Geographic tongue
| Geographic tongue | |
|---|---|
| Other names: Benign migratory glossitis,[1] glossitis areata migrans, lingua geographica, psoriasiform mucositis, stomatitis areata migrans, wandering rash of the tongue,[2] transitory benign plaques of the tongue[3] | |
 | |
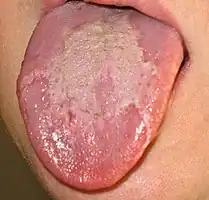
| A patient with geographic tongue | |
| Specialty | Oral Medicine, Oral and Maxillofacial Surgery, Dermatology |
| Symptoms | Burning sensation (rare) |
| Causes | Unknown |
| Diagnostic method | Visual examination |
| Differential diagnosis | Oral lichen planus, erythematous candidiasis, leukoplakia, glossitis, and chemical burns |
| Prevention | None |
| Treatment | Reassurance[4] |
| Medication | None |
| Frequency | 2-3%[4] |
| Deaths | None |
Geographic tongue is a harmless tongue condition with a painless well defined pattern with a slightly irregular raised edge.[1][4]
It is a condition of the mucous membrane of the tongue, usually on the dorsal surface. It is a common condition, affecting approximately 2–3% of the general population.[5][6] It is characterized by areas of smooth, red depapillation (loss of lingual papillae) which migrate over time. The name comes from the map-like appearance of the tongue,[7] with the patches resembling the islands of an archipelago.[5] The cause is unknown, but the condition is entirely benign (importantly, it does not represent oral cancer), and there is no curative treatment. Uncommonly, geographic tongue may cause a burning sensation on the tongue, for which various treatments have been described with little formal evidence of efficacy.
Signs and symptoms
In health, the dorsal surface of the tongue is covered in tuft-like projections called lingual papillae (some of which are associated with taste buds), which give the tongue an irregular surface texture and a white-pink color. Geographic tongue is characterized by areas of atrophy and depapillation (loss of papillae), leaving an erythematous (darker red) and smoother surface than the unaffected areas. The depapillated areas are usually well-demarcated,[2] and bordered by a slightly raised, white, yellow or grey, serpiginous (snaking) peripheral zone.[8] A lesion of geographic tongue may start as a white patch before the depapillation occurs.[2] In certain cases there may be only one lesion, but this is uncommon;[2] the lesions will typically occur in multiple locations on the tongue and coalesce over time to form the typical map-like appearance. The lesions usually change in shape and size, and migrate to other areas, sometimes within hours.[9] The condition may affect only part of the tongue, with a predilection for the tip and the sides of the tongue,[2] or the entire dorsal surface at any one time. The condition goes through periods of remission and relapse. Loss of the white peripheral zone is thought to signify periods of mucosal healing.[8]
There are usually no symptoms other than the unusual appearance of the tongue, but in some cases persons may experience pain or burning, e.g. when eating hot, acidic, spicy or other kinds of foods (e.g. cheese, tomatoes, fruit).[10][9] Where there is a burning symptom, other causes of a burning sensation on the tongue are considered, such as oral candidiasis.[11]
.jpg.webp)


 Fissured tongue combined with geographic tongue
Fissured tongue combined with geographic tongue
Causes
The cause is unknown.[10][12][13] Geographic tongue does not usually cause any symptoms, and in those cases where there are symptoms, an oral parafunctional habit may be a contributory factor.[8] Persons with parafunctional habits related to the tongue may show scalloping on the sides of the tongue (crenated tongue). Some suggest that hormonal factors may be involved,[5] because one reported case in a female appeared to vary in severity in correlation with oral contraceptive use.[2] People with geographic tongue frequently claim that their condition worsens during periods of psychologic stress.[8] Geographic tongue is inversely associated with smoking and tobacco use.[12] Sometimes geographic tongue is said to run in families,[5] and it is reported to be associated with several different genes, though studies show family association may also be caused by similar diets. Some have reported links with various human leukocyte antigens, such as increased incidence of HLA-DR5, HLA-DRW6 and HLA-Cw6 and decreased incidence in HLA-B51.[9] Vitamin B2 deficiency (ariboflavinosis) can cause several signs in the mouth, possibly including geographic tongue,[14] although other sources state that geographic tongue is not related to nutritional deficiency.[5] Fissured tongue often occurs simultaneously with geographic tongue,[10] and some consider fissured tongue to be an end stage of geographic tongue.[8]
In the past, some research suggested that geographic tongue was associated with diabetes, seborrheic dermatitis and atopy, however newer research does not corroborate these findings.[12] Others suggest allergy as a major factor, e.g. to nickel sulphate.[15] Some studies have reported a link between geographic tongue and psoriasis,[16] although 90% of children who are diagnosed with geographic tongue do not develop psoriasis.[13] Again however, modern research studies do not support any link between psoriasis and geographic tongue.[12] Lesions that are histologically indistinguishable from geographic tongue may also be diagnosed in reactive arthritis (arthritis, uveitis/conjunctivitis and urethritis).[8]
Predisposing Factors
Geographic tongue (GT) is a lesion with an unknown origin. However, it has been reported more frequently in people with psoriasis, history of allergies, asthma and rhinitis. Studies have also suggested that psychological/psychiatric factors, diabetes, gastrointestinal diseases and haematological disorders may predispose to GT however, more studies with a larger cohort are needed to determine if GT could be an oral manifestation of a systemic disease.
