Proteus syndrome
| Proteus syndrome | |
|---|---|
| Other names: Partial gigantism-nevi-hemihypertrophy-macrocephaly syndrome, Wiedemann syndrome | |
 | |
| Alex Green, a 7-year-old boy with Proteus syndrome, confirmed to have the AKT1 p.E17K somatic variant | |
Proteus syndrome is a rare disorder with a genetic background that can cause tissue overgrowth.[1]
People with Proteus syndrome tend to have an increased risk of embryonic tumor development.[2] The clinical and radiographic symptoms of Proteus syndrome are highly variable, as are its orthopedic manifestations.[3][4] The syndrome is named after the Greek sea-god Proteus, who could change his shape. The condition appears to have been first described in the American medical literature by Samia Temtamy and John Rogers in 1976.[5][6] Michael Cohen described it in 1979.[7] Only a few more than 200 cases have been confirmed worldwide, with estimates that about 120 people are currently alive with the condition.[8] As attenuated forms of the disease may exist, there could be many people with Proteus syndrome who remain undiagnosed. Those most readily diagnosed are also the most severely disfigured.
Signs and symptoms

Proteus syndrome causes an overgrowth of skin, bones, muscles, fatty tissues, and blood and lymphatic vessels. Proteus syndrome is a progressive condition wherein children are usually born without any obvious deformities. Tumors of skin and bone growths appear as they age typically in early childhood. The musculoskeletal manifestations are cardinal for the diagnosis of Proteus syndrome.[3] The severity and locations of these various asymmetrical growths vary greatly but typically the skull, one or more limbs, and soles of the feet will be affected. There is a risk of premature death in affected individuals due to deep vein thrombosis and pulmonary embolism caused by the vessel malformations that are associated with this disorder. Because of carrying excess weight and enlarged limbs, arthritis and muscle pain may also be symptoms. Further risks may occur due to the mass of extra tissue.
The disorder itself does not uniformly cause learning impairments: the distribution of intelligence deficits among sufferers of Proteus syndrome appears higher than that of the general population, although this is difficult to determine with statistical significance.[9] In addition, the presence of visible deformity may have a negative effect on the social experiences of the affected individual, causing cognitive and social deficits.
Afflicted individuals are at increased risk for developing certain tumors including unilateral ovarian cystadenomas, testicular tumors, meningiomas, and monomorphic adenomas of the parotid gland.
Hemimegalencephaly is often found to be associated.[10]
Orthopaedic features
The musculoskeletal manifestations of Proteus syndrome are frequent and recognizable. Patients tend to demonstrate a unique pattern of skeletal abnormalities. The orthopaedic features are usually bilateral, asymmetrical, progressive and involving all four limbs and spine. Afflicted patients usually have localized periarticular limb distortions, limb length discrepancy, and spine deformity. Patients with Proteus syndrome can have regular bone configuration and contours despite the bone enlargement.[3] Patients can also exhibit deformation of the skull in the form of dolichocephaly or elongated skull and facial abnormalities. Because of the rarity of the syndrome and the variability of signs, the orthopaedic management should be individualized.[3]
Genetics
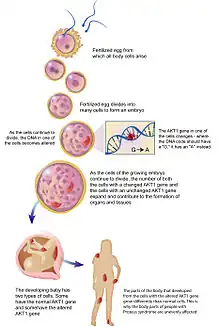
In 2011 researchers determined the cause of Proteus syndrome. In 26 of 29 patients who met strict clinical criteria for the disorder, Lindhurst et al. identified an activating mutation in AKT1 kinase in a mosaic state gene.[11]
