This article was medically reviewed by Lacy Windham, MD. Lacy Windham, MD, is a Board-Certified Obstetrician & Gynecologist in Cleveland, Tennessee. Dr. Windham attended medical school at the University of Tennessee Health Science Center in Memphis. Her residency was completed at Eastern Virginia Medical School in Norfolk, Virginia. She was the recipient of multiple awards during her residency training, including Most Outstanding Resident in Maternal Fetal Medicine, Most Outstanding Resident in Oncology, Most Outstanding Resident Overall, and Special Award in Minimally Invasive Surgery.
There are 32 references cited in this article, which can be found at the bottom of the page.
wikiHow marks an article as reader-approved once it receives enough positive feedback. This article received 23 testimonials and 92% of readers who voted found it helpful, earning it our reader-approved status.
This article has been viewed 2,092,396 times.
If you experience itching, burning, or a change in your vaginal discharge, you may have a vaginal infection. You may be able to treat your infection without medication using home remedies, but it’s still important that you consult your doctor so they can diagnose you.
Steps
Diagnosing Vaginal Infections
-
1Recognize the symptoms of BV. Bacterial vaginosis is typically marked by certain symptoms. These include:[1]
- Vaginal discharge with an unpleasant odor, often described as “fishy”.
- Vaginal discharge that is white or grey and may look foamy
- Burning on urination
- Itchiness and irritation around the vagina
- Keep in mind that not all women with BV have symptoms.
-
2Recognize the symptoms of a yeast infection. Yeast infection symptoms can often resemble the symptoms of BV. These symptoms include:[2]
- An abnormal vaginal discharge. The discharge can be a watery, white discharge to a thick, white, and chunky discharge. This is often described as looking like cottage cheese.
- Itching and burning of the vagina and labia
- Painful intercourse
- Painful urination
- Redness and swelling of the area just outside of the vagina.
-
3Recognize the symptoms of trichomoniasis. Symptoms of trichomoniasis (sometimes called “trich”) in women can be:[3]
- Vaginal discharge that is usually smelly or itchy
- Vaginal discharge that is typically frothy or foamy
- Vaginal itching
- Yellow or a gray-green discharge
- Painful urination
-
4Keep track of your menstrual cycle. Vaginal infection symptoms can differ depending on where a woman is in her cycle. This is because the hormonal changes during the menstrual cycle can affect the composition of the bacteria in the vagina and the characteristics of the vaginal environment. [4]
- Knowing your menstrual cycle will help you keep track of changes that you’re experiencing.
-
5Realize that some women experience no symptoms. Many women have BV or trichomoniasis but they do not have any of the tell-tale symptoms.[5]
- If you suspect you might have an infection, see your doctor.
- Trichomoniasis can be transmitted to sexual partners. If you suspect you have trich, see your doctor for a diagnosis and treatment.
-
6Know that the risk of BV increases with certain activities. Most women have probably had at least one experience with BV. There is no specific cause. Essentially anything that disrupts the normal bacterial balance in the vagina can result in BV. The risk of BV increases with:[6]
- Having a new sexual partner
- Having multiple sexual partners
- Having sex without a condom
- Douching
- Using an intrauterine device (IUD) as a method of birth control
-
7Know what increases the risk of yeast infections. Yeast infections, also called candidiasis, are increased by:[7]
- Wearing tight underwear or non-cotton panties. These styles of panties can increase the temperature, the moisture levels and can be irritating.
- A weakened immune system
- Using vaginal douches and/or perfumed feminine hygiene sprays
- Vaginal trauma. This can be scratches in the vagina that occur during insertion of a tampon or other objects, or during rough sex.
-
8Understand how these vaginal infections can occur. These types of infections can occur because of a number of causes.
- In BV, there is no specific cause, but it typically results from an imbalance of the normal bacterial populations.
- Yeast infections can result after antibiotic use; the antibiotics kill off the normal bacterial populations, allowing the yeast to get a “foothold.” They can also come about as a complication of diabetes, or during hormonal changes, including a normal menstrual cycle or the use of birth control.
