Eating disorder
| Eating disorders | |
|---|---|
.jpg.webp) | |
| Sketch of a person with anorexia nervosa | |
| Specialty | Psychiatry |
| Symptoms | Abnormal eating habits that negatively affect physical or mental health[1] |
| Complications | Anxiety disorders, depression, substance abuse[2] |
| Types | Binge eating disorder, anorexia nervosa, bulimia nervosa, pica, rumination disorder, avoidant/restrictive food intake disorder[1] |
| Causes | Unclear[3] |
| Risk factors | Gastrointestinal disorders, history of sexual abuse, being a dancer or gymnast[4][5][6][7] |
| Treatment | Counselling, proper diet, normal amount of exercise, medications[2] |
An eating disorder is a mental disorder defined by abnormal eating habits that negatively affect a person's physical or mental health.[1] They include binge eating disorder, where people eat a large amount in a short period of time; anorexia nervosa, where people eat very little due to a fear of gaining weight and thus have a low body weight; bulimia nervosa, where people eat a lot and then try to rid themselves of the food; pica, where people eat non-food items; rumination syndrome, where people regurgitate food; avoidant/restrictive food intake disorder (ARFID), where people have a lack of interest in food; and a group of other specified feeding or eating disorders.[1] Anxiety disorders, depression and substance abuse are common among people with eating disorders.[2] These disorders do not include obesity.[1]
The causes of eating disorders are not clear, although both biological and environmental factors appear to play a role.[2][3] Eating disorders affect about 12 percent of dancers.[4] Cultural idealization of thinness is believed to contribute to some eating disorders.[3] Individuals who have experienced sexual abuse are also more likely to develop eating disorders.[6] Some disorders such as pica and rumination disorder occur more often in people with intellectual disabilities.[1] Only one eating disorder can be diagnosed at a given time.[1]
Treatment can be effective for many eating disorders.[2] Treatment varies by disorder and may involve counselling, dietary advice, reducing excessive exercise and the reduction of efforts to eliminate food.[2] Medications may be used to help with some of the associated symptoms.[2] Hospitalization may be needed in more serious cases.[2] About 70% of people with anorexia and 50% of people with bulimia recover within five years.[8] Recovery from binge eating disorder is less clear and estimated at 20% to 60%.[8] Both anorexia and bulimia increase the risk of death.[8]
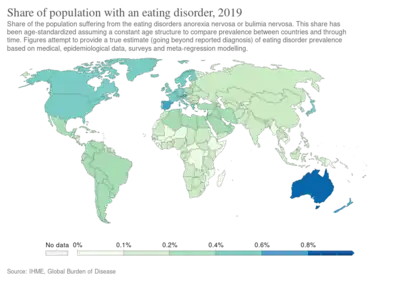
In the developed world, anorexia affects about 0.4% and bulimia affects about 1.3% of young women in a given year.[1] Binge eating disorder affects about 1.6% of women and 0.8% of men in a given year.[1] Among women about 4% have anorexia, 2% have bulimia, and 2% have binge eating disorder at some time in their life.[8] Rates of eating disorders appear to be lower in less developed countries.[9] Anorexia and bulimia occur nearly ten times more often in females than males.[1] Eating disorders typically begin in late childhood or early adulthood.[2] Rates of other eating disorders are not clear.[1]
Classification
Bulimia nervosa is a disorder characterized by episodes of binge eating and purging, as well as excessive evaluation of one's self-worth in terms of body weight or shape. Purging can include self-induced vomiting, over-exercising, and the use of diuretics, enemas, or laxatives.[1]
Anorexia nervosa is characterized by extreme food restriction, low body weight, and the fear of becoming fat.[1] Pubertal and post-pubertal females with anorexia often experience amenorrhea, or the loss of menstrual periods, due to the extreme weight loss these individuals face. Although amenorrhea was a required criterion for a diagnosis of anorexia in the DSM-IV, it was dropped in the DSM-5 due to its exclusive nature, as male, post-menopause women, or individuals who do not menstruate for other reasons would fail to meet this criterion.[10] Females with bulimia may also experience amenorrhea, although the cause is not clear.[11]
Two subtypes of anorexia nervosa are specified in the DSM-5—restricting type and binge-eating/purging type. Those who have the restricting type of anorexia nervosa restrict food intake and do not engage in binge eating, whereas those with the binge/purge type lose control over their eating at least occasionally and may compensate for these binge episodes. Although similar in presentation to bulimia, individuals with the binge-eating/purging subtype of anorexia are typically underweight, whereas those with bulimia tend to be normal weight or overweight.[11][12]
ICD and DSM
These eating disorders are specified as mental disorders in standard medical manuals, including the ICD-10 and the DSM-5.
- Anorexia nervosa (AN) is characterized by lack of maintenance of a healthy body weight, an obsessive fear of gaining weight or refusal to do so, and an unrealistic perception, or non-recognition of the seriousness, of current low body weight.[13]
- Bulimia nervosa (BN) is characterized by recurrent binge eating followed by compensatory behaviors such as purging (self-induced vomiting, eating to the point of vomiting, excessive use of laxatives/diuretics, or excessive exercise). Fasting may also be used as a method of purging following a binge. However, unlike anorexia nervosa, body weight is maintained at or above a minimally normal level.
- Binge eating disorder (BED) is characterized by recurring binge eating at least once a week for over a period of 3 months while experiencing lack of control and guilt after overeating.[1] There are no compensatory behaviors. However, unlike anorexia nervosa, body weight is maintained at or above a minimally normal level. The disorder can develop in individuals of a wide range of ages and socioeconomic classes.[14][15]
- Other Specified Feeding or Eating Disorder (OSFED) is an eating or feeding disorder that does not meet full DSM-5 criteria for AN, BN, or BED. Examples of otherwise-specified eating disorders include individuals with atypical anorexia nervosa, who meet all criteria for AN except being underweight despite substantial weight loss; atypical bulimia nervosa, who meet all criteria for BN except that bulimic behaviors are less frequent or have not been ongoing for long enough; purging disorder; and night eating syndrome.[1]
Other
- Avoidant/restrictive food intake disorder (ARFID), which includes cases characterized by strict adherence to a limited repertoire of foods (“restriction”, former “selective eating disorder”), and cases with fears of eating secondary to fears of choking or vomiting (phobic, “avoidant”). [1] [16].
- Compulsive overeating, which may include habitual "grazing" of food or episodes of binge eating without feelings of guilt.[17]
- Diabulimia, which is characterized by the deliberate manipulation of insulin levels by diabetics in an effort to control their weight.
- Drunkorexia, which is commonly characterized by purposely restricting food intake in order to reserve food calories for alcoholic calories, exercising excessively in order to burn calories from drinking, and over-drinking alcohol in order to purge previously consumed food.[18]
- Food maintenance, which is characterized by a set of aberrant eating behaviors of children in foster care.[19]
- Gourmand syndrome, a rare condition occurring after damage to the frontal lobe. Individuals develop an obsessive focus on fine foods.[20]
- Orthorexia nervosa, a term used by Steven Bratman to describie an obsession with a "pure" diet, in which a person develops an obsession with avoiding unhealthy foods to the point where it interferes with the person's life.[21]
- Prader-Willi syndrome, a genetic disorder associated with insatiable appetite and morbid obesity.
- Pregorexia, which is characterized by extreme dieting and over-exercising in order to control pregnancy weight gain. Prenatal undernutrition is associated with low birth weight, coronary heart disease, type 2 diabetes, stroke, hypertension, cardiovascular disease risk, and depression.[22]
- Muscle dysmorphia is characterized by appearance preoccupation that one's own body is too small, too skinny, insufficiently muscular, or insufficiently lean. Muscle dysmorphia affects mostly males.
Signs and symptoms
Symptoms and complications vary according to the nature and severity of the eating disorder:[23]
| acne | xerosis | amenorrhoea | tooth loss, cavities |
| constipation | diarrhea | water retention and/or edema | lanugo |
| telogen effluvium | cardiac arrest | hypokalemia | death |
| osteoporosis[24] | electrolyte imbalance | hyponatremia | brain atrophy[25][26] |
| pellagra[27] | scurvy | kidney failure | suicide[28][29][30] |
Associated physical symptoms of eating disorders include weakness, fatigue, sensitivity to cold, reduced beard growth in men, reduction in waking erections, reduced libido, weight loss and growth failure.[31]
Frequent vomiting, which may cause acid reflux or entry of acidic gastric material into the laryngoesophageal tract, can lead to unexplained hoarseness. As such, individuals who induce vomiting as part of their eating disorder, such as those with anorexia nervosa, binge eating-purging type or those with purging-type bulimia nervosa, are at risk for acid reflux.
Polycystic ovary syndrome (PCOS) is the most common endocrine disorder to affect women. Though often associated with obesity it can occur in normal weight individuals. PCOS has been associated with binge eating and bulimic behavior.[32][33][34][35][36][37]
Other possible manifestations are dry lips,[38] burning tongue,[38] parotid gland swelling,[38] and temporomandibular disorders.[38]
Pro-ana subculture
Pro-ana refers to the promotion of behaviors related to the eating disorder anorexia nervosa. Several websites promote eating disorders, and can provide a means for individuals to communicate in order to maintain eating disorders. Members of these websites typically feel that their eating disorder is the only aspect of a chaotic life that they can control.[39] These websites are often interactive and have discussion boards where individuals can share strategies, ideas, and experiences, such as diet and exercise plans that achieve extremely low weights.[40] A study comparing the personal web-blogs that were pro-eating disorder with those focused on recovery found that the pro-eating disorder blogs contained language reflecting lower cognitive processing, used a more closed-minded writing style, contained less emotional expression and fewer social references, and focused more on eating-related contents than did the recovery blogs.[41]
Psychopathology
The psychopathology of eating disorders centers around body image disturbance, such as concerns with weight and shape; self-worth being too dependent on weight and shape; fear of gaining weight even when underweight; denial of how severe the symptoms are and a distortion in the way the body is experienced.[31]
The main psychopathological features of anorexia were outlined in 1982 as problems in body perception, emotion processing and interpersonal relationships.[42][43] Women with eating disorders have greater body dissatisfaction.[44] This impairment of body perception involves vision, proprioception, and tactile perception.[45] There is an alteration in integration of signals in which body parts are experienced as dissociated from the body as a whole.[45] Bruch theorized that difficult early relationships were related to the cause of anorexia and how primary caregivers can contribute to the onset of the illness.[42]
A prominent feature of bulimia is dissatisfaction with body shape.[46] However, dissatisfaction with body shape is not of diagnostic significance as it is sometimes present in individuals with no eating disorder.[46] This highly labile feature can fluctuate depending on changes in shape and weight, the degree of control over eating and mood.[46] In contrast, a necessary diagnostic feature for anorexia nervosa and bulimia nervosa is having overvalued ideas about shape and weight are relatively stable and closely related to the patients’ low self-esteem.[46]
Causes
The causes of eating disorders are not clear.
Many people with eating disorders also have body dysmorphic disorder, altering the way a person sees oneself.[47][48] Studies have found that a high proportion of individuals diagnosed with body dysmorphic disorder also had some type of eating disorder, with 15% of individuals having either anorexia nervosa or bulimia nervosa.[47] This link between body dysmorphic disorder and anorexia stems from the fact that both BDD and anorexia nervosa are characterized by a preoccupation with physical appearance and a distortion of body image.[48] There are also many other possibilities such as environmental, social and interpersonal issues that could promote and sustain these illnesses.[49] Also, the media are oftentimes blamed for the rise in the incidence of eating disorders due to the fact that media images of idealized slim physical shape of people such as models and celebrities motivate or even force people to attempt to achieve slimness themselves. The media are accused of distorting reality, in the sense that people portrayed in the media are either naturally thin and thus unrepresentative of normality or unnaturally thin by forcing their bodies to look like the ideal image by putting excessive pressure on themselves to look a certain way. While past findings have described eating disorders as primarily psychological, environmental, and sociocultural, further studies have uncovered evidence that there is a genetic component.[50]
Genetics
Numerous studies show a genetic predisposition toward eating disorders.[51][51][52] Twin studies have found a slight instances of genetic variance when considering the different criterion of both anorexia nervosa and bulimia nervosa as endophenotypes contributing to the disorders as a whole.[49] A genetic link has been found on chromosome 1 in multiple family members of an individual with anorexia nervosa.[50] An individual who is a first degree relative of someone who has had or currently has an eating disorder is seven to twelve times more likely to have an eating disorder themselves.[53] Twin studies also show that at least a portion of the vulnerability to develop eating disorders can be inherited, and there is evidence to show that there is a genetic locus that shows susceptibility for developing anorexia nervosa.[53] About 50% of eating disorder cases are attributable to genetics.[54] Other cases are due to external reasons or developmental problems.[55] There are also other neurobiological factors at play tied to emotional reactivity and impulsivity that could lead to binging and purging behaviors.[56]
Epigenetics mechanisms are means by which environmental effects alter gene expression via methods such as DNA methylation; these are independent of and do not alter the underlying DNA sequence. They are heritable, but also may occur throughout the lifespan, and are potentially reversible. Dysregulation of dopaminergic neurotransmission due to epigenetic mechanisms has been implicated in various eating disorders.[57] Other candidate genes for epigenetic studies in eating disorders include leptin, pro-opiomelanocortin (POMC) and brain-derived neurotrophic factor (BDNF).[58]
Psychological
Eating disorders are classified as Axis I[59] disorders in the Diagnostic and Statistical Manual of Mental Health Disorders (DSM-IV) published by the American Psychiatric Association. There are various other psychological issues that may factor into eating disorders, some fulfill the criteria for a separate Axis I diagnosis or a personality disorder which is coded Axis II and thus are considered comorbid to the diagnosed eating disorder. Axis II disorders are subtyped into 3 "clusters": A, B and C. The causality between personality disorders and eating disorders has yet to be fully established.[60] Some people have a previous disorder which may increase their vulnerability to developing an eating disorder.[61][62][63] Some develop them afterwards.[64] The severity and type of eating disorder symptoms have been shown to affect comorbidity.[65] The DSM-IV should not be used by laypersons to diagnose themselves even when used by professionals there has been considerable controversy over the diagnostic criteria used for various diagnoses, including eating disorders. There has been controversy over various editions of the DSM including the latest edition, DSM-V, due in May 2013.[66][67][68][69][70]
Cognitive attentional bias
Attentional bias may have an effect on eating disorders. Attentional bias is the preferential attention toward certain types of information in the environment while simultaneously ignoring others. Individuals with eating disorders can be thought to have schemas, knowledge structures, which are dysfunctional as they may bias judgement, thought, behaviour in a manner that is self-destructive or maladaptive.[85] They may have developed a disordered schema which focuses on body size and eating. Thus, this information is given the highest level of importance and overvalued among other cognitive structures. Researchers have found that people who have eating disorders tend to pay more attention to stimuli related to food. For people struggling to recover from an eating disorder or addiction, this tendency to pay attention to certain signals while discounting others can make recovery that much more difficult.[85]
Studies have utilized the Stroop task to assess the probable effect of attentional bias on eating disorders. This may involve separating food and eating words from body shape and weight words. Such studies have found that anorexic subjects were slower to colour name food related words than control subjects.[86] Other studies have noted that individuals with eating disorders have significant attentional biases associated with eating and weight stimuli.[87]
Personality traits
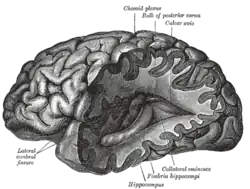
There are various childhood personality traits associated with the development of eating disorders.[88] During adolescence these traits may become intensified due to a variety of physiological and cultural influences such as the hormonal changes associated with puberty, stress related to the approaching demands of maturity and socio-cultural influences and perceived expectations, especially in areas that concern body image. Eating disorders have been associated with a fragile sense of self and with disordered mentalization.[89] Many personality traits have a genetic component and are highly heritable. Maladaptive levels of certain traits may be acquired as a result of anoxic or traumatic brain injury, neurodegenerative diseases such as Parkinson's disease, neurotoxicity such as lead exposure, bacterial infection such as Lyme disease or parasitic infection such as Toxoplasma gondii as well as hormonal influences. While studies are still continuing via the use of various imaging techniques such as fMRI; these traits have been shown to originate in various regions of the brain[90] such as the amygdala[91][92] and the prefrontal cortex.[93] Disorders in the prefrontal cortex and the executive functioning system have been shown to affect eating behavior.[94][95]
Celiac disease
People with gastrointestinal disorders may be more risk of developing disordered eating practices than the general population, principally restrictive eating disturbances.[5] An association of anorexia nervosa with celiac disease has been found.[96] The role that gastrointestinal symptoms play in the development of eating disorders seems rather complex. Some authors report that unresolved symptoms prior to gastrointestinal disease diagnosis may create a food aversion in these persons, causing alterations to their eating patterns. Other authors report that greater symptoms throughout their diagnosis led to greater risk. It has been documented that some people with celiac disease, irritable bowel syndrome or inflammatory bowel disease who are not conscious about the importance of strictly following their diet, choose to consume their trigger foods to promote weight loss. On the other hand, individuals with good dietary management may develop anxiety, food aversion and eating disorders because of concerns around cross contamination of their foods.[5] Some authors suggest that medical professionals should evaluate the presence of an unrecognized celiac disease in all people with eating disorder, especially if they present any gastrointestinal symptom (such as decreased appetite, abdominal pain, bloating, distension, vomiting, diarrhea or constipation), weight loss, or growth failure; and also routinely ask celiac patients about weight or body shape concerns, dieting or vomiting for weight control, to evaluate the possible presence of eating disorders,[96] specially in women.[97]
Environmental influences
Child maltreatment
Child abuse which encompasses physical, psychological and sexual abuse, as well as neglect has been shown to approximately triple the risk of an eating disorder.[98] Sexual abuse appears to about double the risk of bulimia; however, the association is less clear for anorexia.[98]
Social isolation
Social isolation has been shown to have a deleterious effect on an individual's physical and emotional well-being. Those that are socially isolated have a higher mortality rate in general as compared to individuals that have established social relationships. This effect on mortality is markedly increased in those with pre-existing medical or psychiatric conditions, and has been especially noted in cases of coronary heart disease. "The magnitude of risk associated with social isolation is comparable with that of cigarette smoking and other major biomedical and psychosocial risk factors." (Brummett et al.)