There is strong evidence to support a high prevalence of coeliac disease and iron-deficiency anaemia in patients with GT. Oral candidiasis and caries are commonly reported in patients with GT, however this can be explained by saliva of a lower pH which will promote the cariogenic process.
Most common areas in which GT can be found include; the lateral border of the tongue, followed by the anterior dorsum of the tongue and ventral surface.[17]
Diagnosis
Diagnosis of Geographic Tongue (GT) mainly relies on clinical, intraoral findings. As GT is usually asymptomatic in the mouth it does not require treatment. A differential diagnosis between oral candidiasis and GT, two similar looking conditions, can be established through a careful and thorough examination. GT is a keratotic lesion which can be described as a round or irregular shaped white plaque, cannot be scraped off and is normally self-resolving.[18] These lesions are known to reoccur within variable periods. Although rare, cytological techniques and biopsies can be done to aid in a clinical diagnosis. The cytological description can define the disease due to its inflammatory characteristics, with its main characteristic being nuclear demarcation. Furthermore, it is important to be aware that GT may be related to other extraoral and intraoral conditions.
The differential diagnosis includes oral lichen planus,[11] erythematous candidiasis,[11] leukoplakia,[11] lupus erythematosus,[9] glossitis,[9] and chemical burns.[5] Atrophic glossitis is usually distinguished from benign migratory glossitis on the basis of the migrating pattern of the lesions and the presence of a whitish border, features which are not present in atrophic glossitis, which instead shows lesions which enlarge rather than migrate.[19] Rarely, blood tests may be required to distinguish from glossitis associated with anemia or other nutritional deficiencies.[9] Since the appearance and the history of the condition (i.e. migrating areas of depapillation) are so striking, there is rarely any need for biopsy.[11] When biopsy is taken, the histopathologic appearance is quite similar to psoriasis:
- Hyperparakeratosis.
- Acanthosis.
- Subepithelial T lymphocyte inflammatory infiltrate.
- Migration of neutrophilic granulocytes into the epithelial layer, which may create superficial microabscesses, similar to the Munro's microabscesses described in pustular psoriasis.[8]
Classification
Geographic tongue could be considered to be a type of glossitis. It usually presents only on the dorsal 2/3 and lateral surfaces of the tongue,[10] but less commonly an identical condition can occur on other mucosal sites in the mouth, such as the ventral surface (undersurface) of the tongue, mucosa of the cheeks or lips, soft palate or floor of mouth; usually in addition to tongue involvement.[11] In such cases, terms such as stomatitis erythema migrans,[11] ectopic geographic tongue,[11] areata migrans,[6] geographic stomatitis,[8] or migratory stomatitis are used instead of geographic tongue. Beside the differences in locations of presentation inside the oral cavity and prevalence among the general population, in all other aspects of clinical significance, symptoms, treatment, and histopathologic appearance, these two forms are identical.
This condition is sometimes termed (oral) erythema migrans, but this has no relation to the more common use of the term erythema migrans (erythema chronicum migrans), to describe the appearance of skin lesions in Lyme disease and southern tick-associated rash illness.[9]
Treatment
Geographic tongue (GT) also termed benign migratory glossitis usually presents without symptoms and due to a lack of reliable evidence, researchers can not identify a specific treatment for the condition. It is currently suggested that patients are given reassurance that the condition is entirely benign and self-resolving.
