This article was co-authored by Eric Baron, DO and by wikiHow staff writer, Danielle Blinka, MA, MPA. Dr. Eric P. Baron is a staff ABPN (American Board of Psychiatry and Neurology) board certified Neurologist and a UCNS (United Council for Neurologic Subspecialties) Diplomat board certified in Headache Medicine at Cleveland Clinic Neurological Institute, Center for Neurological Restoration – Headache and Chronic Pain Medicine, in Cleveland, Ohio. With over 15 years of experience practicing medicine, he specializes in helping patients with headaches, migraines, and facial pain. Dr. Baron holds a BS in Biology from the University of Toledo and a DO from The Ohio University Heritage College of Osteopathic Medicine. Following his medical education, he completed his neurology residency and fellowship in headache medicine at Cleveland Clinic. Dr. Baron has authored publications in journals such as The Journal of Headache and Pain and was named one of “America’s Top Physicians."
There are 17 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 25,766 times.
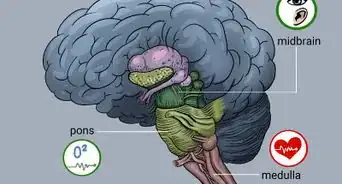
It's normal to be worried if you may have neuropathy, but your healthcare provider can help you manage the condition and minimize symptoms. Neuropathy occurs when your nervous system is damaged, making it hard for your nerves to communicate effectively. This can result in changes in sensation, mobility issues, or problems with your bodily functions. Neuropathy can affect your entire body or can be localized to a particular area. Neuropathy has many causes, including injuries, diseases, disorders, and exposure to toxins. If you suspect that you have neuropathy, visit your healthcare provider to undergo tests to confirm the diagnosis.
Steps
Recognizing Symptoms of Neuropathy
-
1Watch for numbness, prickling, or tingling in your hands or feet. The feeling will come on gradually and may start to spread from your hands and feet up through your arms and legs.[1] If your numbness, prickling, or tingling sensations do not have an obvious cause, such as sitting on your leg for too long or sleeping funny, you should talk to your healthcare provider.[2]
- If your feet are numb, it can change the way that you walk. Over time, the change can affect your body in other ways, such as causing foot deformities or pain from an uneven gait.
- You may also get blisters and sores around the affected areas of your feet because you cannot feel that you are walking unevenly.[3]
-
2Notice if you have pain with no direct external cause. You may experience sharp, jabbing, throbbing, burning, or freezing pain caused from issues within your nerves and not due to an injury.[4] If you’re experiencing pain for no reason, it could be neuropathy.[5]Advertisement
-
3Consider if you have extreme sensitivity to touch. Since your nerves are not responding properly to sensations, you may feel sensations more strongly than you did before. Although this is rare, it could mean that a light pat on the back feels painful to you, or that a hug ignites your pain receptors.[6]
-
4Look for a lack of coordination and a tendency to fall down. If this is caused by neuropathy, it will likely be a recent development and not a lifelong issue with clumsiness. Consider if you’ve been bumping into doors and furniture more often lately, or if you’ve suddenly started to fall down or trip for seemingly no reason.[7]
-
5Notice muscle weakness and paralysis. When your motor nerves are affected by the neuropathy, you’ll experience muscle weakness and possibly paralysis because the nerve can’t appropriately communicate with your muscles. In late stages of neuropathy, you may have trouble moving around, picking things up, or even talking.[8]
-
6Consider if you’ve become heat intolerant or are sweating less. If your autonomic nerves are affected, you may have trouble regulating your bodily functions. This includes telling your body to sweat when you get hot. Your body may not sweat as often, causing you to overheat.[9]
-
7Look for bowel, bladder, or digestive issues. Though these symptoms alone could be caused by a variety of problems, if you have them in conjunction with other symptoms like numbness or pain, they may indicate neuropathy. Neuropathy causes nerve damage, so your nerves may not be able to send messages to your body to tell it when to go to the bathroom, when to process food, and when to stop those functions.[10] It’s possible that you may experience the following symptoms:[11]
- Constipation
- Diarrhea
- Nausea
- Vomiting
- Indigestion
- Problems urinating
- Erectile dysfunction in men
- Lack of vaginal fluid in women
-
8Watch for dizziness and lightheadedness. If you have neuropathy, your body may be unable to regulate your heart rate and blood pressure, so it won’t be able to respond to changes in your activity levels. Your heart rate may remain high even when you are not exercising, and your blood pressure can quickly drop, causing you to feel dizzy. If you have dizziness or lightheadedness along with pain or tingling, it could be neuropathy.