Social isolation can be inherently stressful, depressing and anxiety-provoking. In an attempt to ameliorate these distressful feelings an individual may engage in emotional eating in which food serves as a source of comfort. The loneliness of social isolation and the inherent stressors thus associated have been implicated as triggering factors in binge eating as well.[99][100][101][102]
Waller, Kennerley and Ohanian (2007) argued that both bingeing–vomiting and restriction are emotion suppression strategies, but they are just utilized at different times. For example, restriction is used to pre-empt any emotion activation, while bingeing–vomiting is used after an emotion has been activated.[103]
Parental influence
Parental influence has been shown to be an intrinsic component in the development of eating behaviors of children. This influence is manifested and shaped by a variety of diverse factors such as familial genetic predisposition, dietary choices as dictated by cultural or ethnic preferences, the parents' own body shape and eating patterns, the degree of involvement and expectations of their children's eating behavior as well as the interpersonal relationship of parent and child. This is in addition to the general psychosocial climate of the home and the presence or absence of a nurturing stable environment. It has been shown that maladaptive parental behavior has an important role in the development of eating disorders. As to the more subtle aspects of parental influence, it has been shown that eating patterns are established in early childhood and that children should be allowed to decide when their appetite is satisfied as early as the age of two. A direct link has been shown between obesity and parental pressure to eat more.
Coercive tactics in regard to diet have not been proven to be efficacious in controlling a child's eating behavior. Affection and attention have been shown to affect the degree of a child's finickiness and their acceptance of a more varied diet.[104][105][106][107][108][109]
Adams and Crane (1980), have shown that parents are influenced by stereotypes that influence their perception of their child's body. The conveyance of these negative stereotypes also affects the child's own body image and satisfaction.[110] Hilde Bruch, a pioneer in the field of studying eating disorders, asserts that anorexia nervosa often occurs in girls who are high achievers, obedient, and always trying to please their parents. Their parents have a tendency to be over-controlling and fail to encourage the expression of emotions, inhibiting daughters from accepting their own feelings and desires. Adolescent females in these overbearing families lack the ability to be independent from their families, yet realize the need to, often resulting in rebellion. Controlling their food intake may make them feel better, as it provides them with a sense of control.[111]
Peer pressure
In various studies such as one conducted by The McKnight Investigators, peer pressure was shown to be a significant contributor to body image concerns and attitudes toward eating among subjects in their teens and early twenties.
Eleanor Mackey and co-author, Annette M. La Greca of the University of Miami, studied 236 teen girls from public high schools in southeast Florida. "Teen girls' concerns about their own weight, about how they appear to others and their perceptions that their peers want them to be thin are significantly related to weight-control behavior", says psychologist Eleanor Mackey of the Children's National Medical Center in Washington and lead author of the study. "Those are really important."
According to one study, 40% of 9- and 10-year-old girls are already trying to lose weight.[112] Such dieting is reported to be influenced by peer behavior, with many of those individuals on a diet reporting that their friends also were dieting. The number of friends dieting and the number of friends who pressured them to diet also played a significant role in their own choices.[113][114][115][116]
Elite athletes have a significantly higher rate in eating disorders. Female athletes in sports such as gymnastics, ballet, diving, etc. are found to be at the highest risk among all athletes. Women are more likely than men to acquire an eating disorder between the ages of 13–25. 0–15% of those with bulimia and anorexia are men.[117]
Cultural pressure
Western perspective
There is a cultural emphasis on thinness which is especially pervasive in western society. A child's perception of external pressure to achieve the ideal body that is represented by the media predicts the child's body image dissatisfaction, body dysmorphic disorder and an eating disorder.[118] "The cultural pressure on men and women to be 'perfect' is an important predisposing factor for the development of eating disorders".[119][120] Further, when women of all races base their evaluation of their self upon what is considered the culturally ideal body, the incidence of eating disorders increases.[121]
Socioeconomic status (SES) has been viewed as a risk factor for eating disorders, presuming that possessing more resources allows for an individual to actively choose to diet and reduce body weight.[122] Some studies have also shown a relationship between increasing body dissatisfaction with increasing SES.[123] However, once high socioeconomic status has been achieved, this relationship weakens and, in some cases, no longer exists.[124]
The media plays a major role in the way in which people view themselves. Countless magazine ads and commercials depict thin celebrities like Lindsay Lohan, Nicole Richie, Victoria Beckham and Mary Kate Olsen, who appear to gain nothing but attention from their looks. Society has taught people that being accepted by others is necessary at all costs.[125] Unfortunately this has led to the belief that in order to fit in one must look a certain way. Televised beauty competitions such as the Miss America Competition contribute to the idea of what it means to be beautiful because competitors are evaluated on the basis of their opinion.[126]
In addition to socioeconomic status being considered a cultural risk factor so is the world of sports. Athletes and eating disorders tend to go hand in hand, especially the sports where weight is a competitive factor. Gymnastics, horse back riding, wrestling, body building, and dancing are just a few that fall into this category of weight dependent sports. Eating disorders among individuals that participate in competitive activities, especially women, often lead to having physical and biological changes related to their weight that often mimic prepubescent stages. Oftentimes as women's bodies change they lose their competitive edge which leads them to taking extreme measures to maintain their younger body shape. Men often struggle with binge eating followed by excessive exercise while focusing on building muscle rather than losing fat, but this goal of gaining muscle is just as much an eating disorder as obsessing over thinness. The following statistics taken from Susan Nolen-Hoeksema's book, (ab)normal psychology, show the estimated percentage of athletes that struggle with eating disorders based on the category of sport.
- Aesthetic sports (dance, figure skating, gymnastics) – 35%
- Weight dependent sports (judo, wrestling) – 29%
- Endurance sports (cycling, swimming, running) – 20%
- Technical sports (golf, high jumping) – 14%
- Ball game sports (volleyball, soccer) – 12%
Although most of these athletes develop eating disorders to keep their competitive edge, others use exercise as a way to maintain their weight and figure. This is just as serious as regulating food intake for competition. Even though there is mixed evidence showing at what point athletes are challenged with eating disorders, studies show that regardless of competition level all athletes are at higher risk for developing eating disorders that non-athletes, especially those that participate in sports where thinness is a factor.[127]
Pressure from society is also seen within the homosexual community. Homosexual men are at greater risk of eating disorder symptoms than heterosexual men.[128] Within the gay culture, muscularity gives the advantages of both social and sexual desirability and also power.[129] These pressures and ideas that another homosexual male may desire a mate who is thinner or muscular can possibly lead to eating disorders. The higher eating disorder symptom score reported, the more concern about how others perceive them and the more frequent and excessive exercise sessions occur.[129] High levels of body dissatisfaction are also linked to external motivation to working out and old age; however, having a thin and muscular body occurs within younger homosexual males than older.[128][129]
Most of the cross-cultural studies use definitions from the DSM-IV-TR, which has been criticized as reflecting a Western cultural bias. Thus, assessments and questionnaires may not be constructed to detect some of the cultural differences associated with different disorders. Also, when looking at individuals in areas potentially influenced by Western culture, few studies have attempted to measure how much an individual has adopted the mainstream culture or retained the traditional cultural values of the area. Lastly, the majority of the cross-cultural studies on eating disorders and body image disturbances occurred in Western nations and not in the countries or regions being examined.[11]
While there are many influences to how an individual processes their body image, the media does play a major role. Along with the media, parental influence, peer influence, and self-efficacy beliefs also play a large role in an individual's view of themselves. The way the media presents images can have a lasting effect on an individual's perception of their body image. Eating disorders are a worldwide issue and while women are more likely to be affected by an eating disorder it still affects both genders (Schwitzer 2012). The media influences eating disorders whether shown in a positive or negative light, it then has a responsibility to use caution when promoting images that projects an ideal that many turn to eating disorders to attain.[130]
To try to address unhealthy body image in the fashion world, in 2015, France passed a law requiring models to be declared healthy by a doctor to participate in fashion shows. It also requires re-touched images to be marked as such in magazines.[131]
There is a relationship between “thin ideal” social media content and body dissatisfaction and eating disorders among young adult women, especially in the Western hemisphere.[132] New research points to an “internalization” of distorted images online, as well as negative comparisons among young adult women.[133] Most studies have been based in the U.S, the U.K, and Australia, these are places where the thin ideal is strong among women, as well as the strive for the “perfect” body.[133]
In addition to mere media exposure, there is an online “pro-eating disorder” community. Through personal blogs and Twitter, this community promotes eating disorders as a “lifestyle”, and continuously posts pictures of emaciated bodies, and tips on how to stay thin. The hashtag “#proana” (pro-anorexia), is a product of this community,[134] as well as images promoting weight loss, tagged with the term “thinspiration”. According to social comparison theory, young women have a tendency to compare their appearance to others, which can result in a negative view of their own bodies and altering of eating behaviors, that in turn can develop disordered eating behaviors.[135]
When body parts are isolated and displayed in the media as objects to be looked at, it is called objectification, and women are affected most by this phenomenon. Objectification increases self-objectification, where women judge their own body parts as a mean of praise and pleasure for others. There is a significant link between self-objectification, body dissatisfaction, and disordered eating, as the beauty ideal is altered through social media.[132]
African perspective
In the majority of many African communities, thinness is generally not seen as an ideal body type and most pressure to attain a slim figure may stem from influence or exposure to Western culture and ideology. Traditional African cultural ideals are reflected in the practice of some health professionals; in Ghana, pharmacists sell appetite stimulants to women who desire to, as Ghanaians stated, “grow fat”.[136] Girls are told that if they wish to find a partner and birth children they must gain weight. On the contrary, there are certain taboos surrounding a slim body image, specifically in West Africa. Lack of body fat is linked to poverty and HIV/AIDS.[137]
However, the emergence of Western and European influence, specifically with the introduction of such fashion and modelling shows and competitions, is changing certain views among body acceptance, and the prevalence of eating disorders has consequently increased.[137] This acculturation is also related to how South Africa is concurrently undergoing rapid, intense urbanization. Such modern development is leading to cultural changes, and professionals cite rates of eating disorders in this region will increase with urbanization, specifically with changes in identity, body image, and cultural issues.[138] Further, exposure to Western values through private Caucasian schools or caretakers is another possible factor related to acculturation which may be associated with the onset of eating disorders.[139]
Other factors which are cited to be related to the increasing prevalence of eating disorders in African communities can be related to sexual conflicts, such as psychosexual guilt, first sexual intercourse, and pregnancy. Traumatic events which are related to both family (i.e. parental separation) and eating related issues are also cited as possible effectors.[139] Religious fasting, particularly around times of stress, and feelings of self-control are also cited as determinants in the onset of eating disorders.[140]
Asian perspective
The West plays a role in Asia's economic development via foreign investments, advanced technologies joining financial markets, and the arrival of American and European companies in Asia, especially through outsourcing manufacturing operations.[141] This exposure to Western culture, especially the media, imparts Western body ideals to Asian society, termed Westernization.[141] In part, Westernization fosters eating disorders among Asian populations.[141] However, there are also country-specific influences on the occurrence of eating disorders in Asia.[141]
China
In China as well as other Asian countries, Westernization, migration from rural to urban areas, after-effects of sociocultural events, and disruptions of social and emotional support are implicated in the emergence of eating disorders.[141] In particular, risk factors for eating disorders include higher socioeconomic status, preference for a thin body ideal, history of child abuse, high anxiety levels, hostile parental relationships, jealousy towards media idols, and above-average scores on the body dissatisfaction and interoceptive awareness sections of the Eating Disorder Inventory.[142] Similarly to the West, researchers have identified the media as a primary source of pressures relating to physical appearance, which may even predict body change behaviors in males and females.[141]
Hong Kong
From the early- to-mid- 1990s, a variant form of anorexia nervosa was identified in Hong Kong.[143] This variant form did not share features of anorexia in the West, notably “fat-phobia” and distorted body image.[143] Patients attributed their restrictive food intake to somatic complaints, such as epigastric bloating, abdominal or stomach pain, or a lack of hunger or appetite.[141] Compared to Western patients, individuals with this variant anorexia demonstrated bulimic symptoms less frequently and tended to have lower pre-morbid body mass index.[141] This form disapproves the assumption that a “fear of fatness or weight gain” is the defining characteristic of individuals with anorexia nervosa.[143]
India
In the past, the available evidence did not suggest that unhealthy weight loss methods and eating disordered behaviors are common in India as proven by stagnant rates of clinically diagnosed eating disorders.[144] However, it appears that rates of eating disorders in urban areas of India are increasing based on surveys from psychiatrists who were asked whether they perceived eating disorders to be a “serious clinical issue” in India.[141] 23.5% of respondents believed that rates of eating disorders were rising in Bangalore, 26.5% claimed that rates were stagnant, and 42%, the largest percentage, expressed uncertainty. It has been suggested that urbanization and socioeconomic status are associated with increased risk for body weight dissatisfaction.[141] However, due to the physical size of and diversity within India, trends may vary throughout the country.[141]
Mechanisms
- Biochemical: Eating behavior is a complex process controlled by the neuroendocrine system, of which the Hypothalamus-pituitary-adrenal-axis (HPA axis) is a major component. Dysregulation of the HPA axis has been associated with eating disorders,[145][146] such as irregularities in the manufacture, amount or transmission of certain neurotransmitters, hormones[147] or neuropeptides[148] and amino acids such as homocysteine, elevated levels of which are found in AN and BN as well as depression.[149]
- Serotonin: a neurotransmitter involved in depression also has an inhibitory effect on eating behavior.[150][151][152][153][154]
- Norepinephrine is both a neurotransmitter and a hormone; abnormalities in either capacity may affect eating behavior.[155][156]
- Dopamine: which in addition to being a precursor of norepinephrine and epinephrine is also a neurotransmitter which regulates the rewarding property of food.[157][158]
- Neuropeptide Y also known as NPY is a hormone that encourages eating and decreases metabolic rate.[159] Blood levels of NPY are elevated in patients with anorexia nervosa, and studies have shown that injection of this hormone into the brain of rats with restricted food intake increases their time spent running on a wheel. Normally the hormone stimulates eating in healthy patients, but under conditions of starvation it increases their activity rate, probably to increase the chance of finding food.[159] The increased levels of NPY in the blood of patients with eating disorders can in some ways explain the instances of extreme over-exercising found in most anorexia nervosa patients.
