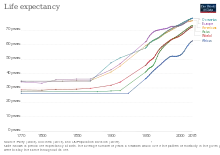
Global health is the health of the populations in the worldwide context;[1] it has been defined as "the area of study, research and practice that places a priority on improving health and achieving equity in health for all people worldwide".[2] Problems that transcend national borders or have a global political and economic impact are often emphasized.[3] Thus, global health is about worldwide health improvement (including mental health), reduction of disparities, and protection against global threats that disregard national borders.[4][5] Global health is not to be confused with international health, which is defined as the branch of public health focusing on developing nations and foreign aid efforts by industrialized countries.[6] Global health can be measured as a function of various global diseases and their prevalence in the world and threat to decrease life expectancy in the present day. Estimates suggest that in a pre-modern, poor world, life expectancy was around 30 years in all regions of the world.[7]

| Part of a series on |
| Public health |
|---|
 |
|
The predominant agency associated with global health (and international health) is the World Health Organization (WHO). Other important agencies impacting global health include UNICEF and World Food Programme (WFP). The United Nations system has also played a part with cross-sectoral actions to address global health and its underlying socioeconomic determinants with the declaration of the Millennium Development Goals[8] and the more recent Sustainable Development Goals.
Definition

Global health employs several perspectives that focus on the determinants and distribution of health in international contexts.
- Medicine describes the pathology of diseases and promotes prevention, diagnosis, and treatment.[9]
- Public health emphasizes the health of populations.[10]
- Epidemiology helps identify risk factors and causes of health problems.[11]
- Demography provides data for policy decisions.[12]<
- Economics emphasizes the cost-effectiveness and cost-benefit approaches for the optimal allocation of health resources.[13]
- Other social sciences such as sociology, development studies, psychology, anthropology, cultural studies, and law can help understand the determinants of health in societies.
Both individuals and organizations working in the domain of global health often face many questions regarding ethical and human rights. Critical examination of the various causes and justifications of health inequities is necessary for the success of proposed solutions. Such issues are discussed at the bi-annual Global Summits of National Ethics/Bioethics Councils.[14]
History
Global health as a discipline is widely acknwoledged to be of imperial origin and the need for its decolonisation has been widely recognised.[15][16][17] The global health ecosystem has also been mentioned to be have a feudal structure, acting for a small group of insitutions and individuals based in high-income countries which acts similar to an imperial "Crown".[18].
Important steps were taken towards global co-operation in health with the formation of the United Nations (UN) and the World Bank Group in 1945, after World War II. In 1948, the member states of the newly formed United Nations gathered to create the World Health Organization. A cholera epidemic that took 20,000 lives in Egypt in 1947 and 1948 helped spur the international community to action.[19] The WHO published its Model List of Essential Medicines, and the 1978 Alma Ata declaration underlined the importance of primary health care.[20]
At a United Nations Summit in 2000, member nations declared eight Millennium Development Goals (MDGs),[21] which reflected the major challenges facing human development globally, to be achieved by 2015.[22] The declaration was matched by unprecedented global investment by donor and recipient countries. According to the UN, these MDGs provided an important framework for development and significant progress has been made in a number of areas.[23] However, progress has been uneven and some of the MDGs were not fully realized including maternal, newborn and child health and reproductive health.[23] Building on the MDGs, a new Sustainable Development Agenda with 17 Sustainable Development Goals (SDGs) has been established for the years 2016–2030.[23] The first goal being an ambitious and historic pledge to end poverty.[24] On 25 September 2015, the 193 countries of the UN General Assembly adopted the 2030 Development Agenda titled Transforming our world: the 2030 Agenda for Sustainable Development.[24]
Several major initiatives began in the 2000s, including the vaccine alliance GAVI in 2000, The Global Fund to Fight AIDS, Tuberculosis and Malaria in 2002, U.S. President's Emergency Plan for AIDS Relief in 2003, the U.S. President's Malaria Initiative in 2005. In this decade and as part of the Monterrey Consensus, an increasing emphasis was put on measuring improvement in health outcomes, rather than merely the amount of money spent.[25]
In 2015 a book titled "To Save Humanity" was published, with nearly 100 essays regarding today's most pressing global health issues.[26] The essays were authored by global figures in politics, science, and advocacy ranging from Bill Clinton to Peter Piot, and addressed a wide range of issues including vaccinations, antimicrobial resistance, health coverage, tobacco use, research methodology, climate change, equity, access to medicine, and media coverage of health research.
Measures
Measures of global health include disability-adjusted life year (DALY), quality-adjusted life years (QALYs), and mortality rate.[27]
Disability-adjusted life years

The DALY is a summary measure that combines the impact of illness, disability, and mortality by measuring the time lived with disability and the time lost due to premature mortality. One DALY can be thought of as one lost year of "healthy" life. The DALY for a disease is the sum of the years of life lost due to premature mortality and the years lost due to disability for incident cases of the health condition.
Quality-adjusted life years
QALYs combine expected survival with expected quality of life into a single number: if an additional year of healthy life is worth a value of one (year), then a year of less healthy life is worth less than one (year). QALY calculations are based on measurements of the value that individuals place on expected years of survival. Measurements can be made in several ways: by techniques that replicate gambles about preferences for alternative states of health, with surveys or analyses that infer willingness to pay for alternative states of health, or through instruments that are based on trading off some or all likely survival time that a medical intervention might provide in order to gain less survival time of higher quality.[27]
Infant and child mortality
Infant mortality and child mortality for children under age 5 are more specific than DALYs or QALYs in representing the health in the poorest sections of a population, and are thus especially useful when focusing on health equity.[28] added section
Morbidity
Morbidity measures include incidence rate, prevalence, and cumulative incidence, with incidence rate referring to the risk of developing a new health condition within a specified period of time. Although sometimes loosely expressed simply as the number of new cases during a time period, morbidity is better expressed as a proportion or a rate.
