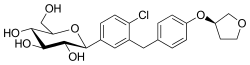
Empagliflozin
Empagliflozin, sold under the brand name Jardiance among others, is an antidiabetic medication used to improve glucose control in people with type 2 diabetes, used to reduce the risk of cardiovascular death in adults with type 2 diabetes and established cardiovascular disease, used to reduce the risk of death and hospitalization in people with heart failure and low ejection fraction, and used to reduce the risk of cardiovascular death and hospitalization for heart failure in adults.[6][8][2][9] It can be prescribed instead of metformin and has benefits over sulfonylureas.[10] It may be used together with other medications such as metformin or insulin.[2][9] It is not recommended for type 1 diabetes.[2] It is taken by mouth.[2]
 | |
| Clinical data | |
|---|---|
| Trade names | Jardiance, others |
| Other names | BI-10773 |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a614043 |
| License data |
|
| Pregnancy category |
|
| Routes of administration | By mouth |
| Drug class | Sodium-glucose cotransporter-2 (SGLT2) inhibitor[2] |
| ATC code | |
| Legal status | |
| Legal status | |
| Identifiers | |
IUPAC name
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| ECHA InfoCard | 100.122.058 |
| Chemical and physical data | |
| Formula | C23H27ClO7 |
| Molar mass | 450.91 g·mol−1 |
| 3D model (JSmol) | |
SMILES
| |
InChI
| |
Common side effects include urinary tract infections, fungal infections of the groin, and joint pains.[2] Rarer but more serious side effects include a skin infection of the groin called Fournier's gangrene and a form of diabetic ketoacidosis with normal blood sugar levels.[2][11] Use in pregnancy and breastfeeding is not recommended.[10] Use is not recommended in those with significant kidney disease, though it may help slow the progression of mild kidney problems.[2][9] Empagliflozin is an inhibitor of the sodium glucose co-transporter-2 (SGLT-2), and works by increasing sugar lost in the urine.[2]
Empagliflozin was approved for medical use in the United States and in the European Union in 2014.[2][12][13][7] It is on the World Health Organization's List of Essential Medicines.[14] In 2020, it was the 102nd most commonly prescribed medication in the United States, with more than 6 million prescriptions.[15][16]
Medical uses
Type 2 diabetes
Empagliflozin is used in combination with proper diet and exercise to help people with type 2 diabetes lower their blood sugar levels.[6] It can be used alongside other medications for type 2 diabetes such as metformin, sulfonylureas, and insulin.[17]
Weight and blood pressure
Empagliflozin causes moderate reductions in blood pressure and body weight. These effects are likely due to the excretion of glucose in the urine and a slight increase in urinary sodium excretion.[18][19] In clinical trials, patients taking empagliflozin lost an average of 2% of their baseline body weight.[20] A higher percentage of people taking empagliflozin achieved weight loss greater than 5% from their baseline.[19] The medication reduced systolic blood pressure by 3 to 5 millimeters of mercury (mmHg).[19] The effects on blood pressure and body weight are generally viewed as favorable, as many patients with type 2 diabetes have high blood pressure or are overweight or obese.[21][22]
Heart & kidney disease
Empagliflozin appears to reduce the likelihood of hospitalization for heart failure or progression of chronic kidney disease in people with type 2 diabetes. Empagliflozin may reduce the likelihood of death due to cardiovascular causes in people with type 2 diabetes who have known cardiovascular disease.[23][24][25][26] One concern regarding the trial on which these claims are based is that the different arms received different amounts of other medications; thus, the reduced risk cannot necessarily be attributed to empaglifozin.[27] In some countries it has also been approved to reduce the risk of death from cardiovascular causes in people with type 2 diabetes and heart disease.[26]
Treatment guidelines