- Leptin and ghrelin: leptin is a hormone produced primarily by the fat cells in the body; it has an inhibitory effect on appetite by inducing a feeling of satiety. Ghrelin is an appetite inducing hormone produced in the stomach and the upper portion of the small intestine. Circulating levels of both hormones are an important factor in weight control. While often associated with obesity, both hormones and their respective effects have been implicated in the pathophysiology of anorexia nervosa and bulimia nervosa.[160] Leptin can also be used to distinguish between constitutional thinness found in a healthy person with a low BMI and an individual with anorexia nervosa.[49][161]
- Gut bacteria and immune system: studies have shown that a majority of patients with anorexia and bulimia nervosa have elevated levels of autoantibodies that affect hormones and neuropeptides that regulate appetite control and the stress response. There may be a direct correlation between autoantibody levels and associated psychological traits.[162][163] Later study revealed that autoantibodies reactive with alpha-MSH are, in fact, generated against ClpB, a protein produced by certain gut bacteria e.g. Escherichia coli. ClpB protein was identified as a conformational antigen-mimetic of alpha-MSH. In patients with eating disorders plasma levels of anti-ClpB IgG and IgM correalated with patients' psychological traits[164]
- Infection: PANDAS, is an abbreviation for Pediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococcal Infections. Children with PANDAS "have obsessive-compulsive disorder (OCD) and/or tic disorders such as Tourette syndrome, and in whom symptoms worsen following infections such as "strep throat" and scarlet fever". (NIMH) There is a possibility that PANDAS may be a precipitating factor in the development of anorexia nervosa in some cases, (PANDAS AN).[165]
- Lesions: studies have shown that lesions to the right frontal lobe or temporal lobe can cause the pathological symptoms of an eating disorder.[166][167][168]
- Tumors: tumors in various regions of the brain have been implicated in the development of abnormal eating patterns.[169][170][171][172][173]
- Brain calcification: a study highlights a case in which prior calcification of the right thalumus may have contributed to development of anorexia nervosa.[174]
- somatosensory homunculus: is the representation of the body located in the somatosensory cortex, first described by renowned neurosurgeon Wilder Penfield. The illustration was originally termed "Penfield's Homunculus", homunculus meaning little man. "In normal development this representation should adapt as the body goes through its pubertal growth spurt. However, in AN it is hypothesized that there is a lack of plasticity in this area, which may result in impairments of sensory processing and distortion of body image". (Bryan Lask, also proposed by VS Ramachandran)
- Obstetric complications: There have been studies done which show maternal smoking, obstetric and perinatal complications such as maternal anemia, very pre-term birth (less than 32 weeks), being born small for gestational age, neonatal cardiac problems, preeclampsia, placental infarction and sustaining a cephalhematoma at birth increase the risk factor for developing either anorexia nervosa or bulimia nervosa. Some of this developmental risk as in the case of placental infarction, maternal anemia and cardiac problems may cause intrauterine hypoxia, umbilical cord occlusion or cord prolapse may cause ischemia, resulting in cerebral injury, the prefrontal cortex in the fetus and neonate is highly susceptible to damage as a result of oxygen deprivation which has been shown to contribute to executive dysfunction, ADHD, and may affect personality traits associated with both eating disorders and comorbid disorders such as impulsivity, mental rigidity and obsessionality. The problem of perinatal brain injury, in terms of the costs to society and to the affected individuals and their families, is extraordinary. (Yafeng Dong, PhD)[175][176][177][178][179][180][181][182][183][184][185]
- Symptom of starvation: Evidence suggests that the symptoms of eating disorders are actually symptoms of the starvation itself, not of a mental disorder. In a study involving thirty-six healthy young men that were subjected to semi-starvation, the men soon began displaying symptoms commonly found in patients with eating disorders.[159][186] In this study, the healthy men ate approximately half of what they had become accustomed to eating and soon began developing symptoms and thought patterns (preoccupation with food and eating, ritualistic eating, impaired cognitive ability, other physiological changes such as decreased body temperature) that are characteristic symptoms of anorexia nervosa.[159] The men used in the study also developed hoarding and obsessive collecting behaviors, even though they had no use for the items, which revealed a possible connection between eating disorders and obsessive compulsive disorder.[159]
Diagnosis
The initial diagnosis should be made by a competent medical professional. "The medical history is the most powerful tool for diagnosing eating disorders"(American Family Physician).[187] There are many medical disorders that mimic eating disorders and comorbid psychiatric disorders. All organic causes should be ruled out prior to a diagnosis of an eating disorder or any other psychiatric disorder. In the past 30 years eating disorders have become increasingly conspicuous and it is uncertain whether the changes in presentation reflect a true increase. Anorexia nervosa and bulimia nervosa are the most clearly defined subgroups of a wider range of eating disorders. Many patients present with subthreshold expressions of the two main diagnoses: others with different patterns and symptoms.[188]
Medical
The diagnostic workup typically includes complete medical and psychosocial history and follows a rational and formulaic approach to the diagnosis. Neuroimaging using fMRI, MRI, PET and SPECT scans have been used to detect cases in which a lesion, tumor or other organic condition has been either the sole causative or contributory factor in an eating disorder. "Right frontal intracerebral lesions with their close relationship to the limbic system could be causative for eating disorders, we therefore recommend performing a cranial MRI in all patients with suspected eating disorders" (Trummer M et al. 2002), "intracranial pathology should also be considered however certain is the diagnosis of early-onset anorexia nervosa. Second, neuroimaging plays an important part in diagnosing early-onset anorexia nervosa, both from a clinical and a research prospective".(O'Brien et al. 2001).[168][189]
Psychological
| Eating Attitudes Test[190] | SCOFF questionnaire[191] |
| Body Attitudes Test[192] | Body Attitudes Questionnaire[193] |
| Eating Disorder Inventory[194] | Eating Disorder Examination Interview[195] |
After ruling out organic causes and the initial diagnosis of an eating disorder being made by a medical professional, a trained mental health professional aids in the assessment and treatment of the underlying psychological components of the eating disorder and any comorbid psychological conditions. The clinician conducts a clinical interview and may employ various psychometric tests. Some are general in nature while others were devised specifically for use in the assessment of eating disorders. Some of the general tests that may be used are the Hamilton Depression Rating Scale[196] and the Beck Depression Inventory.[197][198] longitudinal research showed that there is an increase in chance that a young adult female would develop bulimia due to their current psychological pressure and as the person ages and matures, their emotional problems change or are resolved and then the symptoms decline.[199]
Differential diagnoses
There are multiple medical conditions which may be misdiagnosed as a primary psychiatric disorder, complicating or delaying treatment. These may have a synergistic effect on conditions which mimic an eating disorder or on a properly diagnosed eating disorder.
- Lyme disease is known as the "great imitator", as it may present as a variety of psychiatric or neurological disorders including anorexia nervosa.[200][201]
- Gastrointestinal diseases,[5] such as celiac disease, Crohn's disease, peptic ulcer, eosinophilic esophagitis[96] or non-celiac gluten sensitivity,[202] among others. Celiac disease is also known as the "great imitator", because it may involve several organs and cause an extensive variety of non-gastrointestinal symptoms, such as psychiatric and neurological disorders,[203][204][205] including anorexia nervosa.[96]
- Addison's disease is a disorder of the adrenal cortex which results in decreased hormonal production. Addison's disease, even in subclinical form may mimic many of the symptoms of anorexia nervosa.[206]
- Gastric adenocarcinoma is one of the most common forms of cancer in the world. Complications due to this condition have been misdiagnosed as an eating disorder.[207]
- Hypothyroidism, hyperthyroidism, hypoparathyroidism and hyperparathyroidism may mimic some of the symptoms of, can occur concurrently with, be masked by or exacerbate an eating disorder.[208][209][210][211][212][213][214][215]
- Toxoplasma seropositivity: even in the absence of symptomatic toxoplasmosis, toxoplasma gondii exposure has been linked to changes in human behavior and psychiatric disorders including those comorbid with eating disorders such as depression. In reported case studies the response to antidepressant treatment improved only after adequate treatment for toxoplasma.[216]
- Neurosyphilis: It is estimated that there may be up to one million cases of untreated syphilis in the US alone. "The disease can present with psychiatric symptoms alone, psychiatric symptoms that can mimic any other psychiatric illness". Many of the manifestations may appear atypical. Up to 1.3% of short term psychiatric admissions may be attributable to neurosyphilis, with a much higher rate in the general psychiatric population. (Ritchie, M Perdigao J,)[217]
- Dysautonomia: a wide variety of autonomic nervous system (ANS) disorders may cause a wide variety of psychiatric symptoms including anxiety, panic attacks and depression. Dysautonomia usually involves failure of sympathetic or parasympathetic components of the ANS system but may also include excessive ANS activity. Dysautonomia can occur in conditions such as diabetes and alcoholism.
Psychological disorders which may be confused with an eating disorder, or be co-morbid with one:
- Emetophobia is an anxiety disorder characterized by an intense fear of vomiting. A person so afflicted may develop rigorous standards of food hygiene, such as not touching food with their hands. They may become socially withdrawn to avoid situations which in their perception may make them vomit. Many who have emetophobia are diagnosed with anorexia or self-starvation. In severe cases of emetophobia they may drastically reduce their food intake.[218][219]
- Phagophobia is an anxiety disorder characterized by a fear of eating, it is usually initiated by an adverse experience while eating such as choking or vomiting. Persons with this disorder may present with complaints of pain while swallowing.[220]
- Body dysmorphic disorder (BDD) is listed as a somatoform disorder that affects up to 2% of the population. BDD is characterized by excessive rumination over an actual or perceived physical flaw. BDD has been diagnosed equally among men and women. While BDD has been misdiagnosed as anorexia nervosa, it also occurs comorbidly in 39% of eating disorder cases. BDD is a chronic and debilitating condition which may lead to social isolation, major depression and suicidal ideation and attempts. Neuroimaging studies to measure response to facial recognition have shown activity predominately in the left hemisphere in the left lateral prefrontal cortex, lateral temporal lobe and left parietal lobe showing hemispheric imbalance in information processing. There is a reported case of the development of BDD in a 21-year-old male following an inflammatory brain process. Neuroimaging showed the presence of a new atrophy in the frontotemporal region.[221][222][223][224]
Prevention
Prevention aims to promote a healthy development before the occurrence of eating disorders. It also intends early identification of an eating disorder before it is too late to treat. Children as young as ages 5–7 are aware of the cultural messages regarding body image and dieting.[225] Prevention comes in bringing these issues to the light. The following topics can be discussed with young children (as well as teens and young adults).
- Emotional Bites: a simple way to discuss emotional eating is to ask children about why they might eat besides being hungry. Talk about more effective ways to cope with emotions, emphasizing the value of sharing feelings with a trusted adult.[226]
- Say No to Teasing: another concept is to emphasize that it is wrong to say hurtful things about other people's body sizes.[227]
- Body Talk: emphasize the importance of listening to one's body. That is, eating when you are hungry (not starving) and stopping when you are satisfied (not stuffed). Children intuitively grasp these concepts.[226]
- Fitness Comes in All Sizes: educate children about the genetics of body size and the normal changes occurring in the body. Discuss their fears and hopes about growing bigger. Focus on fitness and a balanced diet.[228]
Internet and modern technologies provide new opportunities for prevention. On-line programs have the potential to increase the use of prevention programs.[229] The development and practice of prevention programs via on-line sources make it possible to reach a wide range of people at minimal cost.[230] Such an approach can also make prevention programs to be sustainable.
Treatment
Treatment varies according to type and severity of eating disorder, and usually more than one treatment option is utilized.[231] Family doctors play an important role in early treatment of people with eating disorders by encouraging those who are also reluctant to see a psychiatrist.[232] Treatment can take place in a variety of different settings such as community programs, hospitals, day programs, and groups.[233] The American Psychiatric Association (APA) recommends a team approach to treatment of eating disorders. The members of the team are usually a psychiatrist, therapist, and registered dietitian, but other clinicians may be included.[234]
That said, some treatment methods are:
- Cognitive behavioral therapy (CBT),[235][236][237] which postulates that an individual's feelings and behaviors are caused by their own thoughts instead of external stimuli such as other people, situations or events; the idea is to change how a person thinks and reacts to a situation even if the situation itself does not change. See Cognitive behavioral treatment of eating disorders.
- The Maudsley anorexia nervosa treatment for adults (MANTRA), which focuses on addressing rigid information processing styles, emotional avoidance, pro-anorectic beliefs, and difficulties with interpersonal relationships.[243] These four targets of treatment are proposed to be core maintenance factors within the Cognitive-Interpersonal Maintenance Model of anorexia nervosa.[244]
- Dialectical behavior therapy[245]
- Family therapy[246] including "conjoint family therapy" (CFT), "separated family therapy" (SFT) and Maudsley Family Therapy.[247][248]
- Behavioral therapy: focuses on gaining control and changing unwanted behaviors.[249]
- Interpersonal psychotherapy (IPT)[250]
- Cognitive Emotional Behaviour Therapy (CEBT)[251]
- Art therapy[252]
- Nutrition counseling[253] and Medical nutrition therapy[254][255][256]
- Medication: Orlistat is used in obesity treatment. Olanzapine seems to promote weight gain as well as the ability to ameliorate obsessional behaviors concerning weight gain. zinc supplements have been shown to be helpful, and cortisol is also being investigated.[257][258][259][260][261][262]
- Self-help and guided self-help have been shown to be helpful in AN, BN and BED;[237][263][264][265] this includes support groups and self-help groups such as Eating Disorders Anonymous and Overeaters Anonymous.[266][267]
- Psychoanalysis
- Inpatient care
There are few studies on the cost-effectiveness of the various treatments.[268] Treatment can be expensive;[269][270] due to limitations in health care coverage, people hospitalized with anorexia nervosa may be discharged while still underweight, resulting in relapse and rehospitalization.[271]
For children with anorexia, the only well-established treatment is the family treatment-behavior.[272] For other eating disorders in children, however, there is no well-established treatments, though family treatment-behavior has been used in treating bulimia.[272]
A 2019 Cochrane review of the effectiveness of inpatient versus outpatient models of care for eating disorders was unable to draw any definitive conclusions as to the superiority of one model over another.[273]
Outcomes
For anorexia nervosa, bulimia nervosa, and binge eating disorder, there is a general agreement that full recovery rates are in the 50% to 85% range, with larger proportions of people experiencing at least partial remission.[266][274][275][276] It can be a lifelong struggle or it can be overcome within months.
- Miscarriages: Pregnant women with a binge eating disorder have shown to have a greater chance of having a miscarriage compared to pregnant women with any other eating disorders. According to a study done, out of a group of pregnant women being evaluated, 46.7% of the pregnancies ended with a miscarriage in women that were diagnosed with BED, with 23.0% in the control. In the same study, 21.4% of women diagnosed with Bulimia Nervosa had their pregnancies end with miscarriages and only 17.7% of the controls.[277]
- Relapse: An individual who is in remission from BN and EDNOS (Eating Disorder Not Otherwise Specified) is at a high risk of falling back into the habit of self-harm. Factors such as high stress regarding their job, pressures from society, as well as other occurrences that inflict stress on a person, can push a person back to what they feel will ease the pain. A study tracked a group of selected people that were either diagnosed with BN or EDNOS for 60 months. After the 60 months were complete, the researchers recorded whether or not the person was having a relapse. The results found that the probability of a person previously diagnosed with EDNOS had a 41% chance of relapsing; a person with BN had a 47% chance.[278]
- Attachment insecurity: People who are showing signs of attachment anxiety will most likely have trouble communicating their emotional status as well as having trouble seeking effective social support. Signs that a person has adopted this symptom include not showing recognition to their caregiver or when he/she is feeling pain. In a clinical sample, it is clear that at the pretreatment step of a patient's recovery, more severe eating disorder symptoms directly corresponds to higher attachment anxiety. The more this symptom increases, the more difficult it is to achieve eating disorder reduction prior to treatment.[279]
Anorexia symptoms include the increasing chance of getting osteoporosis. Thinning of the hair as well as dry hair and skin are also very common. The muscles of the heart will also start to change if no treatment is inflicted on the patient. This causes the heart to have an abnormally slow heart rate along with low blood pressure. Heart failure becomes a major consideration when this begins to occur.[280] Muscles throughout the body begin to lose their strength. This will cause the individual to begin feeling faint, drowsy, and weak. Along with these symptoms, the body will begin to grow a layer of hair called lanugo. The human body does this in response to the lack of heat and insulation due to the low percentage of body fat.[281]
Bulimia symptoms include heart problems like an irregular heartbeat that can lead to heart failure and death may occur. This occurs because of the electrolyte imbalance that is a result of the constant binge and purge process. The probability of a gastric rupture increases. A gastric rupture is when there is a sudden rupture of the stomach lining that can be fatal.The acids that are contained in the vomit can cause a rupture in the esophagus as well as tooth decay. As a result, to laxative abuse, irregular bowel movements may occur along with constipation. Sores along the lining of the stomach called peptic ulcers begin to appear and the chance of developing pancreatitis increases.[281]
Binge eating symptoms include high blood pressure, which can cause heart disease if it is not treated. Many patients recognize an increase in the levels of cholesterol. The chance of being diagnosed with gallbladder disease increases, which affects an individual's digestive tract.[281]
Risk of death
Eating disorders result in about 7,000 deaths a year as of 2010, making them the mental illnesses with the highest mortality rate.[282] Anorexia has a risk of death that is increased about 5 fold with 20% of these deaths as a result of suicide.[283] Rates of death in bulemia and other disorders are similar at about a 2 fold increase.[283]
The mortality rate for those with anorexia is 5.4 per 1000 individuals per year. Roughly 1.3 deaths were due to suicide. A person who is or had been in an inpatient setting had a rate of 4.6 deaths per 1000. Of individuals with bulimia about 2 persons per 1000 persons die per year and among those with EDNOS about 3.3 per 1000 people die per year.[283]
Epidemiology
In the developed world, binge eating disorder affects about 1.6% of women and 0.8% of men in a given year.[1] Anorexia affects about 0.4% and bulimia affects about 1.3% of young women in a given year.[1] Up to 4% of women have anorexia, 2% have bulimia, and 2% have binge eating disorder at some point in time.[8] Anorexia and bulimia occur nearly ten times more often in females than males.[1] Typically, they begin in late childhood or early adulthood.[2] Rates of other eating disorders are not clear.[1] Rates of eating disorders appear to be lower in less developed countries.[9]
In the United States, twenty million women and ten million men have an eating disorder at least once in their lifetime.[281]
Error: Dataset name contains invalid characters.