- The dizziness and lightheadedness may be worse when you sit down or stand up.[12]
Getting a Medical Diagnosis
-
1Schedule an appointment with your healthcare provider to get a diagnosis. See your healthcare provider as soon as possible for proper diagnosis and treatment. Your healthcare provider can conduct one or more tests to determine if your symptoms are caused by neuropathy or another medical condition.[13] If neuropathy is the cause, there are treatments available. Your healthcare provider can help you manage and minimize your symptoms.[14]
-
2Prepare a medical and lifestyle history to help identify possible causes. Your healthcare provider will need a complete medical profile, including your family history of neurological diseases. They will also need to understand your lifestyle habits and potential exposure to toxins. They may also ask if you have a history of alcohol abuse.[15]
- This will help them identify the possible cause of your symptoms. If it is neuropathy, your healthcare provider can use your background information to narrow the possible causes and decide which tests to run.
-
3Undergo a neurological examination to check for nerve issues. While it sounds scary, a neurological examination is simple, non-invasive, and easily performed in your healthcare provider's office. Your healthcare provider will check to make sure that your muscles are well developed and properly feeling sensations.[16]
- Then they will check your reflexes, either by tapping your knee to see if your leg reacts or by pricking you with a small needle (which won’t hurt but may be uncomfortable).
- Finally, they will check your posture and coordination to make sure that you walk with balance.
-
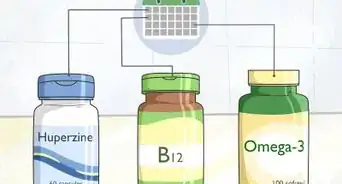
4Have a blood test to look for conditions that cause neuropathy. A blood test will likely be the first test your healthcare provider orders if they suspect neuropathy. You may have a vitamin deficiency, diabetes, or abnormal immune function that could damage your nerves. These conditions could be identified through a blood test, allowing your healthcare provider to make a better diagnosis.[17]
-
5Get an imaging test if the blood test does not reveal a cause. Imaging tests, such as a CT scan or MRI, allow your healthcare provider to get a clearer picture of what’s happening inside your body. While you will need to be still, these tests will not be painful. The healthcare provider will be able to see if you have a herniated disk, tumor, or other abnormality that is affecting your nervous system, resulting in the neuropathy.[18]
-
6Undergo tests to see how well your nerves receive and react to signals. Nerve function tests can be done in either the healthcare provider’s office or a hospital, but are usually a quick outpatient procedure. There are different types of function tests, depending on which type of neuropathy your healthcare provider suspects. Often, they will be done in the same session to make it easier for you. While these tests aren't painful, you may experience discomfort at times as your healthcare provider may use a fine needle to determine if you have nerve damage. Before your tests, bathe or shower, avoiding lotions and moisturizers. Additionally, don't smoke or ingest caffeine for 2 to 3 hours before the tests.[19]
- An electromyography test checks to see how fast your nerves respond to brain signals. A slow response could mean you have damaged nerves.