Health topics
Respiratory tract infections
Infections of the respiratory tract and middle ear are major causes of morbidity and mortality worldwide.[29] Some respiratory infections of global significance include tuberculosis, measles, influenza, coronaviruses and pneumonias caused by Mycobacterium tuberculosis, Morbillivirus, Haemophilus influenzae and Pneumococci respectively. The spread of respiratory infections is exacerbated by crowded conditions, and poverty is associated with more than a 20-fold increase in the relative burden of lung infections.[30]
Diarrheal illnesses
Diarrhea is the second most common cause of child mortality worldwide, responsible for 17% of deaths of children under age 5.[31] Poor sanitation can increase transmission of bacteria and viruses through water, food, utensils, hands, and flies. Dehydration due to diarrhea can be effectively treated through oral rehydration therapy with dramatic reductions in mortality.[32][33] Important nutritional measures include the promotion of breastfeeding and zinc supplementation. While hygienic measures alone may be insufficient for the prevention of rotavirus diarrhea,[34] it can be prevented by a safe and potentially cost-effective vaccine.[35]
HIV/AIDS
The HIV/AIDS epidemic has highlighted the global nature of human health and welfare and globalization has given rise to a trend toward finding common solutions to global health challenges. Numerous international funds have been set up in recent times to address global health challenges such as HIV.[36] Since the beginning of the epidemic, more than 70 million people have been infected with the HIV virus and about 35 million people have died of HIV. Globally, 36.9 million [31.1–43.9 million] people were living with HIV at the end of 2017. An estimated 0.8% [0.6–0.9%] of adults aged 15–49 years worldwide are living with HIV, although the burden of the epidemic continues to vary considerably between countries and regions. The WHO African region remains most severely affected, with nearly 1 in every 25 adults (4.1%) living with HIV and accounting for nearly two-thirds of the people living with HIV worldwide.[37] Human immunodeficiency virus (HIV) is transmitted through unprotected sex, unclean needles, blood transfusions, and from mother to child during birth or lactation. Globally, HIV is primarily spread through sexual intercourse. The risk-per-exposure with vaginal sex in low-income countries from female to male is 0.38% and male to female is 0.3%.[38] The infection damages the immune system, leading to acquired immunodeficiency syndrome (AIDS) and eventually, death. Antiretroviral drugs prolong life and delay the onset of AIDS by minimizing the amount of HIV in the body.
Malaria
Malaria is a mosquito-borne infectious disease caused by the parasites of the genus Plasmodium. Symptoms may include fever, headaches, chills, muscle aches and nausea. Each year, there are approximately 500 million cases of malaria worldwide, most commonly among children and pregnant women in developing countries.[39] The WHO African Region carries a disproportionately high share of the global malaria burden. In 2016, the region was home to 90% of malaria cases and 91% of malaria deaths.[40] The use of insecticide-treated bed nets is a cost-effective way to reduce deaths from malaria, as is prompt artemisinin-based combination therapy, supported by intermittent preventive therapy in pregnancy. International travelers to endemic zones are advised chemoprophylaxis with antimalarial drugs like Atovaquone-proguanil, doxycycline, or mefloquine.[41] Global consumption and international trade in deforestation-associated commodities could also indirectly influence malaria risk. Many primary commodities cause deforestation and deforestation can increase malaria transmission. Consumption of such commodities in developed nations could increase malaria risk in developing nations.[42]
Neglected tropical diseases
More than one billion people were treated for at least one neglected tropical disease in 2015.[43] For instance, neglected tropical diseases are a diverse group of infectious diseases that are endemic in tropical and subtropical regions of 149 countries, primarily effecting low and middle income populations in Africa, Asia, and Latin America. They are variously caused by bacteria (Trachoma, Leprosy), viruses (Dengue,[44] Rabies), protozoa (Human African trypanosomiasis, Chagas), and helminths (Schistosomiasis, Onchocerciasis, Soil transmitted helminths).[45] The Global Burden of Disease Study concluded that neglected tropical diseases comprehensively contributed to approximately 26.06 million disability-adjusted life years in 2010, as well as significant deleterious economic effects.[46] In 2011, the World Health Organization launched a 2020 Roadmap for neglected tropical diseases, aiming for the control or elimination of 10 common diseases.[47] The 2012 London Declaration builds on this initiative, and called on endemic countries and the international community to improve access to clean water and basic sanitation, improved living conditions, vector control, and health education, to reach the 2020 goals.[48] In 2017, a WHO report cited 'unprecedented progress' against neglected tropical diseases since 2007, especially due to mass drug administration of drugs donated by pharmaceutical companies.[49]
Maternal health
Complications of pregnancy and childbirth are the leading causes of death among women of reproductive age. In many developing countries, a woman dies from complications from childbirth approximately every minute.[50] According to the World Health Organization's 2005 World Health Report, poor maternal conditions are the fourth leading cause of death for women worldwide, after HIV/AIDS, malaria, and tuberculosis.[51] Most maternal deaths and injuries can be prevented, and such deaths have been largely eradicated in the developed world.[52] Targets for improving maternal health include increasing and assisting the number of deliveries accompanied by skilled birth attendants.[53] 68 low-income countries tracked by the WHO- and UNICEF-led collaboration Countdown to 2015 are estimated to hold for 97% of worldwide maternal and child deaths.[54]
Nutrition
In 2010, about 104 million children were underweight, and undernutrition contributes to about one third of child deaths around the world.[55] (Undernutrition is not to be confused with malnutrition, which refers to poor proportion of food intake and can thus refer to obesity.)[56] Undernutrition impairs the immune system, increasing the frequency, severity, and duration of infections (including measles, pneumonia, and diarrhea). Infection can further contribute to malnutrition.[57] Deficiencies of micronutrient, such as vitamin A, iron, iodine, and zinc, are common worldwide and can compromise intellectual potential, growth, development, and adult productivity.[58][59][60][61][62][63] Interventions to prevent malnutrition include micronutrient supplementation, fortification of basic grocery foods, dietary diversification, hygienic measures to reduce spread of infections, and the promotion of breastfeeding.
Non-communicable diseases
Approximately 80% of deaths linked to non-communicable diseases occur in developing countries.[64] For instance, urbanization and aging have led to increasing poor health conditions related to non-communicable diseases in India. The fastest-growing causes of disease burden over the last 26 years were diabetes (rate increased by 80%) and ischemic heart disease (up 34%). More than 60% of deaths, about 6.1 million, in 2016 were due to NCDs, up from about 38% in 1990.[65] Increases in refugee urbanization, has led to a growing number of people diagnosed with chronic non-communicable diseases.[66]
In September 2011, the United Nations is hosting its first General Assembly Special Summit on the issue of non-communicable diseases.[67] Noting that non-communicable diseases are the cause of some 35 million deaths each year, the international community is being increasingly called to take measures for the prevention and control of chronic diseases and mitigate their impacts on the world population, especially on women, who are usually the primary caregivers.
