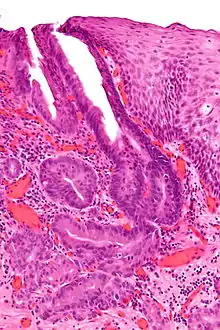
Oesophagogastric junctional adenocarcinoma
Oesophagogastric junctional adenocarcinoma (OGJ adenocarcinoma) is a cancer of the lower part of the oesophagus with a rising incidence in Western countries.[1] This disease is often linked to Barrett's oesophagus.
The incidence of OGJ adenocarcinoma is rising rapidly in Western countries especially in recent decades, in contrast to the declining frequency of distal gastric adenocarcinoma. Treatment options for adenocarcinomas involving the oesophagogastric junction are limited and the overall prognosis is extremely poor, with a five-year survival rate of approximately 30% with surgery alone.[2]
Risk factors
There are several established risk factors for OGJ adenocarcinoma. The biggest risk factors include gastroesophageal reflux disease (GERD) and Barrett's oesophagus. Other risk factors include smoking (with a twofold-increase) and obesity.[3]
Clinical features
The clinical features of OGJ adenocarcinoma are variable depending on the extent of the tumor. Early stages are oftentimes asymptomatic or have difficulty swallowing. More advanced stages can present with signs and symptoms of anemia, especially iron deficiency anemia from chronic gastrointestinal bleeding, weight loss, cervical adenopathy, hoarseness or change in voice, and progressive difficulty with swallowing (initially with solid foods and then with liquids).[4]
Distant metastases typically occur in the liver, lungs, bones, and adrenal glands and can manifest with symptoms typical of involvement with these sites (e.g. abdominal pain, pathological fractures, dyspnea). However, there have been described cases of atypical metastasis sites including the muscle, brain, and skin.[5]
Diagnostics
The diagnostic workup for OGJ adenocarcinoma usually involves performing an endoscopy with endoscopic biopsy of suspicious looking tissue. Accurate staging of tumor extent and involvement of surrounding tissue or distant metastases is critical to establishing a prognosis, and is usually guided by endoscopic ultrasound, computed tomography scans, and/or positron emission tomography scans to establish the extent of disease. Additionally, genetic analysis of the tumor may yield mutations that may be clinically significant, as described below.
Classification
There is no standardized system for the classification of OGJ adenocarcinoma. The Siewart classification system is a classification scheme used for OGJ adenocarcinomas that has been adopted by many clinicians.[6]
Siewart described three different categories of OGJ adenocarcinoma, all based upon anatomic location:
- A Type I tumor, located between 5 and 1cm proximal to the OGJ, is an adenocarcinoma that typically arises from an area of intestinal metaplasia of the esophagus and can infiltrate the OGJ from above.
- A Type II tumor, located between 1cm proximal and 2cm distal to the OGJ, is a true adenocarcinoma of the gastric cardia.
- A Type III tumor, located between 2 and 5 cm distal to the OGJ is a subcardial gastric carcinoma that typically infiltrates the EGJ from below.
The classification system establishes guidelines for surgical approaches to tumor resection.
Oncogenetics
OGJ adenocarcinoma is a highly mutated and heterogeneous disease. Microsatellite instability (MSI) can be observed and coincides with an elevated number of somatic mutations. Potentially actionable coding mutations have been identified in 67 genes, including those in CR2, HGF, FGFR4 and ESRRB.
Numerous genes harboring somatic coding mutations and copy number changes in the microsatellite stable (MSS) OGJ adenocarcinomas are also known to be altered with similar predicted functional consequence in other tumour types. TP53, SYNE1, and ARID1A are among the most frequently mutated genes.[7]
Notably, up to one third of OGJ adenocarcinomas have been found to have human epidermal growth factor receptor 2 (HER2) overexpression or amplification, which may be targetable with trastuzumab, conferring a modest survival benefit based on initial clinical trials.[8][9]
Treatment
There is no established consensus on treatment approaches for OGJ adenocarcinoma. The mainstay of treatment is surgical resection, guided by the Siewart classification system, followed by adjuvant chemotherapy for advanced disease.[10]
References
- Devesa SS, Blot WJ, Fraumeni JF (November 1998). "Changing patterns in the incidence of esophageal and gastric carcinoma in the United States". Cancer. 83 (10): 2049–2053. doi:10.1002/(SICI)1097-0142(19981115)83:10<2049::AID-CNCR1>3.0.CO;2-2. PMID 9827707.
- Njei B, McCarty TR, Birk JW (June 2016). "Trends in esophageal cancer survival in United States adults from 1973 to 2009: A SEER database analysis". Journal of Gastroenterology and Hepatology. 31 (6): 1141–1146. doi:10.1111/jgh.13289. PMC 4885788. PMID 26749521.
- "Esophageal Cancer Risk Factors | Esophagus Cancer Risk". www.cancer.org. Retrieved 2022-03-20.
- Schatz RA, Rockey DC (February 2017). "Gastrointestinal Bleeding Due to Gastrointestinal Tract Malignancy: Natural History, Management, and Outcomes". Digestive Diseases and Sciences. 62 (2): 491–501. doi:10.1007/s10620-016-4368-y. PMID 28032204. S2CID 6901790.
- Shaheen O, Ghibour A, Alsaid B (2017-06-04). "Esophageal Cancer Metastases to Unexpected Sites: A Systematic Review". Gastroenterology Research and Practice. 2017: 1657310. doi:10.1155/2017/1657310. PMC 5474273. PMID 28659974.
- Siewert JR, Stein HJ (July 1996). "Carcinoma of the gastroesophageal junction - classification, pathology and extent of resection". Diseases of the Esophagus. 9 (3): 173–182. doi:10.1093/dote/9.3.173. ISSN 1120-8694.
- Chong IY, Cunningham D, Barber LJ, Campbell J, Chen L, Kozarewa I, et al. (November 2013). "The genomic landscape of oesophagogastric junctional adenocarcinoma". The Journal of Pathology. 231 (3): 301–310. doi:10.1002/path.4247. PMID 24308032. S2CID 24219275.
- Zhao D, Klempner SJ, Chao J (May 2019). "Progress and challenges in HER2-positive gastroesophageal adenocarcinoma". Journal of Hematology & Oncology. 12 (1): 50. doi:10.1186/s13045-019-0737-2. PMC 6525398. PMID 31101074.
- Bang YJ, Van Cutsem E, Feyereislova A, Chung HC, Shen L, Sawaki A, et al. (August 2010). "Trastuzumab in combination with chemotherapy versus chemotherapy alone for treatment of HER2-positive advanced gastric or gastro-oesophageal junction cancer (ToGA): a phase 3, open-label, randomised controlled trial". Lancet. 376 (9742): 687–697. doi:10.1016/S0140-6736(10)61121-X. PMID 20728210. S2CID 8825706.
- Lin D, Khan U, Goetze TO, Reizine N, Goodman KA, Shah MA, et al. (January 2019). "Gastroesophageal Junction Adenocarcinoma: Is There an Optimal Management?". American Society of Clinical Oncology Educational Book. American Society of Clinical Oncology. Annual Meeting. 39 (39): e88–e95. doi:10.1200/EDBK_236827. PMID 31099690. S2CID 157056190.