Although there is no established gold standard treatment confirmed by current evidence, patients with symptomatic GT can be advised on several treatment options prescribed by the clinician on a case-by-case basis. This includes possible prescriptions of antihistamines, anxiolytics, corticosteroids and topical anaesthetics. It is recommended that patients avoid spicy and acidic foods. Research has not shown high levels of evidence for the treatment of symptomatic GT and larger study sizes are needed to come to a reliable recommendation.[20]
Prognosis
The condition may disappear over time, but it is impossible to predict if or when this may happen.[8]
Epidemiology
Geographic tongue is a common condition, affecting 2-3% of the adult general population,[10] although other sources report a prevalence of up to 14%.[12] It is one of the most common tongue disorders that occurs in children.[21] The condition often starts in childhood, sometimes at an early age, but others report that the highest incidence occurs in the over 40 age group.[21] Females are sometimes reported to be more commonly affected than males,[10] in a 2:1 ratio,[2] although others report that the gender distribution is equal.[8]
Clinical Implications
Psoriasis
A recent study has proven the link between geographic tongue (GT) and psoriasis - the presence of geographic tongue can be a predictor of psoriasis. Clinical manifestation of GT and psoriasis can be histologically similar, however a genetic link between the two has been pathogenically identified. Patients with generalised pustular psoriasis and GT both exhibit the c.115 +6T >C mutation in the IL36RN gene. Patients who have GT have been shown to experience a greater severity of psoriasis and have a less positive response to treatment.[22]
Oral Manifestations in Patients with Covid-19
Many articles including case reports, case-series and cross-sectional studies have been done since the recent outbreak of COVID-19, causing a global pandemic. These studies have shown that approximately 20% of patients with COVID-19 can present with mucosal manifestations in their oral cavities, including geographic tongue. Geographic tongue is also thought to appear alongside the onset of the regular symptoms of COVID-19.
Interleukin-6 (IL-6) is known to be an important biomarker in patients with COVID-19 in relation to a cytokine storm where too many inflammatory cells which have a detrimental effect on organ systems throughout the body. Geographic tongue is associated with elevated levels of IL-6, which possibly helps explain it’s presentation on confirmed COVID-19 patients. This evidence is minimal and requires more studies and research to confirm these claims.[23]
Notes
References
- 1 2 James, William D.; Elston, Dirk; Treat, James R.; Rosenbach, Misha A.; Neuhaus, Isaac (2020). "34. Disorders of the mucous membranes". Andrews' Diseases of the Skin: Clinical Dermatology (13th ed.). Edinburgh: Elsevier. p. 799. ISBN 978-0-323-54753-6. Archived from the original on 2023-01-10. Retrieved 2022-05-07.
- 1 2 3 4 5 6 7 Neville BW, Damm DD, Allen CA, Bouquot JE (2002). Oral & maxillofacial pathology (2nd ed.). Philadelphia: W.B. Saunders. pp. 677–679. ISBN 978-0721690032.
- ↑ Rapini, Ronald P.; Bolognia, Jean L.; Jorizzo, Joseph L. (2007). Dermatology: 2-Volume Set. St. Louis: Mosby. ISBN 978-1-4160-2999-1.
- 1 2 3 Jawad, Noor; Skinner, Charlotte (2020). "32. Gastroentrology". Kumar and Clark's Clinical Medicine (10th ed.). Elsevier. p. 1162. ISBN 978-0-7020-7870-5. Archived from the original on 2022-05-08. Retrieved 2022-05-07.
- 1 2 3 4 5 6 Mangione, Salvatore (2012). Physical Diagnosis Secrets: With STUDENT CONSULT Online Access. Elsevier. pp. 604–605. ISBN 978-0323112116. Archived from the original on February 4, 2021. Retrieved November 12, 2012.
- 1 2 Ship, Jonathan A.; Joan Phelan, and A. Ross Kerr (2003). "Chapter 112: Biology and Pathology of the Oral Mucosa". In Freedberg; et al. (eds.). Fitzpatrick's Dermatology in General Medicine (6th ed.). McGraw-Hill. p. 1208. ISBN 0-07-138067-1.
- ↑ Desai, A. B.; Vishwanathan, J. (1989). Textbook Of Paediatrics. India: Orient Blackswan. p. 405. ISBN 978-8125004400. Archived from the original on February 4, 2021. Retrieved November 12, 2012.
- 1 2 3 4 5 6 7 8 9 10 Greenberg, MS; Glick, M; Ship, JA (2008). Burket's oral medicine (11th ed.). Hamilton, Ont.: BC Decker. pp. 103, 104. ISBN 978-1550093452. Archived from the original on 2021-10-31. Retrieved 2022-03-22.