For example, the rate of type 2 diabetes, associated with obesity, has been on the rise in countries previously troubled by hunger. In low-income countries, the number of individuals with diabetes is expected to increase from 84 million to 228 million by 2030.[68] Obesity, a preventable condition, is associated with numerous chronic diseases, including cardiovascular conditions, stroke, certain cancers, and respiratory disease. About 16% of the global burden of disease, measured as DALYs, has been accounted for by obesity.[68]
Violence against women
Violence against women has been defined as: "physical, sexual and psychological violence occurring in the family and in the general community, including battering, sexual abuse, dowry-related violence, rape, female genital mutilation and other traditional practices harmful to women, non-spousal violence and violence related to exploitation, sexual harassment and intimidation at work, in educational institutions and elsewhere, trafficking in women, forced prostitution and violence perpetrated or condoned by the state."[69] In addition to causing injury, violence may increase "women's long-term risk of a number of other health problems, including chronic pain, physical disability, drug and alcohol abuse, and depression".[70] The WHO Report on global and regional estimates on violence against women found that partner abuse causes women to have 16% more chances of suffering miscarriages, 41% more occurrences of pre-term birth babies and twice the likeliness of having abortions and acquiring HIV or other STDs[71]
Although statistics can be difficult to obtain as many cases go unreported, it is estimated that one in every five women faces some form of violence during her lifetime, in some cases leading to serious injury or even death.[72] Risk factors for being an offender include low education, past exposure to child maltreatment or witnessing violence between parents, harmful use of alcohol, attitudes accepting of violence, and gender inequality.[73] Equality of women has been addressed in the Millennium development goals. Now, Gender Equality is Sustainable Development Goal 5. Preventing the violence against women needs to form an essential part of the public health reforms in the form of advocation and evidence gathering. Primary prevention in the form of raising women economic empowerment facilities, microfinance and skills training social projects related to gender equality should be conducted.
Activities promoting relationship and communication skills among couples, reducing alcohol access and altering societal ideologies should be organized. Childhood interventions, community and school-based education, raising media-oriented awareness and other approaches should be carried out to challenge social norms and stereotypical thought processes to promote behavioral change among men and raise gender equality. Trained health care providers would play a vital role in secondary and tertiary prevention of abuse by performing early identification of women suffering from violence and contributing to the addressing of their health and psychological needs. They could be highly important in prevention of the recurrence of violence and the mitigation of its effects on the health of the abused women and their children.[74] The Member States of the World Health Assembly endorsed a plan in 2016 for reinforcing the health system's role in addressing the global phenomenon of violence against women and girls and working towards their health and protection.[75]
Global surgery
Halfdan T. Mahler, the 3rd Director-General of the World Health Organization (WHO), first brought attention to the disparities in surgery and surgical care when he stated, "‘the vast majority of the world’s population has no access whatsoever to skilled surgical care and little is being done to find a solution,".[76]
While significant progresses have been made in fields within global health such as infectious diseases, maternal and child health, and even other non-communicable diseases over the past several decades, the provision of surgery and surgical care in resource-limited settings have largely remained unmet with about 5 billion people lacking access to safe and affordable surgical and anesthesia care.[77] This is especially true in the poorest countries, which account for over one-third of the population but only 3.5% of all surgeries that occur worldwide.[78] In fact, it has been estimated that up to 30% of the total global burden of disease (GBD) could be attributable to surgical conditions, which include a mix of injuries, malignancies, congenital anomalies, and complications of pregnancy.[79][80] As a result, global surgery has become an emerging field within global health as 'the multidisciplinary enterprise of providing improved and equitable surgical care to the world's population, with its core belief as the issues of need, access and quality' and has often been described as the 'neglected stepchild of global health,' a term coined by Dr. Paul Farmer to highlight the urgent need for further work in this area.[81][82] Furthermore, Jim Young Kim, the former President of the World Bank, proclaimed in 2014 that “surgery is an indivisible, indispensable part of health care and of progress towards universal health coverage."[83]
In 2015, the Lancet Commission on Global Surgery (LCoGS) published the landmark report titled "Global Surgery 2030: evidence and solutions for achieving health, welfare, and economic development," describing the large, pre-existing burden of surgical diseases in low- and middle-income countries (LMICs) and future directions for increasing universal access to safe surgery by the year 2030.[77] The Commission highlighted that 143 million additional procedures were needed every year to prevent further morbidity and mortality from treatable surgical conditions as well as a $12.3 trillion loss in economic productivity by the year 2030.[77] It emphasized the need to significantly improve the capacity for Bellwether procedures – laparotomy, caesarean section, open fracture care – which are considered a minimum level of care that first-level hospitals should be able to provide in order to capture the most basic emergency surgical care.[77][84] In order to address these challenges and track progress, the Commission defined the following core indicators for assessing access to safe and affordable surgical d anesthesia care:[77]
| Core Indicators | Definition | Target |
|---|---|---|
| Access to timely essential surgery | The proportion of the population that can access, within 2 hours, a facility that can do cesarean delivery, laparotomy, and treatment of open fracture (the Bellwether Procedures) | A minimum of 80% coverage of essential surgical and anesthesia services per country by 2030 |
| Specialist surgical workforce density | The number of specialist surgical, anaesthetic, and obstetric physicians who are working, per 100,000 population | 100% of countries with at least 20 surgical, anaesthetic, and obstetric physicians per 100, 000 population by 2030 |
| Surgical volume | The number of procedures done in an operating theatre, per 100,000 population per year | 80% of countries by 2020 and 100% of countries by 2030 tracking surgical volume; a minimum of 5000 procedures per 100,000 population by 2030 |
| Perioperative mortality | All-cause death rate before discharge in patients who have undergone a procedure in an operating theatre, divided by the total number of procedures, presented as a percentage | 80% of countries by 2020 and 100% of countries by 2030 tracking perioperative mortality; in 2020, assess global data and set national targets for 2030 |
| Protection against impoverishing expenditure | The proportion of households protected against impoverishment from direct out-of-pocket payments for surgical and anesthesia care | 100% protection against impoverishment from out-of-pocket payments for surgical and anaesthesia care by 2030 |
| Protection against catastrophic expenditure | The proportion of households protected against catastrophic expenditure from direct out-of-pocket payments for surgical and anesthesia care | 100% protection against catastrophic expenditure from out-of-pocket payments for surgical and anaesthesia care by 2030 |
Meeting these goals by the year 2030 would require increases in anesthetists, obstetricians, surgeons, nurses, and facilities with operating rooms as well as pre- and post-surgical care capacities.