-
9Visit your doctor. It is important to get the correct diagnosis from a doctor before starting treatment. The treatments for the different forms of vaginal infections can be different, depending on the degree of infection.
- At the doctor’s office, your physician will likely take a sample of the vaginal discharge, ask for a urine sample and perform a vaginal exam. This exam may be uncomfortable but it is usually over quickly. The discharge will be tested for the presence of bacteria, yeast or other organisms such as Trichomonas.
- It’s important to get a specific diagnosis from your doctor. The approaches for treating vaginal infections differ depending on the type of infection.
-
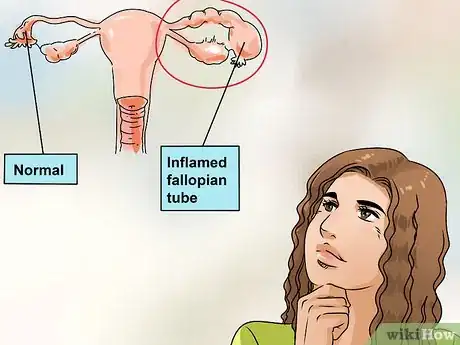
10Know the risks of leaving an infection untreated. Untreated or incorrectly treated BV can result in complications such as pelvic inflammatory disease (PID), pre-term births and low-birth weight babies and put a woman at higher risk of sexually transmitted infections such as HIV, herpes simplex virus (HSV ), chlamydia and gonorrhea. Untreated or incorrectly treated Trichomonas infections can also lead to increased risk of HIV.[8]
-
11See your doctor immediately if you have severe symptoms. If you choose to only use natural remedies, make sure you call your physician if:[9]
- There is no improvement in your symptoms after three days.
- You develop a fever.
- You experience difficulty or pain on urination.
- Sexual activity is painful.
- You have abdominal pain.
- The amount or characteristic of the vaginal discharge increases or changes (such as changing odor or color).
- You have a new rash that appears anywhere on your body.
-
12Tell your doctor you’re planning to use natural treatments. You should always get a diagnosis from your physician when you first start experiencing any of the symptoms. This is because some natural treatments work better for BV or candidiasis, and others may not work as well. You can also use these treatments along with the medications prescribed by your physician. They don’t interfere with oral antibiotics.
- Tell your doctor that you are using these approaches. If you are successful, perhaps your physician can recommend the method to others.
-
13Warn sexual partners if you suspect you have trichomoniasis. Trichomoniasis is classified as a sexually transmitted infection (STI), so if you are diagnosed with trichomoniasis, you should inform any sexual partner so they can be treated as well. [10] ,[11]
- If trichomoniasis is the diagnosis, then home remedies are not appropriate.
Trying Douches to Treat Vaginal Infections
-
1Know the risks of douching. Douching is not generally recommended, because the vagina naturally cleans itself. But, it can be used sparingly when you have BV. You should know, however, that there is a risk of pushing the bacteria into your cervix and uterus and risk PID and other serious infections.
- Douching is actually believed by many physicians to increase the risk of BV.[12]
-
2Try a store-bought douche. Douching is the procedure of washing or cleaning out the inside of the vagina with water or other mixtures of fluids. You can buy prepackaged mixes for douching at most pharmacies and drug stores. These usually come in a bottle with a curved neck or a bag.
- Start by getting into the shower or bath. Most women find it easier to prop one leg on a surface like the edge of the tub. Be careful not to slip.
- Then, with one hand, spread the labia (the “lips” that are on either side of the vagina) and find the vaginal opening.
- Hold the bottle or bag in the other hand.
- Gently squirt the douche upward through the tube or nozzle into your vagina.
- The mixture will come back out through your vagina.
-
3Mix apple cider vinegar with water for a douche. Apple cider vinegar is believed to restore the acidic pH of the vagina.[13] It can be used with relative effectiveness to get rid of BV.