Previous research had suggested the condition linked to PTEN on chromosome 10,[12] while other research pointed to chromosome 16.[13] Prior to the findings regarding AKT1 in 2011, other researchers expressed doubt regarding the involvement of PTEN or GPC3, which codes for glypican 3 and may play a role in regulating cell division and growth regulation.[14][15]
Diagnosis
Differential diagnosis
- Macrodystrophia lipomatosa[16]
- Fibrolipomatous hamartoma
- Neurofibromatosis type 1.[17]
- Klippel Trenaunay syndrome.[18]
- Parkes Weber syndrome
- Sotos syndrome
- Hemangiomas.[19]
Classification
Many sources classify Proteus syndrome to be a type of nevus syndrome. The lesions appear to be distributed in a mosaic manner.[20] It has been confirmed that the disorder is an example of genetic mosaicism.[11]
Treatment
A team of doctors in Australia have trial tested the drug rapamycin in the treatment of a patient said to have Proteus syndrome and have found it to be an effective remedy.[21] However, the diagnosis of Proteus syndrome in this patient has been questioned by others.[22] The Proteus syndrome research team in the National Human Genome Research Institute at the United States National Institutes of Health have initiated a Phase 0 dose finding trial with the AKT1 inhibitor ARQ 092, which is being developed by the Arqule Corporation. In earlier tests on tissue and cell samples obtained from patients, ARQ 092 reduced phosphorylation of AKT and downstream targets of AKT in as little as two hours.[23] The Phase 0 trial opened in November 2015.[24] This trial is based on in vitro data showing inhibition of AKT1 in cell lines from patients with Proteus syndrome.[25]
Notable cases
In a 1986 article in the British Medical Journal, Michael Cohen and J.A.R. Tibbles put forward the theory that Joseph Merrick (an Englishman known as the "Elephant Man") had suffered from Proteus syndrome. However, the exact condition suffered by Joseph Merrick is still not known with certainty.[26][27]
Mandy Sellars has been diagnosed by some doctors as suffering from this condition.[8] Her legs and feet have grown at a disproportionate rate since birth. However, in 2013, Sellars' case was profiled on British television in a special called Shrinking My 17 Stone Legs, in which it was determined that Sellars' condition was not, in fact, Proteus syndrome, but rather the often-misdiagnosed PIK3CA-related overgrowth spectrum, a syndrome caused by a PIK3CA gene mutation.
See also
References
- ↑ James, William D.; Elston, Dirk; Treat, James R.; Rosenbach, Misha A.; Neuhaus, Isaac (2020). "27. Genodermatoses and congenital anomalies". Andrews' Diseases of the Skin: Clinical Dermatology (13th ed.). Edinburgh: Elsevier. p. 555. ISBN 978-0-323-54753-6. Archived from the original on 2022-04-18. Retrieved 2022-04-18.
- ↑ Freedberg, et al. (2003). Fitzpatrick's Dermatology in General Medicine. (6th ed.). McGraw-Hill. ISBN 0-07-138076-0.
- 1 2 3 4 El-Sobky, Tamer Ahmed; Elsayed, Solaf M.; El Mikkawy, Dalia M.E. (2015). "Orthopaedic manifestations of Proteus syndrome in a child with literature update". Bone Reports. 3: 104–108. doi:10.1016/j.bonr.2015.09.004. PMC 5365241. PMID 28377973.
- ↑ Jamis-Dow CA, Turner J, Biesecker LG, Choyke PL (2004). "Radiologic manifestations of Proteus syndrome". Radiographics. 24 (4): 1051–68. doi:10.1148/rg.244035726. PMID 15256628.
- ↑ Temtamy SA, Rogers JG (December 1976). "Macrodactyly, hemihypertrophy, and connective tissue nevi: Report of a new syndrome and review of the literature". The Journal of Pediatrics. 89 (6): 924–927. doi:10.1016/S0022-3476(76)80597-5. PMID 993918.
- ↑ Opitz JM, Jorde LB (July 27, 2011). "Hamartoma Syndromes, Exome Sequencing, and a Protean Puzzle". The New England Journal of Medicine. 365 (7): 661–3. doi:10.1056/NEJMe1107384. PMID 21793737.
- ↑ Cohen MM, Hayden PW (1979). "A newly recognized hamartomatous syndrome". Birth Defects Orig. Artic. Ser. 15 (5B): 291–6. PMID 118782.
