Allergies in children
| Allergy | |
|---|---|
| Other names | Allergic diseases |
 | |
| Hives are a common allergic symptom | |
| Specialty | Allergy and immunology |
| Symptoms | Red eyes, itchy rash, runny nose, shortness of breath, swelling, sneezing |
| Types | Hay fever, food allergies, atopic dermatitis, allergic asthma, anaphylaxis |
| Causes | Genetic and environmental factors |
| Diagnostic method | Based on symptoms, skin prick test |
| Differential diagnosis | Food intolerances, food poisoning |
| Prevention | Repeated exposure to allergens, prophylactic respiratory medications |
| Treatment | Avoiding known allergens, medications, allergen immunotherapy |
| Medication | Steroids, antihistamines, epinephrine |
Allergies in children are those causes, pathophsiology, treatments, management, practices and control of allergies that develop in children.[1] [2] Up to 40 percent of children suffer from allergic rhinitis. And children are more likely to develop allergies if one or both parents have allergies.[3] Allergies differ between adults and children. Part of the reason for this that the respiratory system in children is smaller. The bronchi and bronchioles are narrower so even a slight decrease in diameter of these airways can have serious consequences. Many children outgrow their allergies.
The incidence of childhood allergies has increased in the past 50 years.[4]
Signs and symptoms
The signs and symptoms of allergies in a child are:
- Chronic symptoms resembling the cold that last more than a week or two[1][3]
- Cold-like symptoms that appear during the same time each year
- Repeated difficulty breathing, wheezing and breathing
- Cold-like symptoms that happen at night
- Cold-like symptoms that happen during exercise
- Chronic rashes or patches of skin that are dry, itchy, look like scales
- Cold-like symptoms that appear after eating a certain food
- Hives
- Swelling of face, arms or legs
- Gagging, coughing or wheezing, vomiting or significant abdominal pain
- Itching or tingling sensations in the mouth, throat or ears[1]
Cause
Each home contains possible allergens that can develop into allergies after exposure to:
- Dust mites
- Dogs and cats
- Other furry pets
- Cockroaches
- Mice and rats
- Plants
- Indoor smoking[5]
- Mold[1]
Vitamin D deficiency at the time of birth and exposure to egg white, milk, peanut, walnut, soy, shrimp, cod fish, and wheat makes a child more susceptible to allergies.[4] Soy-based infant formula is associated with allergies in infants.[6] Though, in recent years they have been becoming more common in children ages 4 and older.
Pathophysiology
A child's allergy is an immune system reaction. The child is reacting to a specific substance, or allergen. The immune system of a child responds to the invading allergen by releasing histamine and other chemicals that typically trigger symptoms in the nose, lungs, throat, sinuses, ears, eyes, skin, or stomach lining. In some children, allergies can also trigger symptoms of asthma—a disease that causes wheezing or difficulty breathing. If a child has allergies and asthma, controlling the allergies is important because the lack of treatment may make the allergies worse.[3] Compounds such as phthalates are associated with asthma in children.[7][8] Asthma in children is associated with exposure to indoor allergens.[9] in early childhood may prevent the development of asthma, but exposure at an older age may provoke bronchoconstriction.[10] Use of antibiotics in early life has been linked to the development of asthma.[11] Exposure to indoor volatile organic compounds may be a trigger for asthma; formaldehyde exposure, for example, has a positive association.[12]
Diagnosis
Testing is available to help identify any environmental or food allergies.[1] Caregivers and clinicians can assess the child for the development of an allergy by noting the presence of signs and symptoms and history of exposure.[1]
Prevention
.png.webp)
.png.webp)
Avoiding allergens will help prevent symptoms. Allergies that a child has to the family pet can be controlled by removing the animal and finding it a new home. Exterminating cockroaches, mice and rats and a thorough cleaning can reduce symptoms of an allergy in children. Dust mites are attracted to moisture. They consume human skin that has come off and lodged in, furniture, rugs, mattresses, box springs, and pillows. The child's bedding can be covered with allergen-proof covers. Laundering of the child's clothing, bed linens and blankets will also reduce exposure.[1]
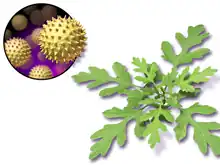
Exposure to allergens outside the home can be controlled with the use of air conditioners. Washing the hair, taking a bath or shower before bedtime can be done to remove allergens that have been picked up from outside the home. If grass or grass pollen is an allergen it is sometimes beneficial to remain indoors while grass is being cut or mowed. Children with allergies to grass can avoid playing in the grass to prevent allergic symptoms. Staying out of piled leaves in the fall can help. Pets returning into the home after being outdoors may track in allergens.[1]
Epidemiology
Up to 5% of infants that are fed cow's milk-based formula will develop an allergy to cow's milk.[13] Over half of cases in children in the United States occur in areas with air quality below EPA standards.[14]
Bibliography
- Walker, Marsha (2011). Breastfeeding management for the clinician : using the evidence. Sudbury, Mass: Jones and Bartlett Publishers. ISBN 9780763766511.