- Get a douche kit from a drugstore. You will use the equipment that is included with the kit. Or, you can use an enema kit, which has the same equipment as a douche kit.
- Mix two tablespoons of apple cider vinegar with one cup of warm filtered water. Don’t use white vinegar, as this is too acidic.
- Use the douche twice a day for four days and then daily until all symptoms disappear. [14]
-
4Try a douche made from hydrogen peroxide. Hydrogen peroxide has disinfectant properties, and it can also get rid of irritants that can cause BV.[15]
- Mix 3% hydrogen peroxide with an equal amount of warm distilled water and douche with this mixture. Use distilled water because the water should be sterile and bacteria-free.
- Use as a douche twice a day for four days and then daily until all symptoms disappear. [16]
-
5Use oregano essential oil and water as a douche. Use two to three drops of essential oregano oil in eight ounces of distilled water. Repeat twice a day for one week. Repeat twice a day for four days and then daily until all symptoms disappear. [17]
- For yeast infections, try douching with two to three drops of essential tea tree oil in eight ounces of distilled water. Repeat twice a day for one week. Repeat twice a day for four days and then daily until all symptoms disappear. Never ingest tea tree oil. [18]
- You can also apply two to three drops of the oil on a tampon and insert the tampon into your vagina. Leave it in for about one hour.
- Do not use essential oil treatments if you are pregnant, nursing, or expect to become pregnant in the immediate future.
Trying Vaginal Suppositories
-
1Try plain yogurt. It sounds messy, and it IS messy. But inserting yogurt into your vagina is a way of re-populating the vagina with harmless bacteria that may be able to “crowd out” the parasite. However, there are no scientific studies that indicate this. [19] , [20] , [21] , [22]
- Use plain yogurt and a 10 mL syringe (you can buy this syringe at your local pharmacy).
- Every night, fill the syringe with the plain yogurt and fill your vagina by inserting the syringe and depressing the plunger.
- Go to bed as usual, but wear a sanitary pad. The messiness comes in the morning when you get out of bed. You should also wear a thin pad during the day.
- Repeat every night until the symptoms disappear.
- You can also use a tampon coated with yogurt, but tampons without the applicator can be difficult and uncomfortable to insert.
-
2Replenish good bacteria with a probiotic suppository. A probiotic will help replenish good bacteria in your body. [23] , [24] , [25]
- Probiotic capsules can be expensive and can be found in most groceries and drugstores. Use gelcap suppositories, since hard suppositories may not be as effective. Buy a brand that has Bifidobacterium longum; Lactobacillus rhamnosus; Bifidobacterium infantis; Lactobacillus acidophilus; or Lactobacillus reuteri HA-188.
- There is not a lot of evidence showing if probiotics as a supplement or in yogurt are helpful in preventing trichomoniasis.
-
3Use periodontal gel. Use Curasept periodontal gel and apply in and around the vagina. Curasept contains 0.5% cyclohexadiene, a disinfectant which has been shown to be effective in treating BV.[26]
-
4Try a clove of garlic. A whole clove of peeled garlic can be inserted into the vagina and has been reported to be helpful in treating BV.[27] This is because the garlic contains allicin, which is a natural antibiotic that fights BV.
- Peel a clove of garlic. Poke some holes in the garlic so that the allicin can be released. Insert the clove into your vagina. Replace the garlic every four hours for seven days or until symptoms have disappeared. [28]
-
5Treat a yeast infection with a boric acid suppository. Boric acid can be irritating, so you shouldn’t make your own suppository. Do not directly apply it to the vagina. Look for Vitanica Yeast Arrest, found in many health food stores. This product is specially formulated for vaginal yeast infections.[29]
- Follow the manufacturer’s instructions for proper usage.
- You must not be the recipient of oral sex while using boric acid because boric acid is poisonous to your partner.