Data from WHO and the World Bank indicate that scaling up infrastructure to enable access to surgical care in regions where it is currently limited or is non-existent is a low-cost measure relative to the significant morbidity and mortality caused by lack of surgical treatment.[79] In fact, a systematic review found that the cost-effectiveness ratio – dollars spent per DALYs averted – for surgical interventions is on par or exceeds those of major public health interventions such as oral rehydration therapy, breastfeeding promotion, and even HIV/AIDS antiretroviral therapy.[85] This finding challenged the common misconception that surgical care is financially prohibitive endeavor not worth pursuing in LMICs.
In terms of the financial impact on the patients, the lack of adequate surgical and anesthesia care has resulted in 33 million individuals every year facing catastrophic health expenditure – the out-of-pocket healthcare cost exceeding 40% of a given household's income.[77][86]
In alignment with the LCoGS call for action, the World Health Assembly adopted the resolution WHA68.15 in 2015 that stated, "Strengthening emergency and essential surgical care and anesthesia as a component of universal health coverage."[87] This not only mandated the WHO to prioritize strengthening the surgical and anesthesia care globally, but also led to governments of the member states recognizing the urgent need for increasing capacity in surgery and anesthesia. Additionally, the third edition of Disease Control Priorities (DCP3), published in 2015 by the World Bank, declared surgery as essential and featured an entire volume dedicated to building surgical capacity.[88]
A key policy framework that arose from this renewed global commitment towards surgical care worldwide is the National Surgical Obstetric and Anesthesia Plan (NSOAP).[89] NSOAP focuses on policy-to-action capacity building for surgical care with tangible steps as follows: (1) analysis of baseline indicators, (2) partnership with local champions, (3) broad stakeholder engagement, (4) consensus building and synthesis of ideas, (5) language refinement, (6) costing, (7) dissemination, and (8) implementation. This approach has been widely adopted and has served as guiding principles between international collaborators and local institutions and governments. Successful implementations have allowed for sustainability in terms of longterm monitoring, quality improvement, and continued political and financial support.[89]
Health interventions
Global interventions for improved child health and survival include the promotion of breastfeeding, zinc supplementation, vitamin A fortification, salt iodization, hygiene interventions such as hand-washing, vaccinations, and treatments of severe acute malnutrition.[53][90][91] The Global Health Council suggests a list of 32 treatments and health interventions that could potentially save several million lives each year.[92]
Many populations face an "outcome gap", which refers to the gap between members of a population who have access to medical treatment versus those who do not. Countries facing outcome gaps lack sustainable infrastructure.[93] In Guatemala, a subset of the public sector, the Programa de Accessibilidad a los Medicamentos ("Program for Access to Medicines"), had the lowest average availability (25%) compared to the private sector (35%). In the private sector, highest- and lowest-priced medicines were 22.7 and 10.7 times more expensive than international reference prices respectively. Treatments were generally unaffordable, costing as much as 15 days wages for a course of the antibiotic ceftriaxone.[94] The public sector in Pakistan, while having access to medicines at a lower price than international reference prices, has a chronic shortage of and lack of access to basic medicines.[95]
Journalist Laurie Garrett argues that the field of global health is not plagued by a lack of funds, but that more funds do not always translate into positive outcomes. The problem lies in the way these funds are allocated, as they are often disproportionately allocated to alleviating a single disease.[96]
In its 2006 World Health Report, the WHO estimated a shortage of almost 4.3 million doctors, midwives, nurses, and support workers worldwide, especially in sub-Saharan Africa.[97]
Global health security
The COVID-19 pandemic has highlighted how global health security is reliant on all countries around the world, including low- and middle-income countries, having strong health systems and at least a minimum of health research capacities. In an article 2020 in Annals of Global Health,[98] the ESSENCE group outlined a mechanism for review of investment in health research capacity building in low- and middle-income countries. The review mechanism will give funders of research for health the information to identify the gaps in capacity that exist in low- and middle-income countries and the opportunity to work together to address those disparities. The overall goal is increased, coordinated support of research on national health priorities as well as improved pandemic preparedness in LMICs, and, eventually, fewer countries with very limited health research capacity.
Organization
Governmental or inter-governmental organizations focused on global health include:
- The United Nations
- World Health Organization
- United Nations Children's Fund (UNICEF)
- World Food Programme (WFP)
- Pan American Health Organization (PAHO)
- International Committee of the Red Cross
- Centers for Disease Control and Prevention (CDC)
- The Global Fund to Fight AIDS, Tuberculosis and Malaria
Non-governmental organizations focused on global health include:
- Médecins Sans Frontières (Doctors Without Borders, MSF)
- Bill & Melinda Gates Foundation
Global Health Security Agenda
The Global Health Security Agenda (GHSA) is "a multilateral, multi-sector effort that includes 60 participating countries and numerous private and public international organizations focused on building up worldwide health security capabilities toward meeting such threats" as the spread of infectious disease. On March 26–28, 2018, the GHSA held a high-level meeting in Tbilisi, Georgia, on biosurveillance of infectious disease threats, "which include such modern-day examples as HIV/AIDS, severe acute respiratory syndrome (SARS), H1N1 influenza, multi-drug resistant tuberculosis — any emerging or reemerging disease that threatens human health and global economic stability."[99] This event brought together GHSA partner countries, contributing countries of Real-Time Surveillance Action Package, and international partner organizations supporting the strengthening of capacities to detect infectious disease threats within the Real-Time Surveillance Action Package and other cross-cutting packages.[100]
GHSA works through four main mechanisms of member action, action packages, task forces and international cooperation. In 2015, the Steering Group of the GHSA agreed upon the implementation of their commitments through 11 Action Packages. Action Packages are a commitment by member countries and their partners to work collaboratively towards development and implementation of International Health Regulations (IHR).[101] Action packages are based on GHSA's aim to strengthen national and international capacity to prevent, detect, and respond to infectious disease threats. Each action package consists of five-year targets, measures of progress, desired impacts, country commitments, and list of baseline assessments.[102] The Joint External Evaluation process, derived as part of the IHR Monitoring and Evaluation Framework is an assessment of a country's capacity for responding to public health threats.[101] So far, G7 partners and EU have made a collective commitment to assist 76 countries whereas the US committed to helping 32 countries to achieve GHSA targets for IHR implementation. In September 2014, a pilot tool was developed to measure progress of the Action Packages and applied in countries (Georgia, Peru, Uganda, Portugal, the United Kingdom, and Ukraine) that volunteered to participate in an external assessment.[103]
See also
- Global mental health
- Global Strategy for Women's and Children's Health
- Health system
- Pandemic prevention
- Planetary health
- Public health
- Social determinants of health
- Universal health care
- Migrant health
- Child health and nutrition in Africa
- CAB Direct – Global Health database
- Global neurosurgery
References
- Brown TM, Cueto M, Fee E (January 2006). "The World Health Organization and the transition from "international" to "global" public health". American Journal of Public Health. 96 (1): 62–72. doi:10.2105/AJPH.2004.050831. PMC 1470434. PMID 16322464.