Anorexia
Rates of anorexia in the general population among women aged 11 to 65 ranges from 0 to 2.2% and around 0.3% among men.[284] The incidence of female cases is low in general medicine or specialized consultation in town, ranging from 4.2 and 8.3/100,000 individuals per year.[284] The incidence of AN ranges from 109 to 270/100,000 individuals per year.[284] Mortality varies according to the population considered.[284] AN has one of the highest mortality rates among mental illnesses.[284] The rates observed are 6.2 to 10.6 times greater than that observed in the general population for follow-up periods ranging from 13 to 10 years.[284] Standardized mortality ratios for anorexia vary from 1.36% to 20%.[285]
Bulimia
Bulimia affects females 9 times more often than males.[286] Approximately one to three percent women develop bulimia in their lifetime.[286] About 2% to 3% of women are currently affected in the United States.[287] New cases occur in about 12 per 100,000 population per year.[288] The standardized mortality ratios for bulimia is 1% to 3%.[285]
Binge eating disorder
Reported rates vary from 1.3 to 30% among subjects seeking weight-loss treatment.[289] Based on surveys, BED appears to affected about 1-2% at some point in their life, with 0.1-1% of people affected in a given year.[290] BED is more common among females than males.[289] There have been no published studies investigating the effects of BED on mortality, although it is comorbid with disorders that are known to increase mortality risks.[290]
Economics
- Since 2017, the number of cost-effectiveness studies regarding eating disorders appears to be increasing in the past six years.[291]
- In 2011 United States dollars, annual healthcare costs were $1,869 greater among individuals with eating disorders compared to the general population.[292] The added presence of mental health comorbidities was also associated with higher, but not statistically significant, costs difference of $1,993.[292]
- In 2013 Canadian dollars, the total hospital cost per admission for treatment of anorexia nervosa was $51,349 and the total societal cost was $54,932 based on an average length of stay of 37.9 days.[293] For every unit increase in body mass index, there was also a 15.7% decrease in hospital cost.[293]
- For Ontario, Canada patients who received specialized inpatient care for an eating disorder both out of country and in province, annual total healthcare costs were about $11 million before 2007 and $6.5 million in the years afterwards.[294] For those treated out of country alone, costs were about $5 million before 2007 and $2 million in the years afterwards.[294]
See also
References
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 American Psychiatric Association (2013). Diagnostic and Statistical Manual of Mental Disorders (5th ed.). Arlington, VA: American Psychiatric Association. pp. 329–354. ISBN 978-0-89042-555-8.
- 1 2 3 4 5 6 7 8 9 10 "What are Eating Disorders?". NIMH. Archived from the original on 23 May 2015. Retrieved 24 May 2015.
- 1 2 3 Rikani AA, Choudhry Z, Choudhry AM, Ikram H, Asghar MW, Kajal D, et al. (October 2013). "A critique of the literature on etiology of eating disorders". Annals of Neurosciences. 20 (4): 157–61. doi:10.5214/ans.0972.7531.200409. PMC 4117136. PMID 25206042.
- 1 2 Arcelus J, Witcomb GL, Mitchell A (March 2014). "Prevalence of eating disorders amongst dancers: a systemic review and meta-analysis". European Eating Disorders Review. 22 (2): 92–101. doi:10.1002/erv.2271. PMID 24277724.
- 1 2 3 4 Satherley R, Howard R, Higgs S (January 2015). "Disordered eating practices in gastrointestinal disorders" (PDF). Appetite (Review). 84: 240–50. doi:10.1016/j.appet.2014.10.006. PMID 25312748. Archived from the original (PDF) on 2019-09-24. Retrieved 2019-09-24.
- 1 2 Chen LP, Murad MH, Paras ML, Colbenson KM, Sattler AL, Goranson EN, et al. (July 2010). "Sexual abuse and lifetime diagnosis of psychiatric disorders: systematic review and meta-analysis". Mayo Clinic Proceedings. 85 (7): 618–29. doi:10.4065/mcp.2009.0583. PMC 2894717. PMID 20458101.
- ↑ McNamee, Mike (2014). Sport, Medicine, Ethics. Routledge. p. 115. ISBN 9781134618330. Archived from the original on 2020-08-01. Retrieved 2020-08-02.
- 1 2 3 4 5 Smink FR, van Hoeken D, Hoek HW (November 2013). "Epidemiology, course, and outcome of eating disorders". Current Opinion in Psychiatry. 26 (6): 543–8. doi:10.1097/yco.0b013e328365a24f. PMID 24060914.
- 1 2 Pike KM, Hoek HW, Dunne PE (November 2014). "Cultural trends and eating disorders". Current Opinion in Psychiatry. 27 (6): 436–42. doi:10.1097/yco.0000000000000100. PMID 25211499.
- ↑ Nolen-Hoeksma (2014). Abnormal Psychology (6th ed.). US: McGraw-Hill. p. 339. ISBN 978-1-308-21150-3.
- 1 2 3 Mash, Eric Jay; Wolfe, David Allen (2010). "Eating Disorders and Related Conditions". Abnormal Child Psychology. Belmont, CA: Wadsworth: Cengage Learning. pp. 415–26. ISBN 978-0-495-50627-0.
{{cite book}}:|access-date=requires|url=(help);|archive-url=requires|url=(help); Unknown parameter|chapterurl=ignored (help) - ↑ Yale, Susan Nolen-Hoeksema (2014). Abnormal psychology (6th ed.). New York, NY: McGraw Hill Education. pp. 340–341. ISBN 978-0-07-803538-8.
- ↑ Thompson, S.B.N. "Eating disorders: a guide for health professionals." London: Chapman & Hall 1993."
- ↑ Striegel-Moore RH, Franko DL (2008). "Should binge eating disorder be included in the DSM-V? A critical review of the state of the evidence". Annual Review of Clinical Psychology. 4: 305–24. doi:10.1146/annurev.clinpsy.4.022007.141149. PMID 18370619.
- ↑ Teaching Students with Mental Health Disorders: Resources for Teachers. Victoria: British Columbia Ministry of Education, Special Programs Branch, 2001. Print.
- ↑ Fisher MM, Rosen DS, Ornstein RM, Mammel KA, Katzman DK, Rome ES, et al. (July 2014). "Characteristics of avoidant/restrictive food intake disorder in children and adolescents: a "new disorder" in DSM-5". The Journal of Adolescent Health. 55 (1): 49–52. doi:10.1016/j.jadohealth.2013.11.013. PMID 24506978.
- ↑ Saunders, Ronna (2004). ""Grazing": A High-Risk Behavior". Obesity Surgery. 14 (1): 98–102. doi:10.1381/096089204772787374. PMID 14980042.
- ↑ Barry AE, Piazza-Gardner AK (2012). "Drunkorexia: understanding the co-occurrence of alcohol consumption and eating/exercise weight management behaviors". Journal of American College Health. 60 (3): 236–43. doi:10.1080/07448481.2011.587487. PMID 22420701.
- ↑ Tarren-Sweeney M, Hazell P (March 2006). "Mental health of children in foster and kinship care in New South Wales, Australia". Journal of Paediatrics and Child Health. 42 (3): 89–97. doi:10.1111/j.1440-1754.2006.00804.x. PMID 16509906.
- ↑ Regard M, Landis T (May 1997). ""Gourmand syndrome": eating passion associated with right anterior lesions". Neurology. 48 (5): 1185–90. doi:10.1212/wnl.48.5.1185. PMID 9153440.
- ↑ Too Much #Fitspo: When Healthy Eating Becomes an Eating Disorder Archived 2015-07-11 at the Wayback Machine, Glammonitor.com, 2015-4-29
- ↑ Mathieu J (June 2009). "What is pregorexia?". Journal of the American Dietetic Association. 109 (6): 976–9. doi:10.1016/j.jada.2009.04.021. PMID 19465173.
- ↑ Strumia R (2005). "Dermatologic signs in patients with eating disorders". American Journal of Clinical Dermatology. 6 (3): 165–73. doi:10.2165/00128071-200506030-00003. PMID 15943493.
- ↑ Joyce JM, Warren DL, Humphries LL, Smith AJ, Coon JS (March 1990). "Osteoporosis in women with eating disorders: comparison of physical parameters, exercise, and menstrual status with SPA and DPA evaluation". Journal of Nuclear Medicine. 31 (3): 325–31. PMID 2308003.
- ↑ Drevelengas A, Chourmouzi D, Pitsavas G, Charitandi A, Boulogianni G (October 2001). "Reversible brain atrophy and subcortical high signal on MRI in a patient with anorexia nervosa". Neuroradiology. 43 (10): 838–40. doi:10.1007/s002340100589. PMID 11688699.
- ↑ Addolorato G, Taranto C, Capristo E, Gasbarrini G (December 1998). "A case of marked cerebellar atrophy in a woman with anorexia nervosa and cerebral atrophy and a review of the literature". The International Journal of Eating Disorders. 24 (4): 443–7. doi:10.1002/(SICI)1098-108X(199812)24:4<443::AID-EAT13>3.0.CO;2-4. PMID 9813771.
- ↑ Jagielska G, Tomaszewicz-Libudzic EC, Brzozowska A (October 2007). "Pellagra: a rare complication of anorexia nervosa". European Child & Adolescent Psychiatry. 16 (7): 417–20. doi:10.1007/s00787-007-0613-4. PMID 17712518.
- ↑ Pompili M, Mancinelli I, Girardi P, Accorrà D, Ruberto A, Tatarelli R (2003). "[Suicide and attempted suicide in anorexia nervosa and bulimia nervosa]". Annali dell'Istituto Superiore di Sanita. 39 (2): 275–81. PMID 14587228.
- ↑ Franko DL, Keel PK, Dorer DJ, Blais MA, Delinsky SS, Eddy KT, et al. (July 2004). "What predicts suicide attempts in women with eating disorders?". Psychological Medicine. 34 (5): 843–53. doi:10.1017/S0033291703001545. PMID 15500305.
- ↑ Fedorowicz VJ, Falissard B, Foulon C, Dardennes R, Divac SM, Guelfi JD, Rouillon F (November 2007). "Factors associated with suicidal behaviors in a large French sample of inpatients with eating disorders". The International Journal of Eating Disorders. 40 (7): 589–95. doi:10.1002/eat.20415. PMID 17607699.
- 1 2 Treasure J, Claudino AM, Zucker N (February 2010). "Eating disorders". Lancet. 375 (9714): 583–93. doi:10.1016/S0140-6736(09)61748-7. PMID 19931176.
- ↑ Hirschberg AL, Naessén S, Stridsberg M, Byström B, Holtet J (August 2004). "Impaired cholecystokinin secretion and disturbed appetite regulation in women with polycystic ovary syndrome". Gynecological Endocrinology. 19 (2): 79–87. doi:10.1080/09513590400002300. PMID 15624269.
- ↑ Naessén S, Carlström K, Garoff L, Glant R, Hirschberg AL (July 2006). "Polycystic ovary syndrome in bulimic women--an evaluation based on the new diagnostic criteria". Gynecological Endocrinology. 22 (7): 388–94. doi:10.1080/09513590600847421. PMID 16864149.
- ↑ McCluskey S, Evans C, Lacey JH, Pearce JM, Jacobs H (February 1991). "Polycystic ovary syndrome and bulimia". Fertility and Sterility. 55 (2): 287–91. doi:10.1016/S0015-0282(16)54117-X. PMID 1991526.
- ↑ Jahanfar S, Eden JA, Nguyent TV (June 1995). "Bulimia nervosa and polycystic ovary syndrome". Gynecological Endocrinology. 9 (2): 113–7. doi:10.3109/09513599509160199. PMID 7502686.
- ↑ Morgan JF, McCluskey SE, Brunton JN, Hubert Lacey J (May 2002). "Polycystic ovarian morphology and bulimia nervosa: a 9-year follow-up study". Fertility and Sterility. 77 (5): 928–31. doi:10.1016/S0015-0282(02)03063-7. PMID 12009345.
- ↑ Lujan ME, Chizen DR, Pierson RA (August 2008). "Diagnostic criteria for polycystic ovary syndrome: pitfalls and controversies". Journal of Obstetrics and Gynaecology Canada. 30 (8): 671–679. doi:10.1016/s1701-2163(16)32915-2. PMC 2893212. PMID 18786289.
- 1 2 3 4 Romanos GE, Javed F, Romanos EB, Williams RC (October 2012). "Oro-facial manifestations in patients with eating disorders". Appetite. 59 (2): 499–504. doi:10.1016/j.appet.2012.06.016. PMID 22750232.
- ↑ Gailey, J (2009). "Starving is the most fun a girl can have: The Pro-Ana subculture as edgework". Critical Criminology. 17 (2): 93–108. doi:10.1007/s10612-009-9074-z.
- ↑ Borzekowski DL, Schenk S, Wilson JL, Peebles R (August 2010). "e-Ana and e-Mia: A content analysis of pro-eating disorder Web sites". American Journal of Public Health. 100 (8): 1526–34. doi:10.2105/AJPH.2009.172700. PMC 2901299. PMID 20558807.
- ↑ Wolf M, Theis F, Kordy H (2013). "Language Use in Eating Disorder Blogs: Psychological Implications of Social Online Activity". Journal of Language and Social Psychology. 32 (2): 212–226. doi:10.1177/0261927x12474278.
- 1 2 Treasure, Janet; Cardi, Valentina (2017). "Anorexia Nervosa, Theory and Treatment: Where Are We 35 Years on from Hilde Bruch's Foundation Lecture?". European Eating Disorders Review. 25 (3): 139–147. doi:10.1002/erv.2511. ISSN 1099-0968. PMID 28402069.
- ↑ Tasca, Giorgio A.; Balfour, Louise (November 2014). "Attachment and eating disorders: a review of current research". The International Journal of Eating Disorders. 47 (7): 710–717. doi:10.1002/eat.22302. ISSN 1098-108X. PMID 24862477.
- ↑ Cash, Thomas F.; Deagle, Edwin A. (1997-09-01). "The nature and extent of body‐image disturbances in anorexia nervosa and bulimia nervosa: A meta‐analysis". International Journal of Eating Disorders. 22 (2): 107–126. doi:10.1002/(SICI)1098-108X(199709)22:2<107::AID-EAT1>3.0.CO;2-J. ISSN 1098-108X. PMID 9261648.
- 1 2 Gaudio, Santino; Brooks, Samantha Jane; Riva, Giuseppe (2014-10-10). "Nonvisual Multisensory Impairment of Body Perception in Anorexia Nervosa: A Systematic Review of Neuropsychological Studies". PLOS ONE. 9 (10): e110087. Bibcode:2014PLoSO...9k0087G. doi:10.1371/journal.pone.0110087. ISSN 1932-6203. PMC 4193894. PMID 25303480.
- 1 2 3 4 Cooper, PJ; Fairburn, CG (May 1993). "Confusion over the core psychopathology of bulimia nervosa". The International Journal of Eating Disorders. 13 (4): 385–9. doi:10.1002/1098-108x(199305)13:4<385::aid-eat2260130406>3.0.co;2-w. PMID 8490640.
- 1 2 Ruffolo JS, Phillips KA, Menard W, Fay C, Weisberg RB (January 2006). "Comorbidity of body dysmorphic disorder and eating disorders: severity of psychopathology and body image disturbance". The International Journal of Eating Disorders. 39 (1): 11–9. doi:10.1002/eat.20219. PMID 16254870.
- 1 2 Grant JE, Kim SW, Eckert ED (November 2002). "Body dysmorphic disorder in patients with anorexia nervosa: prevalence, clinical features, and delusionality of body image". The International Journal of Eating Disorders. 32 (3): 291–300. doi:10.1002/eat.10091. PMID 12210643.
- 1 2 3 Bulik CM, Hebebrand J, Keski-Rahkonen A, Klump KL, Reichborn-Kjennerud T, Mazzeo SE, Wade TD (November 2007). "Genetic epidemiology, endophenotypes, and eating disorder classification". The International Journal of Eating Disorders. 40 Suppl: S52-60. doi:10.1002/eat.20398. PMID 17573683. S2CID 36187776.
- 1 2 DeAngelis, T (2002). "A genetic link to anorexia". Monitor on Psychology. 33 (3): 34. Archived from the original on 2019-06-07. Retrieved 2020-08-02.
- 1 2 Klump KL, Kaye WH, Strober M (June 2001). "The evolving genetic foundations of eating disorders". The Psychiatric Clinics of North America. 24 (2): 215–25. doi:10.1016/S0193-953X(05)70218-5. PMID 11416922.
- ↑ Mazzeo SE, Bulik CM (January 2009). "Environmental and genetic risk factors for eating disorders: what the clinician needs to know". Child and Adolescent Psychiatric Clinics of North America. 18 (1): 67–82. doi:10.1016/j.chc.2008.07.003. PMC 2719561. PMID 19014858.
- 1 2 Patel P, Wheatcroft R, Park RJ, Stein A (March 2002). "The children of mothers with eating disorders". Clinical Child and Family Psychology Review. 5 (1): 1–19. doi:10.1023/A:1014524207660. PMID 11993543.
- ↑ Trace SE, Baker JH, Peñas-Lledó E, Bulik CM (2013). "The genetics of eating disorders". Annual Review of Clinical Psychology. 9: 589–620. doi:10.1146/annurev-clinpsy-050212-185546. PMID 23537489. S2CID 33773190.
- ↑ Kadison, Richard (2004). College of the Overwhelmed: The Campus Mental Health Crisis and What to Do About It. San Francisco: Jossey-Bass. pp. 132. ISBN 9780787981143.
- ↑ Iarovici, Doris (2014). Mental Health Issues & the University Student. Baltimore: Johns Hopkins University Press. pp. 104. ISBN 9781421412382.