Guidelines by the American Diabetes Association (ADA) and European Association for the Study of Diabetes (EASD) recommend SGLT-2 inhibitors like empagliflozin as second-line medications after metformin for type 2 diabetes in people with heart failure or chronic kidney disease.[9] For type 2 diabetes with established cardiovascular disease, the guidelines recommend either a SGLT-2 inhibitor or a GLP-1 agonist as second-line medications after metformin. In all other type 2 diabetes cases, SGLT-2 inhibitors like empagliflozin can be appropriate second-line options if blood glucose control or weight loss are treatment priorities. They are less appropriate if cost is a major factor.[9]
In the United Kingdom, empagliflozin is typically only recommended together with metformin if a sulfonylurea cannot be taken.[17]
Type 1 diabetes
Empagliflozin is not recommended for type 1 diabetes.[2] One trial studied its use in addition to insulin in people with type 1 diabetes.[28] The medications delivered modest improvements in blood glucose control and body weight but were associated with an increased risk of diabetic ketoacidosis, a dangerous complication of diabetes.[28] Empagliflozin is not approved by the U.S. Food and Drug Administration (FDA) for use in type 1 diabetes.[6]
Contraindications
- History of a severe allergic reaction to empagliflozin[6]
- End-stage kidney disease[6]
- Diabetic ketoacidosis[6]
Side effects
Common
- Empagliflozin increases the risk of genital fungal infections. The risk is highest in people with a prior history of genital fungal infections.[19]
- Urinary tract infections (UTIs) may be more common with empagliflozin. Certain individual clinical trials have demonstrated an increase risk but cumulative data across multiple trials show no increase in UTI risk.[20][19][21]
- Empagliflozin reduces systolic and diastolic blood pressure and can increase the risk of low blood pressure, which can cause fainting and/or falls.[19] The risk is higher in older people, people taking diuretics, and people with reduced kidney function.[19]
- Slight increases in LDL cholesterol can be seen with empagliflozin, in the range of 2% to 4% from baseline.[19]
Serious
- Diabetic ketoacidosis (DKA), a rare but potentially life-threatening condition, may occur more commonly with empagliflozin and other SGLT-2 inhibitors.[29][30] While DKA is usually associated with elevated blood glucose levels, in people taking SGLT-2 inhibitors DKA may be seen with uncharacteristically normal blood glucose levels, a phenomenon called euglycemic ketoacidosis.[29] The absence of elevated blood glucose levels in people on an SGLT-2 inhibitor may make it more difficult to diagnose DKA. The risk of empagliflozin-associated DKA may be higher in the setting of illness, dehydration, surgery, and/or alcohol consumption.[29] It is also seen in type 1 diabetes who take empagliflozin, which notably is an unapproved or "off-label" use of the medication.[30] To lessen the risk of developing ketoacidosis (a serious condition in which the body produces high levels of blood acids called ketones) after surgery, the FDA has approved changes to the prescribing information for SGLT2 inhibitor diabetes medicines to recommend they be stopped temporarily before scheduled surgery. Empagliflozin should each be stopped at least three days before scheduled surgery.[31] Symptoms of ketoacidosis include nausea, vomiting, abdominal pain, tiredness, and trouble breathing.[31]
- Fournier's gangrene, a rare but serious infection of the groin, occurs more commonly in people taking empagliflozin and other SGLT-2 inhibitors.[11][2] Symptoms include feverishness, a general sense of malaise, and pain or swelling around the genitals or in the skin behind them. The infection progresses quickly and urgent medical attention is recommended.[11]
- Empagliflozin can increase risk of low blood sugar when it is used together with a sulfonylurea or insulin.[32] When used by itself or in addition to metformin it does not appear to increase the risk of hypoglycemia.[21]
Mechanism of action
Empagliflozin is an inhibitor of the sodium glucose co-transporter-2 (SGLT-2), which is found almost exclusively in the proximal tubules of nephronic components in the kidneys. SGLT-2 accounts for about 90 percent of glucose reabsorption into the blood. Blocking SGLT-2 reduces blood glucose by blocking glucose reabsorption in the kidney and thereby excreting glucose (i.e., blood sugar) via the urine.[33][34][35]
History
It was developed by Boehringer Ingelheim and Eli Lilly and Company. It is also available as the combinations empagliflozin/linagliptin, empagliflozin/metformin, and empagliflozin/linagliptin/metformin.