Treating Vaginal Infections if Home Remedies Aren't Working
-
1Get an over-the-counter gel or cream. Most of the gels and creams for vaginal yeast infections that you can get over-the-counter are almost as effective as anti-fungal medications. Examples include Monistat and Gyne-Lotrimin. Use as directed. If you have recurrent infections, use for seven days.[30]
-
2See your doctor about recurring or long-lasting vaginal infections. If you keep getting vaginal infections, or your infection won't go away, make an appointment to see your doctor. Recurrent yeast infections can be a sign of a more serious underlying disorder such as diabetes, cancer or HIV-AIDs.[31]
- If your symptoms don't clear up after three days, talk with your doctor about taking medication. You should also see your doctor if your symptoms return or worsen.
- Your doctor may prescribe an anti-fungal medication to suppress the infection. You will likely need to take this medication every week or month for six months to a year.[32]
-
3Take antibiotics for BV and trichomoniasis. Treatment will depend on the type of infection, how extensive or severe it is and how long you have had the infection. Antibiotics are prescribed for BV and for trichomoniasis, but they are not effective on yeast infections.
- BV is generally treated with either metronidazole or clindamycin. These are considered safe if you are pregnant.
- Male partners usually don’t need treatment, but female partners should be informed and tested.[33]
- Trichomoniasis is usually treated with a single dose of either metronidazole or tinidazole. These are considered safe if you are pregnant.[34]
- Trichomoniasis is a sexually transmitted infection, so make sure your sexual partner(s) are treated as well and wait for seven days after treatment to have sex.[35]
- BV is generally treated with either metronidazole or clindamycin. These are considered safe if you are pregnant.
-
4Treat stubborn vaginal yeast infections with an anti-fungal cream. Vaginal yeast infections can be treated with anti-fungal creams, ointments and vaginal suppositories.
- Examples of these treatments are butoconazole (Gynazole-1), clotrimazole (Gyne-Lotrimin), miconazole (Monistat 3) and terconazole (Terazol 3). Your doctor can prescribe them or they are available (in weaker doses) over-the-counter at your pharmacy.
-
5Treat a long-lasting yeast infection with fluconazole. Vaginal yeast infections can also be treated with a single oral dose of fluconazole (Diflucan). [36] Recurrent or more complicated yeast infections may be treated with higher doses of the medications or you may be asked to take them for a longer period of time.
- Most often, your partner won’t need treatment. However, this may change if you experience recurrent infections.[37]
-
6Use caution if you are pregnant. Pregnant women can experience yeast infections, which should be cleared up before the baby is due. If you still have a yeast infection when the baby is born, it can pass to the baby, causing thrush.[38]
- Check with your doctor about treating vaginal infections during this time.
Preventing Vaginal Infections
-
1Take oral probiotics to prevent BV. You can take probiotics by mouth (either as capsules or in yogurt). These are mainly useful for prevention rather than treatment of BV. If you are prone to BV, eat one serving of yogurt daily (about 150 grams) with four to give billion CFU (Colony Forming Units). Make sure to choose a yogurt that has this information on the label.
- You can also take probiotic capsules according to manufacturer’s recommendations. Experts don’t know exactly how ingested bacterial cultures in yogurt or probiotic supplements can populate the vagina, but there is evidence that they do.[39]
-
2Wash your genital area gently. Use a very mild soap and warm water to wash your genital area. Dry yourself with a clean towel or allow yourself to air dry. You can also try drying it with a blow dryer set on cool.[40]
- Avoid scratching or rubbing your genitals. Keep irritation at a minimum by leaving your genitals alone. Don’t scratch or rub the area.
-
3Wear only white, 100% cotton underwear. Cotton allows your genital area to stay cool and dry. The white underwear avoids irritants that may be in different dyes. Avoid nylon, acetate and any synthetic fibers.
- Avoid wearing thong underwear because these tend to be irritating.
-
4Use a mild detergent for your underwear. Use a mild and fragrance free soap (such as fragrance-free Woolite) for washing your panties. Do not use fabric softeners or dryer sheets. These also contain chemicals that may irritate you.
- Double-rinse your underwear to ensure that all detergent is gone. Detergent residue can cause irritation.