- ↑ Frieling H, Römer KD, Scholz S, Mittelbach F, Wilhelm J, De Zwaan M, et al. (November 2010). "Epigenetic dysregulation of dopaminergic genes in eating disorders". The International Journal of Eating Disorders. 43 (7): 577–83. doi:10.1002/eat.20745. PMID 19728374.
- ↑ Campbell IC, Mill J, Uher R, Schmidt U (January 2011). "Eating disorders, gene-environment interactions and epigenetics". Neuroscience and Biobehavioral Reviews. 35 (3): 784–93. doi:10.1016/j.neubiorev.2010.09.012. PMID 20888360.
- ↑ Westen D, Harnden-Fischer J (April 2001). "Personality profiles in eating disorders: rethinking the distinction between axis I and axis II". The American Journal of Psychiatry. 158 (4): 547–62. doi:10.1176/appi.ajp.158.4.547. PMID 11282688. S2CID 33162558.
- ↑ Rosenvinge JH, Martinussen M, Ostensen E (June 2000). "The comorbidity of eating disorders and personality disorders: a meta-analytic review of studies published between 1983 and 1998". Eating and Weight Disorders. 5 (2): 52–61. doi:10.1007/bf03327480. PMID 10941603.
- ↑ Kaye WH, Bulik CM, Thornton L, Barbarich N, Masters K (December 2004). "Comorbidity of anxiety disorders with anorexia and bulimia nervosa". The American Journal of Psychiatry. 161 (12): 2215–21. doi:10.1176/appi.ajp.161.12.2215. PMID 15569892. S2CID 9926158.
- ↑ Thornton C, Russell J (January 1997). "Obsessive compulsive comorbidity in the dieting disorders". The International Journal of Eating Disorders. 21 (1): 83–7. doi:10.1002/(SICI)1098-108X(199701)21:1<83::AID-EAT10>3.0.CO;2-P. PMID 8986521.
- ↑ Vitousek K, Manke F (February 1994). "Personality variables and disorders in anorexia nervosa and bulimia nervosa". Journal of Abnormal Psychology. 103 (1): 137–47. doi:10.1037/0021-843X.103.1.137. PMID 8040475.
- ↑ Braun DL, Sunday SR, Halmi KA (November 1994). "Psychiatric comorbidity in patients with eating disorders". Psychological Medicine. 24 (4): 859–67. doi:10.1017/S0033291700028956. PMID 7892354.
- ↑ Spindler A, Milos G (August 2007). "Links between eating disorder symptom severity and psychiatric comorbidity". Eating Behaviors. 8 (3): 364–73. doi:10.1016/j.eatbeh.2006.11.012. PMID 17606234.
- ↑ Collier R (January 2010). "DSM revision surrounded by controversy". CMAJ. 182 (1): 16–7. doi:10.1503/cmaj.109-3108. PMC 2802599. PMID 19920166.
- ↑ Kutchins H, Kirk SA (May 1989). "DSM-III-R: the conflict over new psychiatric diagnoses". Health & Social Work. 14 (2): 91–101. doi:10.1093/hsw/14.2.91. PMID 2714710.
- ↑ Busko, Marlene. "DSM-IV Diagnostic Criteria for Eating Disorders May Be Too Stringent". Medscape. Archived from the original on 2012-05-13.
- ↑ Murdoch CJ (10 September 2009). "The Politics of Disease Definition: A Summer of DSM-V Controversy in Review. Stanford Center for Law and the Biosciences". Archived from the original on 15 September 2010.
- ↑ "Psychiatry manual's secrecy criticized". Los Angeles Times. 29 December 2008. Archived from the original on 23 January 2010.
- ↑ Casper RC (1998). "Depression and eating disorders". Depression and Anxiety. 8 Suppl 1 (Suppl 1): 96–104. doi:10.1002/(SICI)1520-6394(1998)8:1+<96::AID-DA15>3.0.CO;2-4. PMID 9809221.
- ↑ Serpell L, Livingstone A, Neiderman M, Lask B (June 2002). "Anorexia nervosa: obsessive-compulsive disorder, obsessive-compulsive personality disorder, or neither?". Clinical Psychology Review. 22 (5): 647–69. doi:10.1016/S0272-7358(01)00112-X. PMID 12113200.
- ↑ Bulik CM, Klump KL, Thornton L, Kaplan AS, Devlin B, Fichter MM, et al. (July 2004). "Alcohol use disorder comorbidity in eating disorders: a multicenter study". The Journal of Clinical Psychiatry. 65 (7): 1000–6. doi:10.4088/JCP.v65n0718. PMID 15291691.
- ↑ Larsson JO, Hellzén M (September 2004). "Patterns of personality disorders in women with chronic eating disorders". Eating and Weight Disorders. 9 (3): 200–5. doi:10.1007/bf03325067. PMID 15656014.
- ↑ Swinbourne JM, Touyz SW (July 2007). "The co-morbidity of eating disorders and anxiety disorders: a review". European Eating Disorders Review. 15 (4): 253–74. doi:10.1002/erv.784. PMID 17676696.
- ↑ Ronningstam E (1996). "Pathological narcissism and narcissistic personality disorder in Axis I disorders". Harvard Review of Psychiatry. 3 (6): 326–40. doi:10.3109/10673229609017201. PMID 9384963.
- ↑ Anderluh MB, Tchanturia K, Rabe-Hesketh S, Treasure J (February 2003). "Childhood obsessive-compulsive personality traits in adult women with eating disorders: defining a broader eating disorder phenotype". The American Journal of Psychiatry. 160 (2): 242–7. doi:10.1176/appi.ajp.160.2.242. PMID 12562569.
- ↑ Pinto A, Mancebo MC, Eisen JL, Pagano ME, Rasmussen SA (May 2006). "The Brown Longitudinal Obsessive Compulsive Study: clinical features and symptoms of the sample at intake". The Journal of Clinical Psychiatry. 67 (5): 703–11. doi:10.4088/JCP.v67n0503. PMC 3272757. PMID 16841619.
- ↑ Lucka I, Cebella A (2004). "[Characteristics of the forming personality in children suffering from anorexia nervosa]". Psychiatria Polska. 38 (6): 1011–8. PMID 15779665.
- ↑ Biederman J, Ball SW, Monuteaux MC, Surman CB, Johnson JL, Zeitlin S (August 2007). "Are girls with ADHD at risk for eating disorders? Results from a controlled, five-year prospective study". Journal of Developmental and Behavioral Pediatrics. 28 (4): 302–7. doi:10.1097/DBP.0b013e3180327917. PMID 17700082. S2CID 31596462.
- ↑ Dukarm CP (May 2005). "Bulimia nervosa and attention deficit hyperactivity disorder: a possible role for stimulant medication". Journal of Women's Health. 14 (4): 345–50. doi:10.1089/jwh.2005.14.345. PMID 15916509.
- ↑ Mikami AY, Hinshaw SP, Arnold LE, Hoza B, Hechtman L, Newcorn JH, Abikoff HB (April 2010). "Bulimia nervosa symptoms in the multimodal treatment study of children with ADHD". The International Journal of Eating Disorders. 43 (3): 248–59. doi:10.1002/eat.20692. PMID 19378318.
- ↑ Cortese S, Bernardina BD, Mouren MC (September 2007). "Attention-deficit/hyperactivity disorder (ADHD) and binge eating". Nutrition Reviews. 65 (9): 404–11. doi:10.1111/j.1753-4887.2007.tb00318.x. PMID 17958207. S2CID 14578808.
- ↑ Bruce KR, Steiger H, Koerner NM, Israel M, Young SN (January 2004). "Bulimia nervosa with co-morbid avoidant personality disorder: behavioural characteristics and serotonergic function". Psychological Medicine. 34 (1): 113–24. doi:10.1017/S003329170300864X. PMID 14971632.
- 1 2 Williamson DA, Muller SL, Reas DL, Thaw JM (October 1999). "Cognitive bias in eating disorders: implications for theory and treatment". Behavior Modification. 23 (4): 556–77. doi:10.1177/0145445599234003. PMID 10533440. Archived from the original on 2021-08-28. Retrieved 2020-08-02.
- ↑ Faunce GJ (2002-06-01). "Eating disorders and attentional bias: a review". Eating Disorders. 10 (2): 125–39. doi:10.1080/10640260290081696. PMID 16864253.
- ↑ Aspen V, Darcy AM, Lock J (August 2013). "A review of attention biases in women with eating disorders". Cognition & Emotion. 27 (5): 820–38. doi:10.1080/02699931.2012.749777. PMC 3610839. PMID 23228135.
- ↑ Podar I, Hannus A, Allik J (August 1999). "Personality and affectivity characteristics associated with eating disorders: a comparison of eating disordered, weight-preoccupied, and normal samples". Journal of Personality Assessment. 73 (1): 133–47. doi:10.1207/S15327752JPA730109. PMID 10497805.
- ↑ Skårderud, F and Fonagy, P "Eating Disorders" in Bateman, A and Fonagy, P (Eds) Handbook of mentalizing in Mental Health Practice. American Psychiatric Publishing, Washington DC, 2012. Pages 347-383
- ↑ Gardini S, Cloninger CR, Venneri A (June 2009). "Individual differences in personality traits reflect structural variance in specific brain regions". Brain Research Bulletin. 79 (5): 265–70. doi:10.1016/j.brainresbull.2009.03.005. PMID 19480986.
- ↑ Marsh AA, Finger EC, Mitchell DG, Reid ME, Sims C, Kosson DS, et al. (June 2008). "Reduced amygdala response to fearful expressions in children and adolescents with callous-unemotional traits and disruptive behavior disorders". The American Journal of Psychiatry. 165 (6): 712–20. doi:10.1176/appi.ajp.2007.07071145. PMID 18281412. S2CID 6915571.
- ↑ Iidaka T, Matsumoto A, Ozaki N, Suzuki T, Iwata N, Yamamoto Y, et al. (December 2006). "Volume of left amygdala subregion predicted temperamental trait of harm avoidance in female young subjects. A voxel-based morphometry study". Brain Research. 1125 (1): 85–93. doi:10.1016/j.brainres.2006.09.015. PMID 17113049.
- ↑ Rubino V, Blasi G, Latorre V, Fazio L, d'Errico I, Mazzola V, et al. (September 2007). "Activity in medial prefrontal cortex during cognitive evaluation of threatening stimuli as a function of personality style". Brain Research Bulletin. 74 (4): 250–7. doi:10.1016/j.brainresbull.2007.06.019. PMID 17720547.
- ↑ Spinella M, Lyke J (January 2004). "Executive personality traits and eating behavior". The International Journal of Neuroscience. 114 (1): 83–93. doi:10.1080/00207450490249356. PMID 14660070. S2CID 11710150.
- ↑ Sinai C, Hirvikoski T, Vansvik ED, Nordström AL, Linder J, Nordström P, Jokinen J (November 2009). "Thyroid hormones and personality traits in attempted suicide". Psychoneuroendocrinology. 34 (10): 1526–32. doi:10.1016/j.psyneuen.2009.05.009. PMID 19525070.
- 1 2 3 4 Bern EM, O'Brien RF (August 2013). "Is it an eating disorder, gastrointestinal disorder, or both?". Current Opinion in Pediatrics (Review). 25 (4): 463–70. doi:10.1097/MOP.0b013e328362d1ad. PMID 23838835.
Several case reports brought attention to the association of anorexia nervosa and celiac disease.(...) Some patients present with the eating disorder prior to diagnosis of celiac disease and others developed anorexia nervosa after the diagnosis of celiac disease. Healthcare professionals should screen for celiac disease with eating disorder symptoms especially with gastrointestinal symptoms, weight loss, or growth failure.(...) Celiac disease patients may present with gastrointestinal symptoms such as diarrhea, steatorrhea, weight loss, vomiting, abdominal pain, anorexia, constipation, bloating, and distension due to malabsorption. Extraintestinal presentations include anemia, osteoporosis, dermatitis herpetiformis, short stature, delayed puberty, fatigue, aphthous stomatitis, elevated transaminases, neurologic problems, or dental enamel hypoplasia.(...) it has become clear that symptomatic and diagnosed celiac disease is the tip of the iceberg; the remaining 90% or more of children are asymptomatic and undiagnosed.
- ↑ Quick VM, Byrd-Bredbenner C, Neumark-Sztainer D (May 2013). "Chronic illness and disordered eating: a discussion of the literature". Advances in Nutrition (Review). 4 (3): 277–86. doi:10.3945/an.112.003608. PMC 3650496. PMID 23674793.
- 1 2 Caslini M, Bartoli F, Crocamo C, Dakanalis A, Clerici M, Carrà G (January 2016). "Disentangling the Association Between Child Abuse and Eating Disorders: A Systematic Review and Meta-Analysis". Psychosomatic Medicine. 78 (1): 79–90. doi:10.1097/psy.0000000000000233. PMID 26461853.
- ↑ Troop NA, Bifulco A (June 2002). "Childhood social arena and cognitive sets in eating disorders". British Journal of Clinical Psychology. 41 (Pt 2): 205–11. doi:10.1348/014466502163976. PMID 12034006.
- ↑ Nonogaki K, Nozue K, Oka Y (October 2007). "Social isolation affects the development of obesity and type 2 diabetes in mice". Endocrinology. 148 (10): 4658–66. doi:10.1210/en.2007-0296. PMID 17640995.
- ↑ Esplen MJ, Garfinkel P, Gallop R (January 2000). "Relationship between self-soothing, aloneness, and evocative memory in bulimia nervosa". The International Journal of Eating Disorders. 27 (1): 96–100. doi:10.1002/(SICI)1098-108X(200001)27:1<96::AID-EAT11>3.0.CO;2-S. PMID 10590454.
- ↑ Larson R, Johnson C (1985). "Bulimia: disturbed patterns of solitude". Addictive Behaviors. 10 (3): 281–90. doi:10.1016/0306-4603(85)90009-7. PMID 3866486.
- ↑ Fox JR (July 2009). "Eating disorders and emotions". Clinical Psychology & Psychotherapy. 16 (4): 237–9. doi:10.1002/cpp.625. PMID 19639648.
- ↑ Johnson JG, Cohen P, Kasen S, Brook JS (March 2002). "Childhood adversities associated with risk for eating disorders or weight problems during adolescence or early adulthood". The American Journal of Psychiatry. 159 (3): 394–400. doi:10.1176/appi.ajp.159.3.394. PMID 11870002.
- ↑ Klesges RC, Coates TJ, Brown G, Sturgeon-Tillisch J, Moldenhauer-Klesges LM, Holzer B, et al. (1983). "Parental influences on children's eating behavior and relative weight". Journal of Applied Behavior Analysis. 16 (4): 371–8. doi:10.1901/jaba.1983.16-371. PMC 1307898. PMID 6654769.
- ↑ Galloway AT, Fiorito L, Lee Y, Birch LL (April 2005). "Parental pressure, dietary patterns, and weight status among girls who are "picky eaters"". Journal of the American Dietetic Association. 105 (4): 541–8. doi:10.1016/j.jada.2005.01.029. PMC 2530930. PMID 15800554.
- ↑ Jones C, Harris G, Leung N (December 2005). "Parental rearing behaviours and eating disorders: the moderating role of core beliefs". Eating Behaviors. 6 (4): 355–64. doi:10.1016/j.eatbeh.2005.05.002. PMID 16257809.
- ↑ Brown R, Ogden J (June 2004). "Children's eating attitudes and behaviour: a study of the modelling and control theories of parental influence". Health Education Research. 19 (3): 261–71. doi:10.1093/her/cyg040. PMID 15140846.
- ↑ Savage JS, Fisher JO, Birch LL (2007). "Parental influence on eating behavior: conception to adolescence". The Journal of Law, Medicine & Ethics. 35 (1): 22–34. doi:10.1111/j.1748-720X.2007.00111.x. PMC 2531152. PMID 17341215.
- ↑ Adams GR, Crane P (1980). "An Assessment of Parents' and Teachers' Expectations of Preschool Children's Social Preference for Attractive or Unattractive Children and Adults". Child Development. 51 (1): 224–231. doi:10.2307/1129610. JSTOR 1129610.
- ↑ Nolen-Hoeksema, Susan. Abnormal Psychology, 6e. McGraw-Hill Education, 2014. p. 359-360.
- ↑ Schreiber GB, Robins M, Striegel-Moore R, Obarzanek E, Morrison JA, Wright DJ (July 1996). "Weight modification efforts reported by black and white preadolescent girls: National Heart, Lung, and Blood Institute Growth and Health Study". Pediatrics. 98 (1): 63–70. PMID 8668414.
- ↑ Page RM, Suwanteerangkul J (September 2007). "Dieting among Thai adolescents: having friends who diet and pressure to diet". Eating and Weight Disorders. 12 (3): 114–24. doi:10.1007/bf03327638. PMID 17984635.
- ↑ The Mcknight Investigators (February 2003). "Risk factors for the onset of eating disorders in adolescent girls: results of the McKnight longitudinal risk factor study". The American Journal of Psychiatry. 160 (2): 248–54. doi:10.1176/ajp.160.2.248. PMID 12562570.