- 1 2 Woman's 11-stone legs may be lost Archived 2017-12-30 at the Wayback Machine at BBC
- ↑ Turner JT, Cohen MM, Biesecker LG (Oct 1, 2004). "Reassessment of the Proteus syndrome literature: application of diagnostic criteria to published cases". American Journal of Medical Genetics. 130A (2): 111–122. doi:10.1002/ajmg.a.30327. PMID 15372514. S2CID 41588085. Archived (PDF) from the original on August 29, 2021. Retrieved July 6, 2021.
- ↑ Bastos, Halisson; da Silva, Paula Fabiana Sobral; de Albuquerque, Marco Antônio Veloso; Mattos, Adriana; Riesgo, Rudimar Santos; Ohlweiler, Lygia; Winckler, Maria Isabel Bragatti; Bragatti, José Augusto; Duarte, Rodrigo Dias; Zandoná, Denise Isabel (June 2008). "Proteus syndrome associated with hemimegalencephaly and Ohtahara syndrome: Report of two cases". Seizure. 17 (4): 378–382. doi:10.1016/j.seizure.2007.11.001. PMID 18082431. S2CID 13492116.
- 1 2 Lindhurst MJ, Sapp JC, Teer JK, Johnston JJ, Finn EM, Peters K, Turner J, Cannons JL, Bick D, Blakemore L, Blumhorst C, Brockmann K, Calder P, Cherman N, Deardorff MA, Everman DB, Golas G, Greenstein RM, Kato BM, Keppler-Noreuil KM, Kuznetsov SA, Miyamoto RT, Newman K, Ng D, O'Brien K, Rothenberg S, Schwartzentruber DJ, Singhal V, Tirabosco R, Upton J, Wientroub S, Zackai EH, Hoag K, Whitewood-Neal T, Robey PG, Schwartzberg PL, Darling TN, Tosi LL, Mullikin JC, Biesecker LG (Aug 18, 2011). "A mosaic activating mutation in AKT1 associated with the Proteus syndrome". N Engl J Med. 365 (7): 611–9. doi:10.1056/NEJMoa1104017. PMC 3170413. PMID 21793738.
- ↑ Smith JM, Kirk EP, Theodosopoulos G, Marshall GM, Walker J, Rogers M, Field M, Brereton JJ, Marsh DJ (2002). "Germline mutation of the tumour suppressor PTEN in Proteus syndrome". J. Med. Genet. 39 (12): 937–40. doi:10.1136/jmg.39.12.937. PMC 1757209. PMID 12471211.
- ↑ Cardoso MT, de Carvalho TB, Casulari LA, Ferrari I (2003). "Proteus syndrome and somatic mosaicism of the chromosome 16". Panminerva Medica. 45 (4): 267–71. PMID 15206168. Archived from the original on 2012-02-29. Retrieved 2021-07-06.
- ↑ Thiffault I, Schwartz CE, Der Kaloustian V, Foulkes WD (October 2004). "Mutation analysis of the tumor suppressor PTEN and the glypican 3 (GPC3) gene in patients diagnosed with Proteus syndrome". Am. J. Med. Genet. A. 130A (2): 123–7. doi:10.1002/ajmg.a.30335. PMID 15372512. S2CID 32014732.
- ↑ "Entrez Gene: GPC3 glypican 3". Archived from the original on 2010-03-07. Retrieved 2021-07-06.
- ↑ Abdulhady, H; El-Sobky, TA; Elsayed, NS; Sakr, HM (11 June 2018). "Clinical and imaging features of pedal macrodystrophia lipomatosa in two children with differential diagnosis review". Journal of Musculoskeletal Surgery and Research. 2 (3): 130. doi:10.4103/jmsr.jmsr_8_18. S2CID 80970016.
- ↑ Friedman, JM (11 January 2018). Neurofibromatosis 1. GeneReviews. University of Washington, Seattle. Archived from the original on 18 January 2017. Retrieved 30 April 2018.