- Koplan JP, Bond TC, Merson MH, Reddy KS, Rodriguez MH, Sewankambo NK, Wasserheit JN (June 2009). "Towards a common definition of global health". Lancet. 373 (9679): 1993–1995. CiteSeerX 10.1.1.610.7968. doi:10.1016/S0140-6736(09)60332-9. PMID 19493564. S2CID 6919716.
- Global Health Initiative (2008). Why Global Health Matters. Washington, DC: FamiliesUSA. Archived from the original on 2011-03-08. Retrieved 2008-06-10.
- Macfarlane SB, Jacobs M, Kaaya EE (December 2008). "In the name of global health: trends in academic institutions". Journal of Public Health Policy. 29 (4): 383–401. doi:10.1057/jphp.2008.25. PMID 19079297. S2CID 46424271.
- Fischer SE, Patil P, Zielinski C, Baxter L, Bonilla-Escobar FJ, Hussain S, et al. (May 2020). "Is it about the 'where' or the 'how'? Comment on Defining global health as public health somewhere else". BMJ Global Health. 5 (5): e002567. doi:10.1136/bmjgh-2020-002567. PMC 7223010. PMID 32381654.
- White F, Nanan DJ (2008). "International and Global Health". In Wallace RB (ed.). Maxcy-Rosenau-Last Public Health and Preventive Medicine (15th ed.). McGraw Hill. pp. 1252–8. ISBN 978-0-07-144198-8.
- Roser M, Ortiz-Ospina E, Ritchie H (2013-05-23). "Life Expectancy". Our World in Data.
- "Millennium Development Goals". United Nations. Retrieved 2013-03-15.
- Weatherall DJ, Clegg JB (2001). "Inherited haemoglobin disorders: an increasing global health problem". Bulletin of the World Health Organization. 79 (8): 704–712. PMC 2566499. PMID 11545326.
- Fried LP, Bentley ME, Buekens P, Burke DS, Frenk JJ, Klag MJ, Spencer HC (February 2010). "Global health is public health". Lancet. 375 (9714): 535–537. doi:10.1016/s0140-6736(10)60203-6. PMID 20159277. S2CID 38796542.
- Ahern M, Kovats RS, Wilkinson P, Few R, Matthies F (2005). "Global health impacts of floods: epidemiologic evidence". Epidemiologic Reviews. 27 (1): 36–46. doi:10.1093/epirev/mxi004. PMID 15958425.
- Verano JW, Ubelake DH (1992). Disease and demography in the Americas. Washington: Smithsonian Institution Press. ISBN 978-1-56098-163-3.
- Bloom DE, Cafiero E, Jané-Llopis E, Abrahams-Gessel S, Bloom LR, Fathima S, et al. (January 2012). The global economic burden of noncommunicable diseases. Program on the Global Demography of Aging (Report).
- "Global Summits of National Ethics/Bioethics Councils". Berlin. 2016. Archived from the original on 4 April 2019.
- Kwete X, Tang K, Chen L, Ren R, Chen Q, Wu Z, et al. (January 2022). "Decolonizing global health: what should be the target of this movement and where does it lead us?". Global Health Research and Policy. 7 (1): 3. doi:10.1186/s41256-022-00237-3. PMC 8784247. PMID 35067229.
- Rasheed MA (December 2021). "Navigating the violent process of decolonisation in global health research: a guideline". The Lancet. Global Health. 9 (12): e1640–e1641. doi:10.1016/S2214-109X(21)00440-X. PMID 34798014. S2CID 244286291.
- Affun-Adegbulu C, Adegbulu O (August 2020). "Decolonising Global (Public) Health: from Western universalism to Global pluriversalities". BMJ Global Health. 5 (8): e002947. doi:10.1136/bmjgh-2020-002947. PMC 7443258. PMID 32819916. S2CID 221220715.
- Keshri VR, Bhaumik S (September 2022). "The feudal structure of global health and its implications for decolonisation". BMJ Global Health. 7 (9): e010603. doi:10.1136/bmjgh-2022-010603. PMC 9516156. PMID 36167407. S2CID 252565623.
- World Health Organization. "History of WHO". Archived from the original on 2006-12-07.
- Primary Health Care: Report of the International Conference on Primary Health Care (PDF) (Report). Geneva: World Health Organization. 1978. Archived from the original (PDF) on 2017-08-29. Retrieved 2014-05-06.
- Kumar S, Kumar N, Vivekadhish S (January–March 2016). "Millennium Development Goals (MDGs) to Sustainable Development Goals (SDGs): Addressing Unfinished Agenda and Strengthening Sustainable Development and Partnership". Indian Journal of Community Medicine. 41 (1): 1–4. doi:10.4103/0970-0218.170955. PMC 4746946. PMID 26917865.
- "Resolution adopted by the General Assembly, 55/2" (PDF). United Nations. 18 September 2000.
- "Transforming our world: the 2030 Agenda for Sustainable Development .:. Sustainable Development Knowledge Platform". sustainabledevelopment.un.org. Retrieved 2016-02-26.
- "Sustainable Development Goals". UNDP. Archived from the original on 2016-03-04. Retrieved 2016-02-26.
- Mark Dybul M (Summer 2017). "How HIV, SARS, and Ebola Put Global Health on the Agenda". The Catalyst. George W. Bush Institute.