- ↑ Paxton SJ, Schutz HK, Wertheim EH, Muir SL (May 1999). "Friendship clique and peer influences on body image concerns, dietary restraint, extreme weight-loss behaviors, and binge eating in adolescent girls". Journal of Abnormal Psychology. 108 (2): 255–66. doi:10.1037/0021-843X.108.2.255. PMID 10369035.
- ↑ Rukavina T, Pokrajac-Bulian A (March 2006). "Thin-ideal internalization, body dissatisfaction and symptoms of eating disorders in Croatian adolescent girls". Eating and Weight Disorders. 11 (1): 31–7. doi:10.1007/bf03327741. PMID 16801743.
- ↑ [ Nolen-Hoeksema, Susan (2014). (Ab)normal psychology. New York, NY: McGraw Hill. p. 323. ISBN 978-0-07-803538-8.
- ↑ Knauss C, Paxton SJ, Alsaker FD (December 2007). "Relationships amongst body dissatisfaction, internalisation of the media body ideal and perceived pressure from media in adolescent girls and boys". Body Image. 4 (4): 353–60. doi:10.1016/j.bodyim.2007.06.007. PMID 18089281.
- ↑ Garner DM, Garfinkel PE (November 1980). "Socio-cultural factors in the development of anorexia nervosa". Psychological Medicine. 10 (4): 647–56. doi:10.1017/S0033291700054945. PMID 7208724. S2CID 15755468.
- ↑ Eisenberg ME, Neumark-Sztainer D, Story M, Perry C (March 2005). "The role of social norms and friends' influences on unhealthy weight-control behaviors among adolescent girls". Social Science & Medicine. 60 (6): 1165–73. doi:10.1016/j.socscimed.2004.06.055. PMID 15626514.
- ↑ Jung J, Lennon SJ (2003). "Body Image, Appearance Self-Schema, and Media Images". Family and Consumer Sciences Research Journal. 32: 27–51. doi:10.1177/1077727X03255900.
- ↑ Nevonen L, Norring C (December 2004). "Socio-economic variables and eating disorders: a comparison between patients and normal controls". Eating and Weight Disorders. 9 (4): 279–84. doi:10.1007/BF03325082. PMID 15844400.
- ↑ Polivy J, Herman CP (2002). "Causes of eating disorders". Annual Review of Psychology. 53: 187–213. doi:10.1146/annurev.psych.53.100901.135103. PMID 11752484. S2CID 2913370.
- ↑ Soh NL, Touyz SW, Surgenor LJ (2006). "Eating and body image disturbances across cultures: A review". European Eating Disorders Review. 14 (1): 54–65. doi:10.1002/erv.678. S2CID 178892.
- ↑ Essick, Ellen (2006). "Eating Disorders and Sexuality". In Steinberg, Shirley R.; Parmar, Priya; Richard, Birgit (eds.). Contemporary Youth Culture: An International Encyclopedia. Greenwood. pp. 276–80. ISBN 978-0-313-33729-1.
{{cite book}}: Unknown parameter|chapterurl=ignored (help) - ↑ DeMonte, Alexandria. "Beauty Pageants". M.E. Sharpe. Retrieved 24 September 2013.
- ↑ Nolen-Hoeksema, Susan (2014). abnormal psychology (6th ed.). New York: McGraw-Hill Education. pp. 353–354. ISBN 978-0-07-803538-8.
- 1 2 Boisvert JA, Harrell WA (2009). "Homosexuality as a Risk Factor for Eating Disorder Symptomatology in Men". The Journal of Men's Studies. 17 (3): 210–25. doi:10.3149/jms.1703.210.
- 1 2 3 Siconolfi D, Halkitis PN, Allomong TW, Burton CL (2009). "Body Dissatisfaction and Eating Disorders in a Sample of Gay and Bisexual Men". International Journal of Men's Health. 8 (3): 254–64. doi:10.3149/jmh.0803.254.
- ↑ Schwitzer, AM (2012). "Diagnosing, Conceptualizing, and Treating Eating Disorders Not Otherwise Specified: A Comprehensive Practice Model". Journal of Counseling & Development. 90 (3): 281–9. doi:10.1002/j.1556-6676.2012.00036.x.
- ↑ Kim Willsher, Models in France must provide doctor's note to work Archived 2016-12-26 at the Wayback Machine, The Guardian, 18 December.
- 1 2 Ghaznavi J, Taylor LD (June 2015). "Bones, body parts, and sex appeal: An analysis of #thinspiration images on popular social media". Body Image. 14: 54–61. doi:10.1016/j.bodyim.2015.03.006. PMID 25880783.
- 1 2 Perloff, Richard M. (2014-05-29). "Social Media Effects on Young Women's Body Image Concerns: Theoretical Perspectives and an Agenda for Research". Sex Roles. 71 (11–12): 363–377. doi:10.1007/s11199-014-0384-6. ISSN 0360-0025.
- ↑ Arseniev-Koehler A, Lee H, McCormick T, Moreno MA (June 2016). "#Proana: Pro-Eating Disorder Socialization on Twitter". The Journal of Adolescent Health. 58 (6): 659–64. doi:10.1016/j.jadohealth.2016.02.012. PMID 27080731.
- ↑ Yu UJ (2014). "Deconstructing College Students' Perceptions of Thin-Idealized Versus Nonidealized Media Images on Body Dissatisfaction and Advertising Effectiveness". Clothing and Textiles Research Journal. 32 (3): 153–169. doi:10.1177/0887302x14525850.
- ↑ Keel PK, Klump KL (September 2003). "Are eating disorders culture-bound syndromes? Implications for conceptualizing their etiology". Psychological Bulletin. 129 (5): 747–69. doi:10.1037/0033-2909.129.5.747. PMID 12956542. S2CID 7683812.
- 1 2 Coetzee V, Faerber SJ, Greeff JM, Lefevre CE, Re DE, Perrett DI (2012-10-29). "African perceptions of female attractiveness". PLOS ONE. 7 (10): e48116. Bibcode:2012PLoSO...748116C. doi:10.1371/journal.pone.0048116. PMC 3483252. PMID 23144734.
- ↑ Freeman, Amanda C.; Szabo, Christopher P. (2005). "Eating Disorders in South African Males: A Review of the Clinical Presentation of Hospitalised Patients". South African Journal of Psychology. 35 (4): 601–622. doi:10.1177/008124630503500401. ISSN 0081-2463.
- 1 2 Davis C, Yager J (September 1992). "Transcultural aspects of eating disorders: a critical literature review". Culture, Medicine and Psychiatry. 16 (3): 377–94. doi:10.1007/BF00052156. PMID 1395702. Archived from the original on 2021-08-28. Retrieved 2020-08-02.
- ↑ Taylor JY, Caldwell CH, Baser RE, Faison N, Jackson JS (November 2007). "Prevalence of eating disorders among Blacks in the National Survey of American Life". The International Journal of Eating Disorders. 40 Suppl (Suppl): S10-4. doi:10.1002/eat.20451. PMC 2882704. PMID 17879287.
- 1 2 3 4 5 6 7 8 9 10 11 Pike KM, Dunne PE (2015-09-17). "The rise of eating disorders in Asia: a review". Journal of Eating Disorders. 3 (1): 33. doi:10.1186/s40337-015-0070-2. PMC 4574181. PMID 26388993.
- ↑ Chen H, Jackson T (September 2008). "Prevalence and sociodemographic correlates of eating disorder endorsements among adolescents and young adults from China". European Eating Disorders Review. 16 (5): 375–85. doi:10.1002/erv.837. PMID 17960779.
- 1 2 3 Miller MN, Pumariega AJ (May 2001). "Culture and eating disorders: a historical and cross-cultural review". Psychiatry. 64 (2): 93–110. doi:10.1521/psyc.64.2.93.18621. PMID 11495364.
- ↑ Mammen P, Russell S, Russell PS (May 2007). "Prevalence of eating disorders and psychiatric comorbidity among children and adolescents". Indian Pediatrics. 44 (5): 357–9. PMID 17536137.
- ↑ Gross MJ, Kahn JP, Laxenaire M, Nicolas JP, Burlet C (1994). "[Corticotropin-releasing factor and anorexia nervosa: reactions of the hypothalamus-pituitary-adrenal axis to neurotropic stress]". Annales d'Endocrinologie. 55 (6): 221–8. PMID 7864577.
- ↑ Licinio J, Wong ML, Gold PW (April 1996). "The hypothalamic-pituitary-adrenal axis in anorexia nervosa". Psychiatry Research. 62 (1): 75–83. doi:10.1016/0165-1781(96)02991-5. PMID 8739117. Archived from the original on 2020-07-31. Retrieved 2020-08-02.
- ↑ Chaudhri O, Small C, Bloom S (July 2006). "Gastrointestinal hormones regulating appetite". Philosophical Transactions of the Royal Society of London. Series B, Biological Sciences. 361 (1471): 1187–209. doi:10.1098/rstb.2006.1856. PMC 1642697. PMID 16815798.
- ↑ Gendall KA, Kaye WH, Altemus M, McConaha CW, La Via MC (July 1999). "Leptin, neuropeptide Y, and peptide YY in long-term recovered eating disorder patients". Biological Psychiatry. 46 (2): 292–9. doi:10.1016/S0006-3223(98)00292-3. PMID 10418705.
- ↑ Wilhelm J, Müller E, de Zwaan M, Fischer J, Hillemacher T, Kornhuber J, et al. (April 2010). "Elevation of homocysteine levels is only partially reversed after therapy in females with eating disorders". Journal of Neural Transmission. 117 (4): 521–7. doi:10.1007/s00702-010-0379-6. PMID 20191295.
- ↑ Jimerson DC, Lesem MD, Kaye WH, Hegg AP, Brewerton TD (September 1990). "Eating disorders and depression: is there a serotonin connection?". Biological Psychiatry. 28 (5): 443–54. doi:10.1016/0006-3223(90)90412-U. PMID 2207221.
- ↑ Leibowitz SF (1990). "The role of serotonin in eating disorders". Drugs. 39 Suppl 3: 33–48. doi:10.2165/00003495-199000393-00005. PMID 2197074.
- ↑ Blundell JE, Lawton CL, Halford JC (November 1995). "Serotonin, eating behavior, and fat intake". Obesity Research. 3 Suppl 4: 471S–476S. doi:10.1002/j.1550-8528.1995.tb00214.x. PMID 8697045.
- ↑ Kaye WH (1997). "Anorexia nervosa, obsessional behavior, and serotonin". Psychopharmacology Bulletin. 33 (3): 335–44. PMID 9550876.
- ↑ Bailer UF, Price JC, Meltzer CC, Mathis CA, Frank GK, Weissfeld L, et al. (June 2004). "Altered 5-HT(2A) receptor binding after recovery from bulimia-type anorexia nervosa: relationships to harm avoidance and drive for thinness". Neuropsychopharmacology. 29 (6): 1143–55. doi:10.1038/sj.npp.1300430. PMC 4301578. PMID 15054474.
- ↑ Hainer V, Kabrnova K, Aldhoon B, Kunesova M, Wagenknecht M (November 2006). "Serotonin and norepinephrine reuptake inhibition and eating behavior". Annals of the New York Academy of Sciences. 1083 (1): 252–69. Bibcode:2006NYASA1083..252H. doi:10.1196/annals.1367.017. PMID 17148744.
- ↑ George DT, Kaye WH, Goldstein DS, Brewerton TD, Jimerson DC (July 1990). "Altered norepinephrine regulation in bulimia: effects of pharmacological challenge with isoproterenol". Psychiatry Research. 33 (1): 1–10. doi:10.1016/0165-1781(90)90143-S. PMID 2171006.
- ↑ Wang GJ, Volkow ND, Logan J, Pappas NR, Wong CT, Zhu W, et al. (February 2001). "Brain dopamine and obesity". Lancet. 357 (9253): 354–7. doi:10.1016/S0140-6736(00)03643-6. PMID 11210998.
- ↑ Zhulenko VN, Georgieva GN, Smirnova LA (April 1975). "[Mercury content in the organs and tissues of slaughter animals]". Veterinariia (4): 96–8. PMID 1216579.
- 1 2 3 4 5 Carlson, Neil (2013). "Ingestive Behavior". Physiology of Behavior. University of Massachusetts, Amherst: Pearson. pp. 428–432. ISBN 978-0-205-23939-9.
- ↑ Frederich R, Hu S, Raymond N, Pomeroy C (February 2002). "Leptin in anorexia nervosa and bulimia nervosa: importance of assay technique and method of interpretation". The Journal of Laboratory and Clinical Medicine. 139 (2): 72–9. doi:10.1067/mlc.2002.121014. PMID 11919545.
- ↑ Ferron F, Considine RV, Peino R, Lado IG, Dieguez C, Casanueva FF (March 1997). "Serum leptin concentrations in patients with anorexia nervosa, bulimia nervosa and non-specific eating disorders correlate with the body mass index but are independent of the respective disease". Clinical Endocrinology. 46 (3): 289–93. doi:10.1046/j.1365-2265.1997.1260938.x. PMID 9156037.
- ↑ Fetissov SO, Harro J, Jaanisk M, Järv A, Podar I, Allik J, et al. (October 2005). "Autoantibodies against neuropeptides are associated with psychological traits in eating disorders". Proceedings of the National Academy of Sciences of the United States of America. 102 (41): 14865–70. Bibcode:2005PNAS..10214865F. doi:10.1073/pnas.0507204102. PMC 1253594. PMID 16195379.
- ↑ Sinno MH, Do Rego JC, Coëffier M, Bole-Feysot C, Ducrotté P, Gilbert D, et al. (January 2009). "Regulation of feeding and anxiety by alpha-MSH reactive autoantibodies". Psychoneuroendocrinology. 34 (1): 140–9. doi:10.1016/j.psyneuen.2008.08.021. PMID 18842346.
- ↑ Tennoune N, Chan P, Breton J, Legrand R, Chabane YN, Akkermann K, et al. (October 2014). "Bacterial ClpB heat-shock protein, an antigen-mimetic of the anorexigenic peptide α-MSH, at the origin of eating disorders". Translational Psychiatry. 4 (10): e458. doi:10.1038/tp.2014.98. PMC 4350527. PMID 25290265.
- ↑ Sokol MS (2000). "Infection-triggered anorexia nervosa in children: clinical description of four cases". Journal of Child and Adolescent Psychopharmacology. 10 (2): 133–45. doi:10.1089/cap.2000.10.133. PMID 10933123.
- ↑ Uher R, Treasure J (June 2005). "Brain lesions and eating disorders". Journal of Neurology, Neurosurgery, and Psychiatry. 76 (6): 852–7. doi:10.1136/jnnp.2004.048819. PMC 1739667. PMID 15897510.
- ↑ Houy E, Debono B, Dechelotte P, Thibaut F (December 2007). "Anorexia nervosa associated with right frontal brain lesion". The International Journal of Eating Disorders. 40 (8): 758–61. doi:10.1002/eat.20439. PMID 17683096.
- 1 2 Trummer M, Eustacchio S, Unger F, Tillich M, Flaschka G (August 2002). "Right hemispheric frontal lesions as a cause for anorexia nervosa report of three cases". Acta Neurochirurgica. 144 (8): 797–801, discussion 801. doi:10.1007/s00701-002-0934-5. PMID 12181689.
- ↑ Winston AP, Barnard D, D'Souza G, Shad A, Sherlala K, Sidhu J, Singh SP (November 2006). "Pineal germinoma presenting as anorexia nervosa: Case report and review of the literature". The International Journal of Eating Disorders. 39 (7): 606–8. doi:10.1002/eat.20322. PMID 17041920.
- ↑ Chipkevitch E, Fernandes AC (June 1993). "Hypothalamic tumor associated with atypical forms of anorexia nervosa and diencephalic syndrome". Arquivos de Neuro-Psiquiatria. 51 (2): 270–4. doi:10.1590/S0004-282X1993000200022. PMID 8274094.
- ↑ Rohrer TR, Fahlbusch R, Buchfelder M, Dörr HG (2006). "Craniopharyngioma in a female adolescent presenting with symptoms of anorexia nervosa". Klinische Padiatrie. 218 (2): 67–71. doi:10.1055/s-2006-921506. PMID 16506105.
- ↑ Chipkevitch E (1994). "Brain tumors and anorexia nervosa syndrome". Brain & Development. 16 (3): 175–9, discussion 180–2. doi:10.1016/0387-7604(94)90064-7. PMID 7943600.
- ↑ Lin L, Liao SC, Lee YJ, Tseng MC, Lee MB (October 2003). "Brain tumor presenting as anorexia nervosa in a 19-year-old man". Journal of the Formosan Medical Association = Taiwan Yi Zhi. 102 (10): 737–40. PMID 14691602.
- ↑ Conrad R, Wegener I, Geiser F, Imbierowicz K, Liedtke R (October 2008). "Nature against nurture: calcification in the right thalamus in a young man with anorexia nervosa and obsessive-compulsive personality disorder". CNS Spectrums. 13 (10): 906–10. doi:10.1017/S1092852900017016. PMID 18955946.
- ↑ Burke CJ, Tannenberg AE, Payton DJ (November 1997). "Ischaemic cerebral injury, intrauterine growth retardation, and placental infarction". Developmental Medicine and Child Neurology. 39 (11): 726–30. doi:10.1111/j.1469-8749.1997.tb07373.x. PMID 9393885.
