This article was medically reviewed by Lacy Windham, MD. Lacy Windham, MD, is a Board-Certified Obstetrician & Gynecologist in Cleveland, Tennessee. Dr. Windham attended medical school at the University of Tennessee Health Science Center in Memphis. Her residency was completed at Eastern Virginia Medical School in Norfolk, Virginia. She was the recipient of multiple awards during her residency training, including Most Outstanding Resident in Maternal Fetal Medicine, Most Outstanding Resident in Oncology, Most Outstanding Resident Overall, and Special Award in Minimally Invasive Surgery.
There are 19 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 43,735 times.
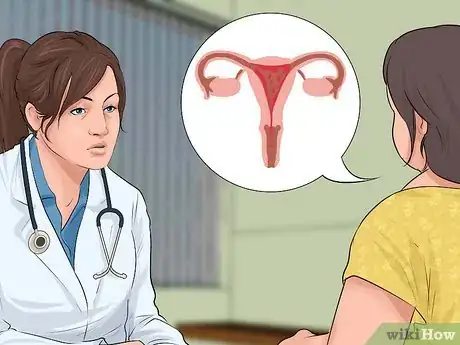
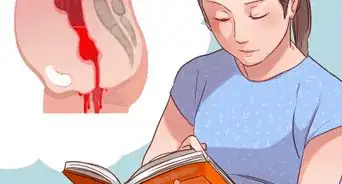
Experts say placenta previa can make you bleed throughout your pregnancy and during delivery, so you may be feeling nervous.[1] Normally, the placenta, which gives your baby nutrients, attaches to the top or side of your uterus. Placenta previa occurs when the placenta attaches to the bottom of your uterus covering your cervix. Research suggests that placenta previa makes it really hard to have a vaginal delivery, so you may need a cesarean section.[2] While you need medical care to treat placenta previa, there are ways to manage your condition to help you have a healthy delivery.
Steps
Diagnosing Placenta Previa
-
1Get regular prenatal care. Most cases of placenta previa are diagnosed during a routine appointment. Whether you have concerns about this condition or not, regular prenatal care is one of the most important aspects of a healthy pregnancy. See your midwife or obstetrician regularly, and do not skip appointments.
- Getting regular care means seeing your doctor as soon as you think you're pregnant. After that, your doctor will schedule appointments as needed.[3]
-
2See your doctor if you notice any vaginal bleeding. In general, you should contact your doctor if you have vaginal bleeding at any point in your pregnancy; it can indicate a potential miscarriage or a number of other problems. If you have bright red bleeding (but no pain) at any point from the second trimester onward, it may also be a symptom of placenta previa.[4]
- Bleeding related to placenta previa can be light or heavy, and it is not necessarily constant; it may stop and then recur.
- If your bleeding is heavy, it's best to go to the emergency room instead of waiting to hear from your doctor.
Advertisement -
3Request an ultrasound. To confirm the presence of placenta previa, your doctor will order an ultrasound to view the location of your placenta. In some cases, you may need to undergo both an abdominal and a transvaginal ultrasound. Transvaginal ultrasounds are performed by inserting a narrow transducer into your vagina.[5]
- You may also need an MRI, but that test is not often done.[6]
-
4Seek help for early contractions. Like bleeding, contractions before your ninth month always merit a visit to your doctor. These contractions might indicate preterm labor or other problems, or they may be a sign of placenta previa.
- It can be difficult to distinguish between true contractions and the normal Braxton-Hicks contractions that many women notice during pregnancy. Do not feel worried or embarrassed about checking with your doctor to be sure. Generally, the cliché that it's better to be safe than sorry applies here.