- Hoffman SJ (October 2011). "Ending medical complicity in state-sponsored torture". Lancet. 378 (9802): 1535–1537. doi:10.1016/S0140-6736(11)60816-7. PMID 21944647. S2CID 45829194.
- Etches V, Frank J, Di Ruggiero E, Manuel D (2006). "Measuring population health: a review of indicators". Annual Review of Public Health. 27: 29–55. doi:10.1146/annurev.publhealth.27.021405.102141. PMID 16533108.
- Mulholland E, Smith L, Carneiro I, Becher H, Lehmann D (May 2008). "Equity and child-survival strategies". Bulletin of the World Health Organization. 86 (5): 399–407. doi:10.2471/BLT.07.044545. PMC 2647438. PMID 18545743.
- Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJ (May 2006). "Global and regional burden of disease and risk factors, 2001: systematic analysis of population health data". Lancet. 367 (9524): 1747–1757. doi:10.1016/S0140-6736(06)68770-9. PMID 16731270. S2CID 22609505.
- Mizgerd JP (February 2006). "Lung infection--a public health priority". PLOS Medicine. 3 (2): e76. doi:10.1371/journal.pmed.0030076. PMC 1326257. PMID 16401173.
- "Statistics by Area – Diarrhoeal disease – The challenge". UNICEF. Retrieved 2013-01-12.
- Taylor CE, Greenough WB (1989). "Control of diarrheal diseases". Annual Review of Public Health. 10: 221–244. doi:10.1146/annurev.pu.10.050189.001253. PMID 2655632.
- Victora CG, Bryce J, Fontaine O, Monasch R (2000). "Reducing deaths from diarrhoea through oral rehydration therapy". Bulletin of the World Health Organization. 78 (10): 1246–1255. PMC 2560623. PMID 11100619.
- "Rotavirus Vaccine Access and Delivery – PATH" (PDF). Rotavirusvaccine.org. 2011-12-07. Archived from the original (PDF) on 2009-12-22. Retrieved 2013-01-12.
- Valencia-Mendoza A, Bertozzi SM, Gutierrez JP, Itzler R (July 2008). "Cost-effectiveness of introducing a rotavirus vaccine in developing countries: the case of Mexico". BMC Infectious Diseases. 8: 103. doi:10.1186/1471-2334-8-103. PMC 2527317. PMID 18664280.
- Coovadia HM, Hadingham J (August 2005). "HIV/AIDS: global trends, global funds and delivery bottlenecks". Globalization and Health. 1: 13. doi:10.1186/1744-8603-1-13. PMC 1199613. PMID 16060961.
- "HIV/AIDS". World Health Organization. Retrieved 2018-11-01.
- "Estimated HIV transmission risk per exposure for specific activities and events".
- Birn A, Pillay Y, Holtz T (2009). Textbook of International Health (3rd ed.). Oxford University Press. p. 273. ISBN 978-0-19-971985-3.
- "Malaria key facts".
- "CDC – Malaria – Travelers – Malaria Information and Prophylaxis, by Country". U.S. Centers for Disease Control and Prevention. 2018-01-26. Retrieved 2018-11-01.
- Chaves LS, Fry J, Malik A, Geschke A, Sallum MA, Lenzen M (March 2020). "Global consumption and international trade in deforestation-associated commodities could influence malaria risk". Nature Communications. 11 (1): 1258. Bibcode:2020NatCo..11.1258C. doi:10.1038/s41467-020-14954-1. PMC 7062889. PMID 32152272.
- "Unprecedented progress against neglected tropical diseases, WHO reports". World Health Organization. 2017. Retrieved 2017-05-11.
- Horstick O, Tozan Y, Wilder-Smith A (April 2015). "Reviewing dengue: still a neglected tropical disease?". PLOS Neglected Tropical Diseases. 9 (4): e0003632. doi:10.1371/journal.pntd.0003632. PMC 4415787. PMID 25928673.
- "CDC – Neglected Tropical Diseases – Diseases". www.cdc.gov. Retrieved 2017-05-11.
- Hotez PJ, Alvarado M, Basáñez MG, Bolliger I, Bourne R, Boussinesq M, et al. (July 2014). "The global burden of disease study 2010: interpretation and implications for the neglected tropical diseases". PLOS Neglected Tropical Diseases. 8 (7): e2865. doi:10.1371/journal.pntd.0002865. PMC 4109880. PMID 25058013.
- World Health Organization (2013). Sustaining the drive to overcome the global impact of neglected tropical diseases: second WHO report on neglected tropical diseases; summary (PDF).
- London Declaration on Neglected Tropical Diseases (PDF). 2012.
- World Health Organization (2017). Integrating Neglected Tropical Diseases into Global Health and Development (PDF).
- "Improve Maternal Health". UNICEF.
- "World Health Report 2005: make every mother and child count". Geneva: World Health Organization. 2005. Archived from the original on April 9, 2005.
- "Most Maternal Deaths in Sub-Saharan Africa Could Be Avoided". Science Daily. 2 March 2010. Retrieved 3 March 2011.
- Bhutta ZA, Ahmed T, Black RE, Cousens S, Dewey K, Giugliani E, et al. (February 2008). "What works? Interventions for maternal and child undernutrition and survival". Lancet. 371 (9610): 417–440. doi:10.1016/S0140-6736(07)61693-6. PMID 18206226. S2CID 18345055.
- "Progress reports". Countdown to 2015. Archived from the original on 2011-07-25. Retrieved 2011-03-15.
- "Challenges". Nutrition. World Health Organization. Archived from the original on March 21, 2006.
- Shetty P (2003). "Malnutrition and Undernutrition". Medicine. Nutrition. 31 (4): 18–22. doi:10.1383/medc.31.4.18.27958. ISSN 1357-3039.
Malnutrition refers to all deviations from adequate and optimal nutritional status, including energy undernutrition and over-nutrition (obesity is a form of malnutrition). The term 'undernutrition' is used to refer to generally poor nutritional status, but also implies underfeeding
- Schaible UE, Kaufmann SH (May 2007). "Malnutrition and infection: complex mechanisms and global impacts". PLOS Medicine. 4 (5): e115. doi:10.1371/journal.pmed.0040115. PMC 1858706. PMID 17472433.
- "Vitamin A supplementation". World Health Organization. Archived from the original on 2013-01-25.