- ↑ Cnattingius S, Hultman CM, Dahl M, Sparén P (July 1999). "Very preterm birth, birth trauma, and the risk of anorexia nervosa among girls". Archives of General Psychiatry. 56 (7): 634–8. doi:10.1001/archpsyc.56.7.634. PMID 10401509.
- ↑ Favaro A, Tenconi E, Santonastaso P (January 2006). "Perinatal factors and the risk of developing anorexia nervosa and bulimia nervosa". Archives of General Psychiatry. 63 (1): 82–8. doi:10.1001/archpsyc.63.1.82. PMID 16389201. S2CID 45181444.
- ↑ Favaro A, Tenconi E, Santonastaso P (April 2008). "The relationship between obstetric complications and temperament in eating disorders: a mediation hypothesis". Psychosomatic Medicine. 70 (3): 372–7. doi:10.1097/PSY.0b013e318164604e. PMID 18256341.
- ↑ Decker MJ, Hue GE, Caudle WM, Miller GW, Keating GL, Rye DB (2003). "Episodic neonatal hypoxia evokes executive dysfunction and regionally specific alterations in markers of dopamine signaling". Neuroscience. 117 (2): 417–25. doi:10.1016/S0306-4522(02)00805-9. PMID 12614682.
- ↑ Decker MJ, Rye DB (December 2002). "Neonatal intermittent hypoxia impairs dopamine signaling and executive functioning". Sleep & Breathing = Schlaf & Atmung. 6 (4): 205–10. doi:10.1007/s11325-002-0205-y. PMID 12524574.
- ↑ Scher MS (February 2003). "Fetal and neonatal neurologic case histories: assessment of brain disorders in the context of fetal-maternal-placental disease. Part 1: Fetal neurologic consultations in the context of antepartum events and prenatal brain development". Journal of Child Neurology. 18 (2): 85–92. doi:10.1177/08830738030180020901. PMID 12693773.
- ↑ Scher MS, Wiznitzer M, Bangert BA (December 2002). "Cerebral infarctions in the fetus and neonate: maternal-placental-fetal considerations". Clinics in Perinatology. 29 (4): 693–724, vi–vii. doi:10.1016/S0095-5108(02)00055-6. PMID 12516742.
- ↑ Burke CJ, Tannenberg AE (June 1995). "Prenatal brain damage and placental infarction--an autopsy study". Developmental Medicine and Child Neurology. 37 (6): 555–62. doi:10.1111/j.1469-8749.1995.tb12042.x. PMID 7789664.
- ↑ Squier M, Keeling JW (February 1991). "The incidence of prenatal brain injury". Neuropathology and Applied Neurobiology. 17 (1): 29–38. doi:10.1111/j.1365-2990.1991.tb00691.x. PMID 2057048.
- ↑ Al Mamun A, Lawlor DA, Alati R, O'Callaghan MJ, Williams GM, Najman JM (August 2006). "Does maternal smoking during pregnancy have a direct effect on future offspring obesity? Evidence from a prospective birth cohort study". American Journal of Epidemiology. 164 (4): 317–25. doi:10.1093/aje/kwj209. PMID 16775040.
- ↑ Keys A, Brozek J, Henschel A, Mickelsen O, Taylor H (1950). The Biology of Human Starvation. University of Minnesota Press.
- ↑ Pritts SD, Susman J (January 2003). "Diagnosis of eating disorders in primary care". American Family Physician. 67 (2): 297–304. PMID 12562151.
- ↑ Gelder, Mayou, Geddes (2005). Psychiatry: Page 161. New York, NY; Oxford University Press Inc.
- ↑ O'Brien A, Hugo P, Stapleton S, Lask B (November 2001). ""Anorexia saved my life": coincidental anorexia nervosa and cerebral meningioma". The International Journal of Eating Disorders. 30 (3): 346–9. doi:10.1002/eat.1095. PMID 11746295.
- ↑ Garfinkel PE, Newman A (March 2001). "The eating attitudes test: twenty-five years later". Eating and Weight Disorders. 6 (1): 1–24. doi:10.1007/bf03339747. PMID 11300541.
- ↑ Rueda GE, Díaz LA, Campo A, Barros JA, Avila GC, Oróstegui LT, et al. (June 2005). "[Validation of the SCOFF questionnaire for screening of eating disorders in university women]". Biomedica. 25 (2): 196–202. doi:10.7705/biomedica.v25i2.1342. PMID 16022374. Archived from the original on 2020-10-28. Retrieved 2020-08-02.
- ↑ Probst M, Pieters G, Vanderlinden J (November 2008). "Evaluation of body experience questionnaires in eating disorders in female patients (AN/BN) and nonclinical participants". The International Journal of Eating Disorders. 41 (7): 657–65. doi:10.1002/eat.20531. PMID 18446834.
- ↑ Ben-Tovim DI, Walker MK (November 1992). "A quantitative study of body-related attitudes in patients with anorexia and bulimia nervosa". Psychological Medicine. 22 (4): 961–9. doi:10.1017/S0033291700038538. PMID 1488491.
- ↑ Olson MS, Williford HN, Richards LA, Brown JA, Pugh S (June 1996). "Self-reports on the Eating Disorder Inventory by female aerobic instructors". Perceptual and Motor Skills. 82 (3 Pt 1): 1051–8. doi:10.2466/pms.1996.82.3.1051. PMID 8774050.
- ↑ Wilfley DE, Schwartz MB, Spurrell EB, Fairburn CG (April 2000). "Using the eating disorder examination to identify the specific psychopathology of binge eating disorder". The International Journal of Eating Disorders. 27 (3): 259–69. doi:10.1002/(SICI)1098-108X(200004)27:3<259::AID-EAT2>3.0.CO;2-G. PMID 10694711. S2CID 34245277.
- ↑ Ehle G, Wahlstab A, Ott J (November 1982). "[Psychodiagnostic findings in anorexia nervosa and post-pill amenorrhea]". Psychiatrie, Neurologie, und Medizinische Psychologie. 34 (11): 647–56. PMID 7170321.
- ↑ Kennedy SH, Kaplan AS, Garfinkel PE, Rockert W, Toner B, Abbey SE (October 1994). "Depression in anorexia nervosa and bulimia nervosa: discriminating depressive symptoms and episodes". Journal of Psychosomatic Research. 38 (7): 773–82. doi:10.1016/0022-3999(94)90030-2. PMID 7877132.
- ↑ Camargo EE (April 2001). "Brain SPECT in neurology and psychiatry". Journal of Nuclear Medicine. 42 (4): 611–23. PMID 11337551.
- ↑ Abebe DS, Lien L, von Soest T (September 2012). "The development of bulimic symptoms from adolescence to young adulthood in females and males: a population-based longitudinal cohort study". The International Journal of Eating Disorders. 45 (6): 737–45. doi:10.1002/eat.20950. PMID 22886952.
- ↑ Fallon BA, Nields JA (November 1994). "Lyme disease: a neuropsychiatric illness". The American Journal of Psychiatry. 151 (11): 1571–83. doi:10.1176/ajp.151.11.1571. PMID 7943444. S2CID 22568915.
- ↑ Pachner AR (1988). "Borrelia burgdorferi in the nervous system: the new "great imitator"". Annals of the New York Academy of Sciences. 539 (1): 56–64. Bibcode:1988NYASA.539...56P. doi:10.1111/j.1749-6632.1988.tb31838.x. PMID 3190104.
- ↑ Volta U, Caio G, De Giorgio R, Henriksen C, Skodje G, Lundin KE (June 2015). "Non-celiac gluten sensitivity: a work-in-progress entity in the spectrum of wheat-related disorders". Best Practice & Research. Clinical Gastroenterology (Review). 29 (3): 477–91. doi:10.1016/j.bpg.2015.04.006. PMID 26060112.
Among psychiatric disorders, a minority (6%) of patients with NCGS showed a previous clinical history of eating behavior abnormalities (NCGS = non-celiac gluten sensitivity)
- ↑ Duggan JM (May 2004). "Coeliac disease: the great imitator" (PDF). The Medical Journal of Australia (Review). 180 (10): 524–6. doi:10.5694/j.1326-5377.2004.tb06058.x. PMID 15139831. Archived (PDF) from the original on March 5, 2016.
- ↑ Zingone F, Swift GL, Card TR, Sanders DS, Ludvigsson JF, Bai JC (April 2015). "Psychological morbidity of celiac disease: A review of the literature". United European Gastroenterology Journal (Review). 3 (2): 136–45. doi:10.1177/2050640614560786. PMC 4406898. PMID 25922673.
- ↑ Jackson JR, Eaton WW, Cascella NG, Fasano A, Kelly DL (March 2012). "Neurologic and psychiatric manifestations of celiac disease and gluten sensitivity". The Psychiatric Quarterly. 83 (1): 91–102. doi:10.1007/s11126-011-9186-y. PMC 3641836. PMID 21877216.
- ↑ Adams R, Hinkebein MK, McQuillen M, Sutherland S, El Asyouty S, Lippmann S (February 1998). "Prompt differentiation of Addison's disease from anorexia nervosa during weight loss and vomiting". Southern Medical Journal. 91 (2): 208–11. doi:10.1097/00007611-199802000-00017. PMID 9496878.
- ↑ Siew LC, Huang C, Fleming J (April 2010). "Gastric adenocarcinoma mistakenly diagnosed as an eating disorder: case report". The International Journal of Eating Disorders. 43 (3): 286–8. doi:10.1002/eat.20678. PMID 19365820.
- ↑ Mannucci E, Ricca V, Filetti S, Boldrini M, Rotella CM (August 2003). "Eating behavior and thyroid disease in female obese patients". Eating Behaviors. 4 (2): 173–9. doi:10.1016/S1471-0153(03)00012-6. PMID 15000980.
- ↑ Byerley B, Black DW, Grosser BI (August 1983). "Anorexia nervosa with hyperthyroidism: case report". The Journal of Clinical Psychiatry. 44 (8): 308–9. PMID 6874653.
- ↑ Krahn D (1990). "Thyrotoxicosis and bulimia nervosa". Psychosomatics. 31 (2): 222–4. doi:10.1016/S0033-3182(90)72201-3. PMID 2330406.
- ↑ Tiller J, Macrae A, Schmidt U, Bloom S, Treasure J (August 1994). "The prevalence of eating disorders in thyroid disease: a pilot study". Journal of Psychosomatic Research. 38 (6): 609–16. doi:10.1016/0022-3999(94)90058-2. PMID 7990069.
- ↑ Fonseca V, Wakeling A, Havard CW (August 1990). "Hyperthyroidism and eating disorders". BMJ. 301 (6747): 322–3. doi:10.1136/bmj.301.6747.322. PMC 1663651. PMID 2393739.
- ↑ Birmingham CL, Gritzner S, Gutierrez E (November 2006). "Hyperthyroidism in anorexia nervosa: case report and review of the literature". The International Journal of Eating Disorders. 39 (7): 619–20. doi:10.1002/eat.20308. PMID 16958126.
- ↑ Mattingly D, Bhanji S (April 1995). "Hypoglycaemia and anorexia nervosa". Journal of the Royal Society of Medicine. 88 (4): 191–5. PMC 1295161. PMID 7745563.
- ↑ Ozawa Y, Koyano H, Akama T (July 1999). "Complete recovery from intractable bulimia nervosa by the surgical cure of primary hyperparathyroidism". The International Journal of Eating Disorders. 26 (1): 107–10. doi:10.1002/(SICI)1098-108X(199907)26:1<107::AID-EAT15>3.0.CO;2-U. PMID 10349592.
- ↑ Kar N, Misra B (February 2004). "Toxoplasma seropositivity and depression: a case report". BMC Psychiatry. 4: 1. doi:10.1186/1471-244X-4-1. PMC 356918. PMID 15018628.
- ↑ Ritchie MA, Perdigao JA. Neurosyphilis: Considerations for a Psychiatrist. Louisiana State University School of Medicine Department of Psychiatry Neurosyphilis Archived 2010-01-05 at the Wayback Machine
- ↑ Lipsitz JD, Fyer AJ, Paterniti A, Klein DF (2001). "Emetophobia: preliminary results of an internet survey". Depression and Anxiety. 14 (2): 149–52. doi:10.1002/da.1058. PMID 11668669. S2CID 11784677.
- ↑ Boschen MJ (2007). "Reconceptualizing emetophobia: a cognitive-behavioral formulation and research agenda". Journal of Anxiety Disorders. 21 (3): 407–19. doi:10.1016/j.janxdis.2006.06.007. PMID 16890398.
- ↑ Shapiro J, Franko DL, Gagne A (April 1997). "Phagophobia: a form of psychogenic dysphagia. A new entity". The Annals of Otology, Rhinology, and Laryngology. 106 (4): 286–90. doi:10.1177/000348949710600404. PMID 9109717.
- ↑ Gabbay V, Asnis GM, Bello JA, Alonso CM, Serras SJ, O'Dowd MA (July 2003). "New onset of body dysmorphic disorder following frontotemporal lesion". Neurology. 61 (1): 123–5. doi:10.1212/01.WNL.0000069607.30528.D5. PMID 12847173.
- ↑ Phillips KA, McElroy SL, Keck PE, Hudson JI, Pope HG (1994). "A comparison of delusional and nondelusional body dysmorphic disorder in 100 cases". Psychopharmacology Bulletin. 30 (2): 179–86. PMID 7831453.
- ↑ Feusner JD, Townsend J, Bystritsky A, Bookheimer S (December 2007). "Visual information processing of faces in body dysmorphic disorder". Archives of General Psychiatry. 64 (12): 1417–25. doi:10.1001/archpsyc.64.12.1417. PMID 18056550.
- ↑ Feusner JD, Yaryura-Tobias J, Saxena S (March 2008). "The pathophysiology of body dysmorphic disorder". Body Image. 5 (1): 3–12. doi:10.1016/j.bodyim.2007.11.002. PMC 3836287. PMID 18314401.
- ↑ Wallace, Kelly. "Kids as young as 5 concerned about body image". CNN. Archived from the original on 2019-11-05. Retrieved 2019-11-05.
- 1 2 Frayn M, Livshits S, Knäuper B (2018-09-14). "Emotional eating and weight regulation: a qualitative study of compensatory behaviors and concerns". Journal of Eating Disorders. 6: 23. doi:10.1186/s40337-018-0210-6. PMC 6137864. PMID 30221002.
- ↑ Vogel L (June 2019). "Fat shaming is making people sicker and heavier". CMAJ. 191 (23): E649. doi:10.1503/cmaj.109-5758. PMC 6565398. PMID 31182466.
- ↑ "Staying Active at Any Size | NIDDK". National Institute of Diabetes and Digestive and Kidney Diseases. Archived from the original on 2019-11-09. Retrieved 2019-11-05.
- ↑ Manwaring JL, Bryson SW, Goldschmidt AB, Winzelberg AJ, Luce KH, Cunning D, et al. (April 2008). "Do adherence variables predict outcome in an online program for the prevention of eating disorders?". Journal of Consulting and Clinical Psychology. 76 (2): 341–6. doi:10.1037/0022-006X.76.2.341. PMID 18377129. S2CID 30681111.
- ↑ National Research Council & Institute of Medicine. (2009b). Preventing mental, emotional, and behavioral disorders among young people: Progress and possibilities (M. E. O'Connell, T. Boat, & K. E. Warner, Eds.).Washington, DC: National Academies Press. p. 216.
- ↑ Halmi KA (June 2005). "The multimodal treatment of eating disorders". World Psychiatry. 4 (2): 69–73. PMC 1414734. PMID 16633511.
- ↑ Gelder, Mayou, Geddes (2005). Psychiatry. New York, NY: Oxford University Press Inc.
- ↑ (Downey, 2014) Archived 2015-07-01 at the Wayback Machine
- ↑ American Psychiatric Association practice guidelines for the treatment of psychiatric disorders (PDF) (3 ed.). Arlington, Virg.: American Psychiatric Association. 2006. ISBN 978-0890423851. Archived (PDF) from the original on 2020-08-04. Retrieved 2020-08-02.
- ↑ Pike KM, Walsh BT, Vitousek K, Wilson GT, Bauer J (November 2003). "Cognitive behavior therapy in the posthospitalization treatment of anorexia nervosa". The American Journal of Psychiatry. 160 (11): 2046–9. doi:10.1176/appi.ajp.160.11.2046. PMID 14594754. S2CID 27979486.
- ↑ Yeh HW, Tzeng NS, Lai TJ, Chou KR (August 2006). "[Cognitive behavioral therapy for eating disorders]". Hu Li Za Zhi. 53 (4): 65–73. PMID 16874604.
- 1 2 Schmidt U, Lee S, Beecham J, Perkins S, Treasure J, Yi I, et al. (April 2007). "A randomized controlled trial of family therapy and cognitive behavior therapy guided self-care for adolescents with bulimia nervosa and related disorders". The American Journal of Psychiatry. 164 (4): 591–8. doi:10.1176/appi.ajp.164.4.591. PMID 17403972.
- ↑ Berman MI, Boutelle KN, Crow SJ (November 2009). "A case series investigating acceptance and commitment therapy as a treatment for previously treated, unremitted patients with anorexia nervosa". European Eating Disorders Review. 17 (6): 426–34. doi:10.1002/erv.962. PMID 19760625.