-
5Practice good habits with toileting. Use white, soft toilet tissue. Remember always to wipe from the front to the back to minimize the risk of infection from bowel bacteria.
-
6Use tampons during the day. Instead of using sanitary napkins while you have your period, use tampons during the day. Stay away from deodorant tampons because of the risk of toxic shock syndrome. Replace tampons every few hours, depending on your flow.
- Do not leave tampons in overnight. Use sanitary pads instead.
-
7Avoid wearing pantyhose. Pantyhose do not allow the genital area to “breathe.” They also trap heat and moisture, which creates the perfect setting for bacteria, yeast and other organisms. Instead, wear nylons with a cotton panty insert.
-
8Avoid irritating products. Avoid feminine hygiene products, which can irritate the vulva. These include deodorant sanitary pads, all feminine sprays and deodorants, any products containing Vaseline, oils or greases.
- Avoid bubble baths, bath oils, talc, or powder, especially powder that contains cornstarch. Cornstarch provides food for microorganisms.
When Should You Try This?
-
1Treat vaginal infections after getting diagnosed. While some vaginal infections can be cured without the use of medications, it’s important to consult your OB/GYN or primary physician before beginning any treatment. Effective natural remedies may vary depending on the type of vaginal infection you have and the severity of the infection.
- Since some symptoms are common among multiple types of vaginal infections, self-diagnosis is both difficult and risky. An official diagnosis from your doctor is the only safe way to identify the type and degree of vaginal infection you have.
- Tell your doctor if you have a strong preference for natural remedies. Some doctors are willing to work with you to accommodate this preference, and they should be able to guide you on which remedies would be best to try for your specific needs.
- Note that trichomoniasis is technically an STI. Natural remedies will not be sufficient to cure an infection caused by trichomoniasis; you will need medication to treat it.[41]
-
2Consider home treatment if you aren't pregnant or nursing. While many natural treatments are safe for women with BV or yeast infections, you should avoid most home treatments if you are currently pregnant or may become pregnant, or are currently breastfeeding. Some treatments can inadvertently harm your baby.
- That being said, if you have a vaginal infection during pregnancy, you should still ask your doctor about treatment. Active yeast infections, in particular, can pass to your baby during birth and result in thrush.[42]
-
3Match the right treatment to the correct cause. Some treatments are only effective against certain causes of vaginal infection. To avoid possible complications, you should only try a natural remedy promoted for use against your type of infection; do not use a home remedy suggested for treatment against another type of vaginal infection unless instructed to do so by your doctor.
- As a reminder, douching can be used sparingly if you have BV. It is not recommended for vaginal infections caused by yeast or trichomoniasis. Similarly, periodontal gel and garlic cloves should only be used for BV.
- On the other hand, a yogurt suppository or probiotic suppository might be effective for both yeast and BV.[43]
- Boric acid suppositories are only recommended for use against yeast infections.
-
4Try natural remedies if you can limit or abstain from sexual activity during treatment. Abstaining from sexual activity may not be necessary for all treatments, but you should check with your doctor or do some thorough research to determine if the remedy you’ve chosen is safe to you and your partner before engaging in sexual activity during treatment.
- In particular, exercise extreme caution when taking boric acid suppositories. Boric acid is toxic when ingested, making oral sex especially dangerous.[44]
-
5Use natural remedies while they continue to work. Natural home remedies can cure vaginal infections in some cases, but if your symptoms don’t respond to consistent treatment, contact your doctor again. It is possible that your type and degree of infection can only be cured with medication.
- Vaginal infections—especially those caused by yeast—that won't go away or continually return may suggest a more serious underlying cause, including diabetes, cancer, or certain STIs. While this won't always be the case, it's important to rule out the possibility by asking your doctor to test you.[45]
- If your symptoms worsen or do not improve after three days of treatment, contact your doctor.
- It's important to completely get rid of your vaginal infection. If left untreated, you may suffer from future complications, including pelvic inflammatory disease, an increased risk of pre-term deliveries, and an increased risk of contracting STIs. Even if you think you cured your infection naturally, consider asking your doctor to re-test you to make sure.