-
5Ask for a specific diagnosis. If your doctor diagnoses you with placenta previa, ask for the specifics. There are several different kinds, including a low-lying placenta, a partial placenta previa, and a total placenta previa.[7]
- A low-lying placenta means that the placenta is attached to the lower part of your uterus but is not covering the cervix. These cases often resolve themselves before delivery; the placenta may move upward as your pregnancy advances.[8]
- A partial placenta previa means that the placenta is covering part of the cervix, but not all of it. Many of these cases also resolve themselves before delivery.[9]
- A total placenta previa covers the cervical opening completely, making a normal vaginal delivery unlikely. These cases are much less likely to clear up before delivery.[10]
-
6Know the risk factors. Several factors put you more at risk for this condition. For instance, if you are over 30 or have had a pregnancy before, you are at a higher risk for this condition. Also, if you are having more than one baby or if you have scarring in your uterus, you're at higher risk for placenta previa.[11]
- It's important to stop smoking while pregnant for a number of reasons, but it also increases your chance of developing this condition.[12]
Treating Placenta Previa
-
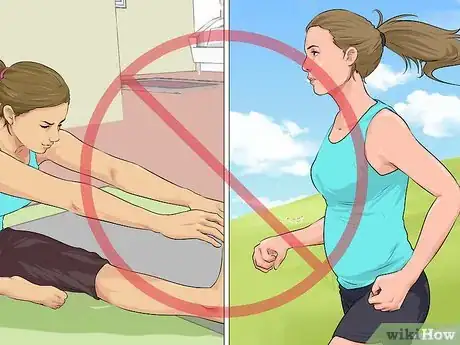
1Slow down. One treatment for placenta previa is just to slow down some. In other words, you'll want to take some of your more strenuous activities off the table. You won't be able to do exercises or many of your normal activities.[13]
- In addition, you shouldn't travel if you have this condition.[14]
-
2Ask your doctor for an explanation if she prescribes bed rest. If you are not experiencing heavy bleeding, your doctor may prescribe bed rest at home. The specifics may vary depending on your particular case, but in general, bed rest is just like it sounds: you'll lie down most of the time and sit or stand only when necessary.[15] However, bed rest can cause health risks, including Deep Vein Thrombosis, so it is less commonly recommended than it used to be.[16] If your doctor recommends bed rest, ask her for her rationale or get a second opinion.
-
3Follow orders about pelvic rest. Pelvic rest means that you cannot perform activities involving your vaginal area. You can't have sex, douche, or wear a tampon, for instance.[17]
-
4Check with your doctor about the severity of your case. If you have a low-lying placenta or a partial placenta previa, the issue may resolve itself. Some women with these mild forms of the condition find that by the time they deliver, the placenta has moved.[18]
-
5Monitor your bleeding. The biggest risk to your health is the heavy bleeding that can accompany placenta previa. Occasionally, women with placenta previa experience uterine hemorrhages that could potentially be fatal. Whether you are at home or in the hospital, watch for signs of heavy bleeding.[19]
- If you notice sudden heavy bleeding, it's best to go to the emergency room.
-
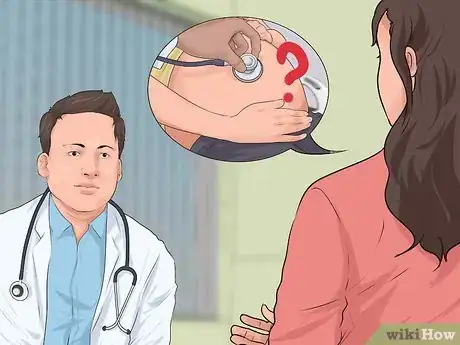
6Understand how future doctor's visits will go. When you have this condition, your doctor will likely limit the time she spends examining you vaginally, as that can exacerbate the condition. In addition, she will use ultrasounds to determine where the baby is over time, and your baby's heartbeat may need to be looked at more closely.[20]
-
7Know what drugs may be used. While medications will not directly treat the condition, you may be given drugs to prolong the pregnancy (so you don't give birth early), as well as corticosteroids to help your baby's lungs develop if you must give birth early. You may also be given blood transfusions due to blood loss.[21]
Coping with Placenta Previa
-
1Be ready to get emergency medical care. Because this condition can become severe, you may need to go to the hospital for medical care at any given point. If you start bleeding or your bleeding becomes suddenly heavier, you need to go to the emergency room.[22]
-
2Consider hospitalization. If you are bleeding moderately to heavily, your doctor may recommend that you enter the hospital. In the hospital, you will be able to lie down most of the time with medical personnel available if any problem arises.[23]
-
3Have a cesarean section if necessary. If your bleeding cannot be controlled or if you or your baby show signs of considerable distress, your doctor may need to perform a cesarean section. This step may be necessary even if you are not yet approaching your due date.[24]
- If you are not bleeding heavily and the placenta is blocking the cervix, you may be able to have a natural birth. However, about 3/4 of women who have this condition in the third trimester are not able to give birth vaginally. Doctors commonly recommend delivering a few weeks early with this condition.[25]
- If you have had a prior cesarean delivery and have placenta previa, you are at higher risk for a condition called placenta accreta. This is a serious condition in which the placenta does not detach after childbirth. You will need to make sure you deliver in a hospital that is prepared for this situation, including having a well-stocked blood bank.[26]
-
4Educate yourself. Read up on placenta previa and cesarean section, which may be a necessary consequence of the condition. Feeling more informed may make you feel less anxious and more in control.