- Lynch S, Stoltzfus R, Rawat R (December 2007). "Critical review of strategies to prevent and control iron deficiency in children". Food and Nutrition Bulletin. 28 (4 Suppl): S610–S620. doi:10.1177/15648265070284S413. PMID 18297898.
- Walker SP, Wachs TD, Gardner JM, Lozoff B, Wasserman GA, Pollitt E, Carter JA (January 2007). "Child development: risk factors for adverse outcomes in developing countries". Lancet. 369 (9556): 145–157. doi:10.1016/S0140-6736(07)60076-2. PMID 17223478. S2CID 11120228.
- Lazzerini M (October 2007). "Effect of zinc supplementation on child mortality". Lancet. 370 (9594): 1194–1195. doi:10.1016/S0140-6736(07)61524-4. PMID 17920908. S2CID 33297518.
- Fischer Walker CL, Ezzati M, Black RE (May 2009). "Global and regional child mortality and burden of disease attributable to zinc deficiency". European Journal of Clinical Nutrition. 63 (5): 591–597. doi:10.1038/ejcn.2008.9. PMID 18270521.
- Lazzerini M, Wanzira H (December 2016). "Oral zinc for treating diarrhoea in children". The Cochrane Database of Systematic Reviews. 12 (4): CD005436. doi:10.1002/14651858.CD005436.pub5. PMC 5450879. PMID 27996088.
- "WHO: Global Status Report on Noncommunicable Diseases 2010". 2011. Archived from the original on April 30, 2011.
- "Comprehensive health study in India finds rise of non-communicable diseases". 2017-11-13.
- Amara AH, Aljunid SM (April 2014). "Noncommunicable diseases among urban refugees and asylum-seekers in developing countries: a neglected health care need". Globalization and Health. 10: 24. doi:10.1186/1744-8603-10-24. PMC 3978000. PMID 24708876.
- "Press Conference on General Assembly Decision to Convene Summit in September 2011 on Non-Communicable Diseases". New York: United Nations. 13 May 2010.
- Hossain P, Kawar B, El Nahas M (January 2007). "Obesity and diabetes in the developing world--a growing challenge". The New England Journal of Medicine. 356 (3): 213–215. doi:10.1056/NEJMp068177. PMID 17229948.
- "Violence Against Women Fact Sheet". The United Nations Population Fund. 2005. Archived from the original on 2012-09-08. Retrieved 2012-09-29.
- Ellsberg M, and Heise L. Researching Violence Against Women: A Practical Guide for Researchers and Activists. Washington DC, United States: World Health Organization, PATH; 2005. Accessed September 19, 2012.
- Global and regional estimates of violence against women: prevalence and health effects of intimate partner violence and non-partner sexual violence. WHO. 2013. hdl:10665/85239. ISBN 978-9-24-156462-5.
- Addressing violence against women and achieving the Millennium Development Goals. World Health Organization (Report). Geneva, Switzerland. September 2005.
- "Violence against women: Intimate partner and sexual violence against women fact sheet". World Health Organization. 2011.
- Cockerham WC, Quah SR, eds. (2017). International Encyclopedia of Public Health (Second ed.). Elsevier/AP. ISBN 978-0-12-803708-9.
- WHO. "The World Health Assembly endorses the global plan of action on violence against women and girls, and also against children". WHO.int. Retrieved 1 December 2019.
- Mahler H. Address by Dr. H. Mahler, Director General of the World Health Organization, in presenting his report for 1986 and 1987. Forty-first World Health Assembly: world health-2000 and beyond. (Report). JSTOR 41989284.
- Meara JG, Leather AJ, Hagander L, Alkire BC, Alonso N, Ameh EA, et al. (August 2015). "Global Surgery 2030: evidence and solutions for achieving health, welfare, and economic development". Lancet. 386 (9993): 569–624. doi:10.1016/S0140-6736(15)60160-X. PMID 25924834. S2CID 2048403.
- Weiser TG, Regenbogen SE, Thompson KD, Haynes AB, Lipsitz SR, Berry WR, Gawande AA (July 2008). "An estimation of the global volume of surgery: a modelling strategy based on available data". Lancet. 372 (9633): 139–144. doi:10.1016/S0140-6736(08)60878-8. PMID 18582931. S2CID 17918156.
- McQueen KA, Ozgediz D, Riviello R, Hsia RY, Jayaraman S, Sullivan SR, Meara JG (June 2010). "Essential surgery: Integral to the right to health". Health and Human Rights. 12 (1): 137–152. PMID 20930260.
- Shrime MG, Bickler SW, Alkire BC, Mock C (April 2015). "Global burden of surgical disease: an estimation from the provider perspective". The Lancet. Global Health. 3 (Suppl 2): S8–S9. doi:10.1016/S2214-109X(14)70384-5. PMID 25926322.
- Bath M, Bashford T, Fitzgerald JE (2019). "What is 'global surgery'? Defining the multidisciplinary interface between surgery, anaesthesia and public health". BMJ Global Health. 4 (5): e001808. doi:10.1136/bmjgh-2019-001808. PMC 6830053. PMID 31749997.
- Farmer PE, Kim JY (April 2008). "Surgery and global health: a view from beyond the OR". World Journal of Surgery. 32 (4): 533–536. doi:10.1007/s00268-008-9525-9. PMC 2267857. PMID 18311574.
- Dare AJ, Grimes CE, Gillies R, Greenberg SL, Hagander L, Meara JG, Leather AJ (December 2014). "Global surgery: defining an emerging global health field". Lancet. 384 (9961): 2245–2247. doi:10.1016/S0140-6736(14)60237-3. PMID 24853601. S2CID 37349469.
- O'Neill KM, Greenberg SL, Cherian M, Gillies RD, Daniels KM, Roy N, et al. (November 2016). "Bellwether Procedures for Monitoring and Planning Essential Surgical Care in Low- and Middle-Income Countries: Caesarean Delivery, Laparotomy, and Treatment of Open Fractures". World Journal of Surgery. Springer Science and Business Media LLC. 40 (11): 2611–2619. doi:10.1007/s00268-016-3614-y. PMID 27351714. S2CID 12830913.
- Chao TE, Sharma K, Mandigo M, Hagander L, Resch SC, Weiser TG, Meara JG (June 2014). "Cost-effectiveness of surgery and its policy implications for global health: a systematic review and analysis". The Lancet. Global Health. 2 (6): e334–e345. doi:10.1016/S2214-109X(14)70213-X. PMID 25103302.