Warnings
- Natural methods don’t work for everyone. It is a reasonable choice to take medications, which have 80% to 90% rate of success. It’s not clear what the success rate of natural methods is.⧼thumbs_response⧽
- Pregnant women do not need to try natural remedies, especially if they have BV. BV can lead to preterm labor.⧼thumbs_response⧽
References
- ↑ http://womenshealth.gov/publications/our-publications/fact-sheet/bacterial-vaginosis.html
- ↑ http://www.nlm.nih.gov/medlineplus/ency/article/001511.htm
- ↑ http://www.emedicinehealth.com/trichomoniasis/page3_em.htm#trichomoniasis_symptoms
- ↑ Barousse MM, Theall KP, Van Der Pol B, Fortenberry JD, Orr DP, Fidel PL Jr. Susceptibility of middle adolescent females to sexually transmitted infections: impact of hormone contraception and sexual behaviors on vaginal immunity. Am J Reprod Immunol. 2007 Aug;58(2):159-68.
- ↑ http://www.cdc.gov/std/trichomonas/stdfact-trichomoniasis.htm
- ↑ http://womenshealth.gov/publications/our-publications/fact-sheet/bacterial-vaginosis.html
- ↑ http://www.emedicinehealth.com/trichomoniasis/page3_em.htm#trichomoniasis_symptoms
- ↑ http://www.cdc.gov/std/trichomonas/stdfact-trichomoniasis.htm
- ↑ http://www.emedicinehealth.com/vaginal_infections/page4_em.htm#when_to_seek_medical_care_for_vaginal_infection
- ↑ http://www.emedicinehealth.com/trichomoniasis/page3_em.htm#trichomoniasis_symptoms
- ↑ http://www.emedicinehealth.com/vaginal_infections/page2_em.htm#vaginal_infection_causes
- ↑ Jenny L. Martino and Sten H. Vermund. Vaginal Douching: Evidence for Risks or Benefits to Women's Health. Epidemiol Rev. 2002; 24(2): 109–124.
- ↑ http://www.nationalcandidacenter.com/Vaginal-Yeast-Infection-s/1832.htm
- ↑ http://www.earthclinic.com/cures/bacterial_vaginosis.html
- ↑ http://www.earthclinic.com/cures/hydrogen-peroxide-for-bacterial-vaginosis-bv-treatment.html#sthash.at9rIBq5.dpuf
- ↑ Cardone A, Zarcone R, Borrelli A, Di Cunzolo A, Russo A, Tartaglia E. Utilisation of hydrogen peroxide in the treatment of recurrent bacterial vaginosis. Minerva Ginecol. 55(6), 483–492 (2003).
- ↑ http://www.earthclinic.com/cures/bacterial_vaginosis.html
- ↑ http://www.earthclinic.com/cures/trichomoniasis.html
- ↑ Daniele M, Pascual L, Barberis L. Curative effect of the probiotic strain Lactobacillus fermentum L23 in a murine model of vaginal infection by Gardnerella vaginalis. Letters In Applied Microbiology [serial online]. July 2014;59(1):93-98.
- ↑ Cooper NA, Moores R. A review of the literature regarding nutritional supplements and their effect on vaginal flora and preterm birth.Curr Opin Obstet Gynecol. 2014 Dec;26(6):487-92.
- ↑ Cardone A, Zarcone R, Borrelli A, Di Cunzolo A, Russo A, Tartaglia E. Utilisation of hydrogen peroxide in the treatment of recurrent bacterial vaginosis. Minerva Ginecol. 55(6), 483–492 (2003).
- ↑ Sobel J. Is There a Protective Role for Vaginal Flora?. Current Infectious Disease Reports [serial online]. October 1999;1(4):379-383.
- ↑ Cooper NA, Moores R. A review of the literature regarding nutritional supplements and their effect on vaginal flora and preterm birth.Curr Opin Obstet Gynecol. 2014 Dec;26(6):487-92.