- ↑ Sung, HM; Chung, HY; Lee, SJ; et, al (2015). "Clinical experience of the Klippel-Trenaunay syndrome". Arch Plast Surg. 42 (5): 552–8. doi:10.5999/aps.2015.42.5.552. PMC 4579165. PMID 26430625.
- ↑ Nguyen, TA; Krakowski, AC; Naheedy, JH; Kruk, PG; Friedlander, SF (2015). "Imaging Pediatric Vascular Lesions". Clin Aesthet Dermatol. 8 (12): 27–41. PMC 4689509. PMID 26705446.
- ↑ Biesecker LG, Happle R, Mulliken JB, Weksberg R, Graham JM, Viljoen DL, Cohen MM (1999). "Proteus syndrome: differential diagnosis, and patient evaluation". Am J Med Genet. 84 (5): 389–95. doi:10.1002/(SICI)1096-8628(19990611)84:5<389::AID-AJMG1>3.0.CO;2-O. PMID 10360391.
- ↑ Marsh DJ, Trahair TN, Martin JL, Chee WY, Walker J, Kirk EP, Baxter RC, Marshall GM (April 22, 2008). "Rapamycin treatment for a child with germline PTEN mutation". Nature Clinical Practice Oncology. 5 (6): 357–361. doi:10.1038/ncponc1112. PMID 18431376. S2CID 2870300.
- ↑ Cohen MM, Turner JT, Biesecker LG (November 1, 2003). "Proteus Syndrome: Misdiagnosis with PTEN Mutations". American Journal of Medical Genetics. 122A (4): 323–324. doi:10.1002/ajmg.a.20474. PMID 14518070. S2CID 26811086.
- ↑ Lindhurst, Marjorie J.; Yourick, Miranda R.; Yu, Yi; Savage, Ronald E.; Ferrari, Dora; Biesecker, Leslie G. (2015-12-11). "Repression of AKT signaling by ARQ 092 in cells and tissues from patients with Proteus syndrome". Scientific Reports. 5: 17162. Bibcode:2015NatSR...517162L. doi:10.1038/srep17162. ISSN 2045-2322. PMC 4675973. PMID 26657992.
- ↑ "Dose Finding Trial of ARQ 092 in Children and Adults With Proteus Syndrome". ClinicalTrials.gov. National Human Genome Research Institute (NHGRI). Oct 31, 2015. NCT02594215. Archived from the original on March 28, 2021. Retrieved July 6, 2021.
- ↑ Lindhurst, Marjorie J.; Yourick, Miranda R.; Yu, Yi; Savage, Ronald E.; Ferrari, Dora; Biesecker, Leslie G. (2015). "Repression of AKT signaling by ARQ 092 in cells and tissues from patients with Proteus syndrome". Scientific Reports. 5: 17162. Bibcode:2015NatSR...517162L. doi:10.1038/srep17162. PMC 4675973. PMID 26657992. 17162.
- ↑ Tibbles JA, Cohen MM (1986). "The Proteus syndrome: the Elephant Man diagnosed". Br Med J (Clin Res Ed). 293 (6548): 683–5. doi:10.1136/bmj.293.6548.683. PMC 1341524. PMID 3092979.
- ↑ – Spiring P (2001). "The Improbable Elephant Man". Biologist (London) 48(3) 104. Archived 2012-03-12 at the Wayback Machine, Article in The Sunday Telegraph, Archived 2020-07-09 at the Wayback Machine – BBC News, [http://www.eurekalert.org/pub_releases/2003-07/dhc-ada071803.php – Eurekalert! Archived 2021-01-26 at the Wayback Machine, Article Archived 2021-03-21 at the Wayback Machine in The Daily Telegraph
External links
| Classification |
|
|---|---|
| External resources |
- GeneReviews/NCBI/NIH/UW entry on PTEN Hamartoma Tumor Syndrome (PHTS) Archived 2010-10-05 at the Wayback Machine