Society and culture
Legal status
As of May 2013, Boehringer and Lilly had submitted applications for marketing approval to the European Medicines Agency (EMA) and the U.S. Food and Drug Administration (FDA).[36] The drug was approved in the European Union in May 2014,[7] and was approved in the United States in August 2014.[12][37] The FDA required four postmarketing studies: a cardiovascular outcomes trial, two studies in children, and a toxicity study in animals related to the pediatric trials.[37]
Research
A single study shows that half a tablet of empagliflozin 25mg has similar glycemic efficacy as a full tablet with the added advantage of reducing the monthly cost of therapy.[38]
References
- "Empagliflozin (Jardiance) Use During Pregnancy". Drugs.com. 30 August 2018. Retrieved 10 February 2020.
- "Empagliflozin Monograph for Professionals". Drugs.com. AHFS. Retrieved 21 December 2018.
- "AusPAR: Empagliflozin". Therapeutic Goods Administration (TGA). 8 November 2017. Retrieved 24 March 2022.
- "Jardiance 10 mg film-coated tablets – Summary of Product Characteristics (SmPC)". (emc). Retrieved 10 February 2020.
- "Jardiance 25 mg film-coated tablets – Summary of Product Characteristics (SmPC)". (emc). 23 October 2019. Retrieved 10 February 2020.
- "Jardiance- empagliflozin tablet, film coated". DailyMed. 22 January 2020. Retrieved 10 February 2020.
- "Jardiance EPAR". European Medicines Agency (EMA). Retrieved 10 February 2020.
- "FDA Approves Treatment for Wider Range of Patients with Heart Failure". U.S. Food and Drug Administration (FDA) (Press release). 25 February 2022. Retrieved 27 February 2022.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - Davies MJ, D'Alessio DA, Fradkin J, Kernan WN, Mathieu C, Mingrone G, et al. (December 2018). "Management of hyperglycaemia in type 2 diabetes, 2018. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD)". Diabetologia. 61 (12): 2461–2498. doi:10.1007/s00125-018-4729-5. PMID 30288571.
- British national formulary: BNF 76 (76 ed.). Pharmaceutical Press. 2018. p. 691. ISBN 9780857113382.
- "FDA warns about rare occurrences of a serious infection of the genital area with SGLT2 inhibitors for diabetes". U.S. Food and Drug Administration (FDA). 9 February 2019. Retrieved 18 March 2019.
- "Drug Approval Package: Jardiance (empagliflozin) Tablets NDA #204629". U.S. Food and Drug Administration (FDA). 8 September 2014. Retrieved 10 February 2020.
- "Jardiance: FDA-Approved Drugs". U.S. Food and Drug Administration (FDA). Retrieved 10 February 2020.
- World Health Organization (2021). World Health Organization model list of essential medicines: 22nd list (2021). Geneva: World Health Organization. hdl:10665/345533. WHO/MHP/HPS/EML/2021.02.
- "The Top 300 of 2020". ClinCalc. Retrieved 7 October 2022.
- "Empagliflozin - Drug Usage Statistics". ClinCalc. Retrieved 7 October 2022.
- "Empagliflozin in combination therapy for treating type 2 diabetes". NICE. Guidance and guidelines. 25 March 2015. Retrieved 21 December 2018.
- Verma S, McMurray JJ (October 2018). "SGLT2 inhibitors and mechanisms of cardiovascular benefit: a state-of-the-art review". Diabetologia. 61 (10): 2108–2117. doi:10.1007/s00125-018-4670-7. PMID 30132036.
- "Empagliflozin (Jardiance) National Drug Monograph" (PDF). VA Pharmacy Benefits Management Services, Medical Advisory Panel, and VISN Pharmacist Executives.
- Zimmermann J (December 2016). "Empagliflozin (Jardiance) for type 2 diabetes mellitus". American Family Physician. 94 (12): 1014–1015. PMID 28075091.
- Anderson JE, Wright EE, Shaefer CF (February 2017). "Empagliflozin: Role in treatment options for patients with type 2 diabetes mellitus". Diabetes Therapy. 8 (1): 33–53. doi:10.1007/s13300-016-0211-x. PMC 5306110. PMID 27837465.
- "Obesity and overweight fact sheet" (PDF). World Health Organization.