References
- 1 2 3 4 5 6 7 8 "Allergy Tips". www.aap.org. Retrieved 25 July 2017.
- ↑ "Asthma Fact sheet №307". WHO. November 2013. Archived from the original on June 29, 2011. Retrieved 3 March 2016.
- 1 2 3 "Allergy Relief for Your Child". United States Food and Drug Administration. 1 June 2017. Retrieved 25 July 2017.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - 1 2 Stallings, Virginia A.; Oria, Maria P. (2017). Finding a Path to Safety in Food Allergy: Assessment of the Global Burden, Causes, Prevention, Management, and Public Policy. doi:10.17226/23658. ISBN 978-0-309-45031-7. PMID 28609025.
- ↑ Jamil, Dr Maria; Janabi, Dr Marya Shamel Yousef Al; Francis, Dr Neema; Ali, Dr Shaher; Alfalahi, Dr Arwa; Ibrahim, Dr Mohammad (2021-06-12). "Prevalence of Asthma among High School Students in Ajman, Uae: A Cross-Sectional Study". Annals of the Romanian Society for Cell Biology. 25 (6): 10843–10849.
- ↑ Nowak-Węgrzyn, Anna; Katz, Yitzhak; Mehr, Sam Soheil; Koletzko, Sibylle (1 May 2015). "Non–IgE-mediated gastrointestinal food allergy". Journal of Allergy and Clinical Immunology. 135 (5): 1114–1124. doi:10.1016/j.jaci.2015.03.025. PMID 25956013.
- ↑ Jaakkola, J.J.; Knight, T.L. (July 2008). "The role of exposure to phthalates from polyvinyl chloride products in the development of asthma and allergies: a systematic review and meta-analysis". Environ Health Perspect. 116 (7): 845–53. doi:10.1289/ehp.10846. PMC 2453150. PMID 18629304.
- ↑ Bornehag, CG; Nanberg, E (April 2010). "Phthalate exposure and asthma in children". International Journal of Andrology. 33 (2): 333–45. doi:10.1111/j.1365-2605.2009.01023.x. PMID 20059582.
- ↑ Ahluwalia, SK; Matsui, EC (April 2011). "The indoor environment and its effects on childhood asthma". Current Opinion in Allergy and Clinical Immunology. 11 (2): 137–43. doi:10.1097/ACI.0b013e3283445921. PMID 21301330. S2CID 35075329.
- ↑ Rao, D; Phipatanakul, W (October 2011). "Impact of environmental controls on childhood asthma". Current Allergy and Asthma Reports. 11 (5): 414–20. doi:10.1007/s11882-011-0206-7. PMC 3166452. PMID 21710109.
- ↑ Murk, W; Risnes, KR; Bracken, MB (June 2011). "Prenatal or early-life exposure to antibiotics and risk of childhood asthma: a systematic review". Pediatrics. 127 (6): 1125–38. doi:10.1542/peds.2010-2092. PMID 21606151. S2CID 26098640.
- ↑ McGwin, G; Lienert, J; Kennedy, JI (March 2010). "Formaldehyde exposure and asthma in children: a systematic review". Environmental Health Perspectives. 118 (3): 313–7. doi:10.1289/ehp.0901143. PMC 2854756. PMID 20064771.
- ↑ Walker, p. 28.
- ↑ American Lung, Association (June 2001). "Urban air pollution and health inequities: a workshop report". Environmental Health Perspectives. 109 Suppl 3: 357–74. doi:10.1289/ehp.01109s3357. PMC 1240553. PMID 11427385.