- ↑ Cardone A, Zarcone R, Borrelli A, Di Cunzolo A, Russo A, Tartaglia E. Utilisation of hydrogen peroxide in the treatment of recurrent bacterial vaginosis. Minerva Ginecol. 55(6), 483–492 (2003).
- ↑ Sobel J. Is There a Protective Role for Vaginal Flora?. Current Infectious Disease Reports [serial online]. October 1999;1(4):379-383.
- ↑ http://www.medscape.com/viewarticle/481671_4
- ↑ Yoshida H, Katsuzaki H, Suzuki A, et al. Antimicrobial activity of the thiosulfinates isolated from oil-macerated garlic extract. Bioscience, Biotechnology, And Biochemistry [serial online]. March 1999;63(3):591-594.
- ↑ Van Kessel K, Assefi N, Marrazzo J, Eckert L.Common complementary and alternative therapies for yeast vaginitis and bacterial vaginosis: a systematic review.Obstet Gynecol Surv. 2003 May;58(5):351-8.
- ↑ Van Kessel K, Assefi N, Marrazzo J, Eckert L.Common complementary and alternative therapies for yeast vaginitis and bacterial vaginosis: a systematic review.Obstet Gynecol Surv. 2003 May;58(5):351-8.
- ↑ http://www.prevention.com/health/yeast-infection-treatments
- ↑ http://www.emedicinehealth.com/candidiasis_yeast_infection/article_em.htm
- ↑ http://www.webmd.com/women/oral-medications-for-vaginal-yeast-infections
- ↑ http://womenshealth.gov/publications/our-publications/fact-sheet/bacterial-vaginosis.html
- ↑ http://www.cdc.gov/std/trichomonas/treatment.htm
- ↑ http://www.cdc.gov/std/trichomonas/treatment.htm
- ↑ http://www.mayoclinic.org/diseases-conditions/yeast-infection/basics/treatment/con-20035129
- ↑ http://www.mayoclinic.org/diseases-conditions/yeast-infection/basics/treatment/con-20035129
- ↑ http://americanpregnancy.org/pregnancy-complications/yeast-infections-during-pregnancy/
- ↑ Shalev E, Battino S, Weiner E, Colodner R, Keness Y. Ingestion of yogurt containing Lactobacillus acidophilus compared with pasteurized yogurt as prophylaxis for recurrent candidal vaginitis and bacterial vaginosis. Archives of Family Medicine. 1996;5(10):593–596
- ↑ http://my.clevelandclinic.org/health/healthy_living/hic_Coping_with_Families_and_Careers/hic_Vulvar_Care
- ↑ http://www.emedicinehealth.com/trichomoniasis/page3_em.htm#trichomoniasis_symptoms
- ↑ http://americanpregnancy.org/pregnancy-complications/yeast-infections-during-pregnancy/
- ↑ http://goaskalice.columbia.edu/answered-questions/yogurt-yeast-infections
- ↑ http://www.webmd.com/women/tc/boric-acid-for-vaginal-yeast-infection-topic-overview
- ↑ http://www.emedicinehealth.com/candidiasis_yeast_infection/article_em.htm
About This Article
If you don't know what type of infection you have, see your doctor to get a diagnosis. If it's bacterial vaginosis (BV), use a douche or apply periodontal gel in and around your vagina. If you have a yeast infection, try inserting a yogurt or probiotic suppository into your vagina. Avoid wearing tight underwear or using irritating hygiene products while you have an infection, and talk to your doctor if your infection persists. To learn how to prevent vaginal infections, keep reading.




































-Step-17.webp)


-Step-11-Version-2.webp)



-Step-10.webp)
-Step-13.webp)

-Step-9.webp)














-Step-17.webp)
































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...