- Philippaert K, Kalyaanamoorthy S, Fatehi M, Long W, Soni S, Byrne NJ, et al. (June 2021). "Cardiac Late Sodium Channel Current Is a Molecular Target for the Sodium/Glucose Cotransporter 2 Inhibitor Empagliflozin". Circulation. 143 (22): 2188–2204. doi:10.1161/CIRCULATIONAHA.121.053350. PMC 8154177. PMID 33832341.
- Zelniker TA, Wiviott SD, Raz I, Im K, Goodrich EL, Bonaca MP, et al. (January 2019). "SGLT2 inhibitors for primary and secondary prevention of cardiovascular and renal outcomes in type 2 diabetes: A systematic review and meta-analysis of cardiovascular outcome trials". Lancet. 393 (10166): 31–39. doi:10.1016/S0140-6736(18)32590-X. PMID 30424892. S2CID 53277899.
- Usman MS, Siddiqi TJ, Memon MM, Khan MS, Rawasia WF, Talha Ayub M, et al. (March 2018). "Sodium-glucose co-transporter 2 inhibitors and cardiovascular outcomes: A systematic review and meta-analysis". European Journal of Preventive Cardiology. 25 (5): 495–502. doi:10.1177/2047487318755531. PMID 29372664. S2CID 3557967.
- "FDA approves Jardiance to reduce cardiovascular death in adults with type 2 diabetes" (Press release). U.S. Food and Drug Administration (FDA). 6 December 2016. Retrieved 12 December 2016.
- "EMPA-REG Outcome trial: What does it mean?" (PDF). Therapeutics Initiative. July–August 2017. Retrieved 21 December 2018.
- Riddle MC, Cefalu WT (December 2018). "SGLT Inhibitors for Type 1 Diabetes: An obvious choice, or too good to be true?". Diabetes Care. 41 (12): 2444–2447. doi:10.2337/dci18-0041. PMID 30459245.
- Rosenstock J, Ferrannini E (September 2015). "Euglycemic diabetic ketoacidosis: A predictable, detectable, and preventable safety concern with SGLT2 inhibitors". Diabetes Care. 38 (9): 1638–1642. doi:10.2337/dc15-1380. PMID 26294774.
- Handelsman Y, Henry RR, Bloomgarden ZT, Dagogo-Jack S, DeFronzo RA, Einhorn D, et al. (June 2016). "American Association of Clinical Endocrinologists and American College of Endocrinology Position Statement on the Association of Sglt-2 Inhibitors and Diabetic Ketoacidosis". Endocrine Practice. 22 (6): 753–762. doi:10.4158/EP161292.PS. PMID 27082665.
- "FDA revises labels of SGLT2 inhibitors for diabetes to include warning". U.S. Food and Drug Administration. 19 March 2020. Retrieved 6 June 2020.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - "Empagliflozin in combination therapy for treating type 2 diabetes". NICE. 25 March 2015. Retrieved 21 December 2018.
- Abdul-Ghani MA, DeFronzo RA (September 2008). "Inhibition of renal glucose reabsorption: A novel strategy for achieving glucose control in type 2 diabetes mellitus". Endocrine Practice. 14 (6): 782–790. doi:10.4158/ep.14.6.782. PMID 18996802.
- Nair S, Wilding JP (January 2010). "Sodium glucose cotransporter 2 inhibitors as a new treatment for diabetes mellitus". The Journal of Clinical Endocrinology and Metabolism. 95 (1): 34–42. doi:10.1210/jc.2009-0473. PMID 19892839.
- Bays H (March 2009). "From victim to ally: The kidney as an emerging target for the treatment of diabetes mellitus". Current Medical Research and Opinion. 25 (3): 671–681. doi:10.1185/03007990802710422. PMID 19232040. S2CID 73341491.
- Tucker, Miriam E. (7 May 2013). "First details of empagliflozin trials follow US and EU filings". Medscape Medical News.
- Mechatie E (1 August 2014). "FDA approves empagliflozin for adults with type 2 diabetes". Clinical Endocrinology News Digital Network.
- Dutta D, Sharma M, Aggarwal S, Agarwal A, Dhall A (March 2022). "Treatment outcomes of graded dose of empagliflozin in type-2 diabetes: A real world study". Ann Afr Med. 21 (1): 26–33. doi:10.4103/aam.aam_69_20. PMC 9020632. PMID 35313401. S2CID 247569552.