- Xu K, Evans DB, Kawabata K, Zeramdini R, Klavus J, Murray CJ (July 2003). "Household catastrophic health expenditure: a multicountry analysis". Lancet. 362 (9378): 111–117. doi:10.1016/S0140-6736(03)13861-5. PMID 12867110. S2CID 2052830.
- Price R, Makasa E, Hollands M (September 2015). "World Health Assembly Resolution WHA68.15: "Strengthening Emergency and Essential Surgical Care and Anesthesia as a Component of Universal Health Coverage"—Addressing the Public Health Gaps Arising from Lack of Safe, Affordable and Accessible Surgical and Anesthetic Services". World Journal of Surgery. 39 (9): 2115–2125. doi:10.1007/s00268-015-3153-y. PMID 26239773. S2CID 13027859.
- Debas HT, Donkor P, Gawande A, Jamison DT, Kruk ME, Mock CN (2015-03-24). Disease Control Priorities. Vol. 1 Essential Surgery (Third ed.). ISBN 978-1-4648-0367-3.
- Truché P, Shoman H, Reddy CL, Jumbam DT, Ashby J, Mazhiqi A, et al. (January 2020). "Globalization of national surgical, obstetric and anesthesia plans: the critical link between health policy and action in global surgery". Globalization and Health. 16 (1): 1. doi:10.1186/s12992-019-0531-5. PMC 6941290. PMID 31898532.
- Laxminarayan R, Mills AJ, Breman JG, Measham AR, Alleyne G, Claeson M, et al. (April 2006). "Advancement of global health: key messages from the Disease Control Priorities Project". Lancet. 367 (9517): 1193–1208. doi:10.1016/S0140-6736(06)68440-7. PMID 16616562. S2CID 1567552.
- Bryce J, Black RE, Walker N, Bhutta ZA, Lawn JE, Steketee RW (2005). "Can the world afford to save the lives of 6 million children each year?". Lancet. 365 (9478): 2193–2200. doi:10.1016/S0140-6736(05)66777-3. PMID 15978927. S2CID 46067330.
- "Interventions in Health". Global Health Council. Archived from the original on 2011-01-06.
- Farmer P (July 2001). "The major infectious diseases in the world--to treat or not to treat?". The New England Journal of Medicine. 345 (3): 208–210. doi:10.1056/NEJM200107193450310. PMID 11463018.
- Anson A, Ramay B, de Esparza AR, Bero L (July 2012). "Availability, prices and affordability of the World Health Organization's essential medicines for children in Guatemala". Globalization and Health. 8: 22. doi:10.1186/1744-8603-8-22. PMC 3503802. PMID 22747646.
- Kiani A, Qadeer A, Mirza Z, Khanum A, Tisocki K, Mustafa T. "Prices, availability and affordability of medicines in Pakistan" (PDF). Geneva: Health Action International. 2006. Archived from the original (PDF) on 14 December 2010. Retrieved 7 April 2014.
- Garrett L (2007). "The Challenge of Global Health". Foreign Affairs.
- "The world health report 2006: working together for health". Geneva: World Health Organization. Archived from the original on December 2, 2006.
- Kilmarx PH, Maitin T, Adam T, Akuffo H, Aslanyan G, Cheetham M, et al. (August 2020). "A Mechanism for Reviewing Investments in Health Research Capacity Strengthening in Low- and Middle-Income Countries". Annals of Global Health. 86 (1): 92. doi:10.5334/aogh.2941. PMC 7413164. PMID 32832386.
- Riley K (2018-03-21). "U.S. at critical juncture with Global Health Security Agenda". Homeland Preparedness News. Retrieved 2018-03-23.
- "Global Health Security Agenda: Action Packages". 23 July 2021 – via U.S. Centers for Disease Control and Prevention (CDC).
- McPhee E, Gronvall GK, Sell TK (May 2019). "Analysis of sectoral participation in the development of Joint External Evaluations". BMC Public Health. 19 (1): 631. doi:10.1186/s12889-019-6978-8. PMC 6533773. PMID 31122234.
- "Global Health Security Agenda: Action Packages". CDC. 2016. Retrieved 18 November 2019.
- Wolicki SB, Nuzzo JB, Blazes DL, Pitts DL, Iskander JK, Tappero JW (2016). "Public Health Surveillance: At the Core of the Global Health Security Agenda". Health Security. 14 (3): 185–8. doi:10.1089/hs.2016.0002. PMC 6937158. PMID 27314658.
Further reading
- Jacobsen K (2008). Introduction to Global Health. Jones & Bartlett Learning. ISBN 978-0-7637-5159-3.
- Levine R (2007). Case Studies in Global Health: Millions Saved. Jones & Bartlett Publishers. ISBN 978-0-7637-4620-9.
- Palmer SP (2010). Launching Global Health: The Caribbean Odyssey of the Rockefeller Foundation. University of Michigan Press. ISBN 978-0472070893.
- Singer M, Erickson PI (2013). Global Health: An Anthropological Perspective. Waveland Press. ISBN 978-1-4786-1028-1.
- Skolnik R (2008). Essentials of Global Health. Jones & Bartlett Learning. ISBN 9780763734213.
- Skolnik R (2011). Global Health 101. Jones & Bartlett Publishers. ISBN 978-0-7637-9752-2.
- Spiegel JM, Huish R (2009). "Canadian foreign aid for global health: Human security opportunity lost". Canadian Foreign Policy Journal. 15 (3): 60–84. doi:10.1080/11926422.2009.9673492. ISSN 1192-6422. S2CID 154963843.
- Taylor AL, Hwenda L, Larsen BI, Daulaire N (December 2011). "Stemming the brain drain--a WHO global code of practice on international recruitment of health personnel". The New England Journal of Medicine. 365 (25): 2348–2351. doi:10.1056/NEJMp1108658. PMID 22187983.
- White F, Stallones L, Last JM (2013). Global Public Health: Ecological Foundations. Oxford University Press. ISBN 9780199751907.
External links
- GlobalHealth.gov (hosted by U.S. Department of Health & Human Services)
- Partnership for Maternal, Newborn and Child Health
- Roll Back Malaria – global partnership against malaria
- Stop TB – global partnership against tuberculosis