- 1 2 3 4 5 6 7 Scully, Crispian (2008). Oral and maxillofacial medicine : the basis of diagnosis and treatment (2nd ed.). Edinburgh: Churchill Livingstone. p. 205,206. ISBN 9780443068188.
- 1 2 3 4 5 6 Kerawala C, Newlands C (editors) (2010). Oral and maxillofacial surgery. Oxford: Oxford University Press. p. 427. ISBN 9780199204830.
- 1 2 3 4 5 6 7 8 Treister NS, Bruch JM (2010). Clinical oral medicine and pathology. New York: Humana Press. pp. 20, 21. ISBN 978-1-60327-519-4.
- 1 2 3 4 5 Reamy, BV; Derby, R; Bunt, CW (Mar 1, 2010). "Common tongue conditions in primary care". American Family Physician. 81 (5): 627–34. PMID 20187599. Archived from the original on February 27, 2021. Retrieved March 22, 2022.
- 1 2 Cameron, Peter; Jelinek, George; Everitt, Ian (2006). Tratado de Medicina de Urgencias Pediátricas. Elsevier. p. 365. ISBN 978-0443073489. Archived from the original on February 4, 2021. Retrieved November 12, 2012.
- ↑ Tadataka Yamada; David H. Alpers; et al., eds. (2009). Textbook of gastroenterology (5th ed.). Chichester, West Sussex: Blackwell Pub. p. 2547. ISBN 978-1-4051-6911-0.
- ↑ Minciullo, PL; Paolino, G; Vacca, M; Gangemi, S; Nettis, E (1 September 2016). "Unmet diagnostic needs in contact oral mucosal allergies". Clinical and Molecular Allergy. 14 (1): 10. doi:10.1186/s12948-016-0047-y. PMC 5007719. PMID 27587983.
- ↑ Migratory Glossitis (Geographic Tongue) on Maxillofacialcenter.com Archived 2005-11-24 at the Wayback Machine.
- ↑ "Geographic tongue: Predisposing factors, diagnosis and treatment. A systematic review". Archived from the original on 2022-03-11. Retrieved 2022-03-22.
- ↑ Gonzalez-Alvarez. "Geographic tongue: Predisposing factors, diagnosis and treatment. A systematic review". PubMed. Archived from the original on 11 March 2022. Retrieved 11 March 2022.
- ↑ Adeyemo, TA; Adeyemo, WL; Adediran, A; Akinbami, AJ; Akanmu, AS (May–Jun 2011). "Orofacial manifestations of hematological disorders: anemia and hemostatic disorders". Indian Journal of Dental Research. 22 (3): 454–61. doi:10.4103/0970-9290.87070. PMID 22048588.
- ↑ de Campos, Wladimir Gushiken; Esteves, Camila Vieira; Fernandes, Lígia Gonzaga; Domaneschi, Carina; Júnior, Celso Augusto Lemos (September 2018). "Treatment of symptomatic benign migratory glossitis: a systematic review". Clinical Oral Investigations. 22 (7): 2487–2493. doi:10.1007/s00784-018-2553-4. ISSN 1436-3771. PMID 29982968. Archived from the original on 2022-03-13. Retrieved 2022-03-22.
- 1 2 Rioboo-Crespo Mdel, R; Planells-del Pozo, P; Rioboo-García, R (Nov–Dec 2005). "Epidemiology of the most common oral mucosal diseases in children" (PDF). Medicina Oral, Patologia Oral y Cirugia Bucal. 10 (5): 376–87. PMID 16264385. Archived (PDF) from the original on 2021-03-13. Retrieved 2022-03-22.
- ↑ González-Álvarez, Laura; García-Martín, José M.; García-Pola, María José (May 2019). "Association between geographic tongue and psoriasis: A systematic review and meta-analyses". Journal of Oral Pathology & Medicine. 48 (5): 365–372. doi:10.1111/jop.12840. ISSN 1600-0714. PMID 30739339. Archived from the original on 2022-03-13. Retrieved 2022-03-22.
- ↑ Amorim Dos Santos, J.; Normando, A. G. C.; Carvalho da Silva, R. L.; Acevedo, A. C.; De Luca Canto, G.; Sugaya, N.; Santos-Silva, A. R.; Guerra, E. N. S. (November 2021). "Oral Manifestations in Patients with COVID-19: A 6-Month Update". Journal of Dental Research. 100 (12): 1321–1329. doi:10.1177/00220345211029637. ISSN 1544-0591. PMID 34324825. Archived from the original on 2022-03-14. Retrieved 2022-03-22.
External links
| Classification | |
|---|---|
| External resources |