-
5Get support. Talk to your partner or to a trusted friend or relative about any sadness, depression, frustration, worry, or anxiety you may be feeling. It's natural to experience these feelings when your pregnancy does not go as you anticipated, and it's vital to get these emotions out into the open.[27]
- Another option is to join an online support group. Online support groups exist for people with placenta previa and people on bed rest. Consider joining one. These groups can provide much-needed commiseration and suggestions for coping strategies.
-
6Make bed rest as pleasant as possible. If you are stuck in bed, either at home or at the hospital, try to make the best of the situation. Be productive in ways that are compatible with bed rest: research and purchase baby supplies online, write thank you notes to people who have sent gifts, and take care of any work-related obligations that you can do from bed. But don't forget to spend time on the things that will make you feel calmer, happier, or less bored.
- For instance, you could watch your favorite movies or TV shows, read a good book, play computer or video games, have phone or Skype conversations with friends and family members, challenge someone to a board or card game, or keep a journal or a blog.
-
7Don't panic. Having placenta previa is certainly not ideal, and bed rest can be a challenge. However, with proper treatment, you can expect to have a healthy baby, as most women with this condition do.[28]
Warnings
- If you experience heavy bleeding during your pregnancy, whether you have been diagnosed with placenta previa or not, seek medical treatment immediately.⧼thumbs_response⧽
References
- ↑ https://medlineplus.gov/ency/article/000900.htm
- ↑ https://medlineplus.gov/ency/article/000900.htm
- ↑ https://www.womenshealth.gov/publications/our-publications/fact-sheet/prenatal-care.html#a
- ↑ https://www.betterhealth.vic.gov.au/health/healthyliving/placenta-previa
- ↑ https://www.betterhealth.vic.gov.au/health/healthyliving/placenta-previa#diagnosis-methods
- ↑ https://www.ncbi.nlm.nih.gov/books/NBK539818/
- ↑ https://www.ncbi.nlm.nih.gov/books/NBK539818/
- ↑ https://www.ncbi.nlm.nih.gov/books/NBK539818/
- ↑ https://www.nlm.nih.gov/medlineplus/ency/article/000900.htm
- ↑ https://www.nlm.nih.gov/medlineplus/ency/article/000900.htm
- ↑ https://www.ncbi.nlm.nih.gov/books/NBK539818/
- ↑ https://www.msdmanuals.com/professional/gynecology-and-obstetrics/abnormalities-of-pregnancy/placenta-previa
- ↑ https://www.ncbi.nlm.nih.gov/books/NBK539818/
- ↑ http://americanpregnancy.org/pregnancy-complications/placenta-previa/
- ↑ https://www.nlm.nih.gov/medlineplus/ency/article/000900.htm
- ↑ https://my.clevelandclinic.org/health/articles/9757-pregnancy-bed-rest
- ↑ https://www.msdmanuals.com/professional/gynecology-and-obstetrics/abnormalities-of-pregnancy/placenta-previa
- ↑ http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3175253/
- ↑ https://www.uptodate.com/contents/placenta-previa-management
- ↑ http://www.mayoclinic.org/diseases-conditions/placenta-previa/basics/tests-diagnosis/con-20032219
- ↑ https://www.uptodate.com/contents/placenta-previa-management
- ↑ http://www.mayoclinic.org/diseases-conditions/placenta-previa/basics/treatment/con-20032219
- ↑ https://www.betterhealth.vic.gov.au/health/healthyliving/placenta-previa#causes-and-risk-factors
- ↑ https://www.uptodate.com/contents/placenta-previa-management#H24
- ↑ https://www.msdmanuals.com/professional/gynecology-and-obstetrics/abnormalities-of-pregnancy/placenta-previa
- ↑ https://my.clevelandclinic.org/health/diseases/17846-placenta-accreta
- ↑ http://americanpregnancy.org/pregnancy-complications/placenta-previa/
- ↑ http://www.whattoexpect.com/pregnancy/placenta-previa/







































































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...