- ↑ Wykes T, Brammer M, Mellers J, Bray P, Reeder C, Williams C, Corner J (August 2002). "Effects on the brain of a psychological treatment: cognitive remediation therapy: functional magnetic resonance imaging in schizophrenia". The British Journal of Psychiatry. 181: 144–52. doi:10.1192/bjp.181.2.144. PMID 12151286.
{{cite journal}}: Unknown parameter|displayauthors=ignored (help) - ↑ Cognitive Remediation Therapy for Anorexia Nervosa by Kate Tchanturia Publisher: Cambridge University Press; 1 edition (April 30, 2010) Language: English ISBN 0-521-74816-X ISBN 978-0-521-74816-2
- ↑ Tchanturia K, Davies H, Campbell IC (June 2007). "Cognitive remediation therapy for patients with anorexia nervosa: preliminary findings". Annals of General Psychiatry. 6 (1): 14. doi:10.1186/1744-859X-6-14. PMC 1892017. PMID 17550611.
- ↑ Cwojdzińska A, Markowska-Regulska K, Rybakowski F (2009). "[Cognitive remediation therapy in adolescent anorexia nervosa--case report]". Psychiatria Polska. 43 (1): 115–24. PMID 19694406.
- ↑ Schmidt, Ulrike; Wade, Tracey D.; Treasure, Janet (2014). "The Maudsley Model of Anorexia Nervosa Treatment for Adults (MANTRA): Development, Key Features, and Preliminary Evidence". Journal of Cognitive Psychotherapy. 28 (1): 48–71. doi:10.1891/0889-8391.28.1.48.
- ↑ Schmidt, Ulrike; Treasure, Janet (September 2006). "Anorexia nervosa: Valued and visible. A cognitive-interpersonal maintenance model and its implications for research and practice". British Journal of Clinical Psychology. 45 (3): 343–366. doi:10.1348/014466505X53902. PMID 17147101.
- ↑ Safer DL, Telch CF, Agras WS (April 2001). "Dialectical behavior therapy for bulimia nervosa". The American Journal of Psychiatry. 158 (4): 632–4. doi:10.1176/appi.ajp.158.4.632. PMID 11282700. S2CID 16651053.
- ↑ Eisler I, Dare C, Hodes M, Russell G, Dodge E, Le Grange D (September 2000). "Family therapy for adolescent anorexia nervosa: the results of a controlled comparison of two family interventions". Journal of Child Psychology and Psychiatry, and Allied Disciplines. 41 (6): 727–36. doi:10.1111/1469-7610.00660. PMID 11039685.
- ↑ Rhodes P, Brown J, Madden S (April 2009). "The Maudsley model of family-based treatment for anorexia nervosa: a qualitative evaluation of parent-to-parent consultation". Journal of Marital and Family Therapy. 35 (2): 181–92. doi:10.1111/j.1752-0606.2009.00115.x. PMID 19302516.
- ↑ Wallis A, Rhodes P, Kohn M, Madden S (2007). "Five-years of family based treatment for anorexia nervosa: the Maudsley Model at the Children's Hospital at Westmead". International Journal of Adolescent Medicine and Health. 19 (3): 277–83. doi:10.1515/IJAMH.2007.19.3.277. PMID 17937144.
- ↑ Gray JJ, Hoage CM (April 1990). "Bulimia nervosa: group behavior therapy with exposure plus response prevention". Psychological Reports. 66 (2): 667–74. doi:10.2466/PR0.66.2.667-674. PMID 1971954.
- ↑ McIntosh VV, Bulik CM, McKenzie JM, Luty SE, Jordan J (March 2000). "Interpersonal psychotherapy for anorexia nervosa". The International Journal of Eating Disorders. 27 (2): 125–39. doi:10.1002/(SICI)1098-108X(200003)27:2<125::AID-EAT1>3.0.CO;2-4. PMID 10657886.
- ↑ Corstorphine E (2006). "Cognitive Emotional Behavioural Therapy for the eating disorders; working with beliefs about emotions". European Eating Disorders Review. 14 (6): 448–461. doi:10.1002/erv.747.
- ↑ Frisch MJ, Franko DL, Herzog DB (2006). "Arts-based therapies in the treatment of eating disorders". Eating Disorders. 14 (2): 131–42. doi:10.1080/10640260500403857. PMID 16777810.
- ↑ Latner JD, Wilson GT (September 2000). "Cognitive-behavioral therapy and nutritional counseling in the treatment of bulimia nervosa and binge eating" (PDF). Eating Behaviors. 1 (1): 3–21. CiteSeerX 10.1.1.578.4563. doi:10.1016/S1471-0153(00)00008-8. PMID 15001063. Archived (PDF) from the original on 2020-11-26. Retrieved 2020-08-02.
- ↑ Perelygina L, Patrusheva I, Manes N, Wildes MJ, Krug P, Hilliard JK (May 2003). "Quantitative real-time PCR for detection of monkey B virus (Cercopithecine herpesvirus 1) in clinical samples". Journal of Virological Methods. 109 (2): 245–51. doi:10.1016/S0166-0934(03)00078-8. PMID 12711069.
- ↑ Whisenant SL, Smith BA (October 1995). "Eating disorders: current nutrition therapy and perceived needs in dietetics education and research". Journal of the American Dietetic Association. 95 (10): 1109–12. doi:10.1016/S0002-8223(95)00301-0. PMID 7560681.
- ↑ American Dietetic Association (December 2006). "Position of the American Dietetic Association: Nutrition intervention in the treatment of anorexia nervosa, bulimia nervosa, and other eating disorders". Journal of the American Dietetic Association. 106 (12): 2073–82. doi:10.1016/j.jada.2006.09.007. PMID 17186637.
- ↑ Casper RC (2002). "How useful are pharmacological treatments in eating disorders?". Psychopharmacology Bulletin. 36 (2): 88–104. PMID 12397843.
- ↑ Goldberg SC, Halmi KA, Eckert ED, Casper RC, Davis JM (January 1979). "Cyproheptadine in anorexia nervosa". The British Journal of Psychiatry. 134: 67–70. doi:10.1192/bjp.134.1.67. PMID 367480.
- ↑ Walsh BT, Wilson GT, Loeb KL, Devlin MJ, Pike KM, Roose SP, et al. (April 1997). "Medication and psychotherapy in the treatment of bulimia nervosa". The American Journal of Psychiatry. 154 (4): 523–31. doi:10.1176/ajp.154.4.523. PMID 9090340.
- ↑ Marrazzi MA, Markham KM, Kinzie J, Luby ED (February 1995). "Binge eating disorder: response to naltrexone". International Journal of Obesity and Related Metabolic Disorders. 19 (2): 143–5. PMID 7735342.
- ↑ Vandereycken W, Pierloot R (December 1982). "Pimozide combined with behavior therapy in the short-term treatment of anorexia nervosa. A double-blind placebo-controlled cross-over study". Acta Psychiatrica Scandinavica. 66 (6): 445–50. doi:10.1111/j.1600-0447.1982.tb04501.x. PMID 6758492.
- ↑ Birmingham CL, Gritzner S (December 2006). "How does zinc supplementation benefit anorexia nervosa?". Eating and Weight Disorders. 11 (4): e109-11. doi:10.1007/BF03327573. PMID 17272939.
- ↑ Perkins SJ, Murphy R, Schmidt U, Williams C (July 2006). "Self-help and guided self-help for eating disorders". The Cochrane Database of Systematic Reviews. 3 (3): CD004191. doi:10.1002/14651858.CD004191.pub2. PMID 16856036. S2CID 45718608.
- ↑ Carter JC, Olmsted MP, Kaplan AS, McCabe RE, Mills JS, Aimé A (May 2003). "Self-help for bulimia nervosa: a randomized controlled trial". The American Journal of Psychiatry. 160 (5): 973–8. doi:10.1176/appi.ajp.160.5.973. PMID 12727703.
- ↑ Thiels C, Schmidt U, Treasure J, Garthe R (September 2003). "Four-year follow-up of guided self-change for bulimia nervosa". Eating and Weight Disorders. 8 (3): 212–7. doi:10.1007/bf03325016. PMID 14649785.
- 1 2 Peterson CB, Mitchell JE, Crow SJ, Crosby RD, Wonderlich SA (December 2009). "The efficacy of self-help group treatment and therapist-led group treatment for binge eating disorder". The American Journal of Psychiatry. 166 (12): 1347–54. doi:10.1176/appi.ajp.2009.09030345. PMC 3041988. PMID 19884223.
- ↑ Delinsky SS, Latner JD, Wilson GT (July 2006). "Binge eating and weight loss in a self-help behavior modification program". Obesity. 14 (7): 1244–9. doi:10.1038/oby.2006.141. PMID 16899805. S2CID 1363953.
- ↑ Bulik CM, Berkman ND, Brownley KA, Sedway JA, Lohr KN (May 2007). "Anorexia nervosa treatment: a systematic review of randomized controlled trials". The International Journal of Eating Disorders. 40 (4): 310–20. doi:10.1002/eat.20367. PMID 17370290. S2CID 10238218.
- ↑ Agras WS (June 2001). "The consequences and costs of the eating disorders". The Psychiatric Clinics of North America. 24 (2): 371–9. doi:10.1016/S0193-953X(05)70232-X. PMID 11416936.
- ↑ Palmer RL, Birchall H, Damani S, Gatward N, McGrain L, Parker L (April 2003). "A dialectical behavior therapy program for people with an eating disorder and borderline personality disorder--description and outcome". The International Journal of Eating Disorders. 33 (3): 281–6. doi:10.1002/eat.10141. PMID 12655624.
- ↑ Baran SA, Weltzin TE, Kaye WH (July 1995). "Low discharge weight and outcome in anorexia nervosa". The American Journal of Psychiatry. 152 (7): 1070–2. doi:10.1176/ajp.152.7.1070. PMID 7793445.
- 1 2 Lock J (2015). "An Update on Evidence-Based Psychosocial Treatments for Eating Disorders in Children and Adolescents". Journal of Clinical Child and Adolescent Psychology. 44 (5): 707–21. doi:10.1080/15374416.2014.971458. PMID 25580937.
- ↑ Hay, Phillipa J.; Touyz, Stephen; Claudino, Angélica M.; Lujic, Sanja; Smith, Caroline A.; Madden, Sloane (2019-01-21). "Inpatient versus outpatient care, partial hospitalisation and waiting list for people with eating disorders". The Cochrane Database of Systematic Reviews. 1: CD010827. doi:10.1002/14651858.CD010827.pub2. ISSN 1469-493X. PMC 6353082. PMID 30663033. Archived from the original on 2021-08-28. Retrieved 2020-08-02.
- ↑ Vandereycken W, Andereycken WV (September 2003). "Prognosis of anorexia nervosa". The American Journal of Psychiatry. 160 (9): 1708, author reply 1708. doi:10.1176/appi.ajp.160.9.1708. PMID 12944354.
- ↑ Bergh C, Brodin U, Lindberg G, Södersten P (July 2002). "Randomized controlled trial of a treatment for anorexia and bulimia nervosa". Proceedings of the National Academy of Sciences of the United States of America. 99 (14): 9486–91. Bibcode:2002PNAS...99.9486B. doi:10.1073/pnas.142284799. PMC 123167. PMID 12082182.
- ↑ Herzog DB, Dorer DJ, Keel PK, Selwyn SE, Ekeblad ER, Flores AT, et al. (July 1999). "Recovery and relapse in anorexia and bulimia nervosa: a 7.5-year follow-up study". Journal of the American Academy of Child and Adolescent Psychiatry. 38 (7): 829–37. doi:10.1097/00004583-199907000-00012. PMID 10405500.
- ↑ Linna MS, Raevuori A, Haukka J, Suvisaari JM, Suokas JT, Gissler M (December 2013). "Reproductive health outcomes in eating disorders". The International Journal of Eating Disorders. 46 (8): 826–33. doi:10.1002/eat.22179. PMID 23996114. S2CID 25589492.
- ↑ Grilo CM, Pagano ME, Stout RL, Markowitz JC, Ansell EB, Pinto A, et al. (March 2012). "Stressful life events predict eating disorder relapse following remission: six-year prospective outcomes". The International Journal of Eating Disorders. 45 (2): 185–92. doi:10.1002/eat.20909. PMC 3275672. PMID 21448971.
- ↑ Illing V, Tasca GA, Balfour L, Bissada H (September 2010). "Attachment insecurity predicts eating disorder symptoms and treatment outcomes in a clinical sample of women". The Journal of Nervous and Mental Disease. 198 (9): 653–9. doi:10.1097/nmd.0b013e3181ef34b2. PMID 20823727.
- ↑ Neumaker, Klaus‐Jürgen (2000). "Mortality rates and causes of death". European Eating Disorders Review. 8 (2): 181–187. doi:10.1002/(SICI)1099-0968(200003)8:2<181::AID-ERV336>3.0.CO;2-#.
- 1 2 3 4 "Health Consequences of Eating Disorders". National Eating Disorder Association. 2017-02-21. Archived from the original on 2015-11-27.
- ↑ Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, et al. (December 2012). "Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010". Lancet. 380 (9859): 2095–128. doi:10.1016/S0140-6736(12)61728-0. hdl:10536/DRO/DU:30050819. PMID 23245604. Archived from the original on 2020-05-19. Retrieved 2020-08-02.
- 1 2 3 Arcelus J, Mitchell AJ, Wales J, Nielsen S (July 2011). "Mortality rates in patients with anorexia nervosa and other eating disorders. A meta-analysis of 36 studies". Archives of General Psychiatry. 68 (7): 724–31. doi:10.1001/archgenpsychiatry.2011.74. PMID 21727255.
- 1 2 3 4 5 6 Roux, H; Chapelon, E; Godart, N (April 2013). "[Epidemiology of anorexia nervosa: a review]". L'Encephale. 39 (2): 85–93. doi:10.1016/j.encep.2012.06.001. PMID 23095584.
- 1 2 Jáuregui-Garrido, Beatriz; Jáuregui-Lobera, Ignacio (2012). "Sudden death in eating disorders". Vascular Health and Risk Management. 8: 91–98. doi:10.2147/VHRM.S28652. ISSN 1176-6344. PMC 3292410. PMID 22393299.
- 1 2 Section D - Eating disorders. (2015, November 27). Retrieved from https://www150.statcan.gc.ca/n1/pub/82-619-m/2012004/sections/sectiond-eng.htm Archived 2020-07-30 at the Wayback Machine.
- ↑ Rushing, Jona M.; Jones, Laura E.; Carney, Caroline P. (2003). "Bulimia Nervosa: A Primary Care Review". Primary Care Companion to the Journal of Clinical Psychiatry. 5 (5): 217–224. doi:10.4088/pcc.v05n0505. ISSN 1523-5998. PMC 419300. PMID 15213788.
- ↑ Hoek, Hans Wijbrand; Hoeken, Daphne van (2003). "Review of the prevalence and incidence of eating disorders". International Journal of Eating Disorders. 34 (4): 383–396. doi:10.1002/eat.10222. ISSN 1098-108X. PMID 14566926.
- 1 2 Dingemans, AE; Bruna, MJ; van Furth, EF (March 2002). "Binge eating disorder: a review". International Journal of Obesity and Related Metabolic Disorders. 26 (3): 299–307. doi:10.1038/sj.ijo.0801949. PMID 11896484.
- 1 2 Ágh, T; Kovács, G; Pawaskar, M; Supina, D; Inotai, A; Vokó, Z (March 2015). "Epidemiology, health-related quality of life and economic burden of binge eating disorder: a systematic literature review". Eating and Weight Disorders. 20 (1): 1–12. doi:10.1007/s40519-014-0173-9. PMC 4349998. PMID 25571885.
- ↑ Le LK, Hay P, Mihalopoulos C (April 2018). "A systematic review of cost-effectiveness studies of prevention and treatment for eating disorders". The Australian and New Zealand Journal of Psychiatry. 52 (4): 328–338. doi:10.1177/0004867417739690. PMID 29113456.
- 1 2 Samnaliev M, Noh HL, Sonneville KR, Austin SB (2015-01-01). "The economic burden of eating disorders and related mental health comorbidities: An exploratory analysis using the U.S. Medical Expenditures Panel Survey". Preventive Medicine Reports. 2: 32–4. doi:10.1016/j.pmedr.2014.12.002. PMC 4721298. PMID 26844048.
- 1 2 Toulany A, Wong M, Katzman DK, Akseer N, Steinegger C, Hancock-Howard RL, Coyte PC (April 2015). "Cost analysis of inpatient treatment of anorexia nervosa in adolescents: hospital and caregiver perspectives". CMAJ Open. 3 (2): E192-7. doi:10.9778/cmajo.20140086. PMC 4565171. PMID 26389097.
- 1 2 de Oliveira C, Macdonald EM, Green D, Colton P, Olmsted M, Bondy S, Kurdyak P (2016-11-03). "Cost evaluation of out-of-country care for patients with eating disorders in Ontario: a population-based study". CMAJ Open. 4 (4): E661–E667. doi:10.9778/cmajo.20160057. PMC 5173482. PMID 28018879.
External links
| Wikiquote has quotations related to: Eating disorder |
| Classification |
|---|
| Library resources about Eating disorder |
- Eating disorder at Curlie