- Your healthcare provider may order an autonomic test, which just means that they will check how well you're breathing, how your blood pressure reacts to body position changes, if you're sweating properly, and if you're having digestive or bathroom issues. Additionally, they may do an ultrasound.[20]
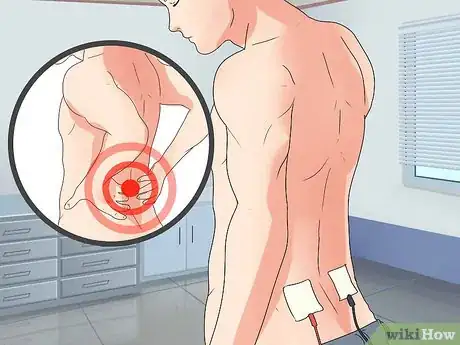
- Sensory tests can show how well you feel touch and vibrations, as well as cold and heat. Your healthcare provider will place a patch on your body that will send vibrations and temperature changes into your body to measure the nerve response. It's a simple, non-invasive test that isn't painful. At most, you may feel uncomfortable at times.[21]
-
7Undergo a nerve biopsy to determine the type and severity of the condition. While a nerve biopsy sounds scary, it's a very simple procedure and is rarely used to determine if you have neuropathy. Your healthcare provider will do it in an outpatient setting and under local anesthesia. The healthcare provider will remove a tiny piece of nerve to examine, most often from your ankle. They will close the small incision with dissolvable stitches and a small amount of plaster. You can usually go home the same day.[22]
- The biopsy will allow the healthcare provider to make a better diagnosis, especially about how serious your condition is. They will also be able to prescribe a better course of treatment to help manage and minimize your symptoms.
Treating Neuropathy
-
1Take pain relievers if your pain is serious. Try over-the-counter pain relievers, including NSAIDs like ibuprofen, Motrin, and Naproxen, if your healthcare provider approves them for your use. If these do not relieve your pain, your healthcare provider may prescribe a stronger pain reliever or refer you to a pain clinic.[23]
- If you don't experience any pain, then you do not need to take pain relievers.
- Always discuss any medications you are taking or plan to take with your healthcare provider and pharmacist to ensure that they are appropriate for you and will not interact with your other medications.
-
2Ask for an anti-seizure medication if pain relievers don't help. Medications that are normally used to treat epilepsy can also be used to treat nerve pain brought on by neuropathy. These medications include Gralise, Neurontin, and Lyrica. Your healthcare provider can determine if they are right for you.
- These medications can cause drowsiness and dizziness.[24]
- Try pain relievers before turning to an anti-seizure medication.
-
3Use topical treatments to help relieve symptoms without oral medication. Topical treatments that can help with nerve pain include capsaicin cream and Lidocaine patches. Capsaicin cream contains a substance found in hot peppers that can help relieve symptoms of neuropathy when it’s absorbed through the skin. Lidocaine patches offer pain relief but require a prescription from your healthcare provider or a pain clinic.[25]
- Only use these medications under your healthcare provider’s supervision.
- Capsaicin cream can cause skin burning and irritation at the application site, which usually goes away after 2 to 4 weeks of continued use. If it does not, you may want to consider a different treatment.
- Lidocaine patches can also cause side effects, including drowsiness, dizziness, and numbness in the area around the patch.[26]
-
4Take an antidepressant if your nerves are over-stimulated. Some antidepressants reduce how much pain you feel by altering the chemical processes in your brain. Your healthcare provider can help you decide if this option may work for you.
- If you use an antidepressant, you may experience side effects, such as dry mouth, nausea, drowsiness, dizziness, decreased appetite, and constipation.[27]
- Only use antidepressants under the supervision of your healthcare provider.
-
5Try TENS therapy to help relieve pain. TENS stands for Transcutaneous Electrical Nerve Stimulation. A healthcare provider or nurse will place electrodes on your skin. During the therapy, a gentle electric current at varying frequencies will travel through the electrodes and into your body, stimulating the nerves. This stimulation should reduce the amount of pain caused by your nerves.
- TENS therapy is usually given daily, with treatments lasting for 30 minutes. Your healthcare provider or therapist can provide you with a portable machine and teach you how to use it at home.[28]
- Your healthcare provider should monitor your usage of a TENS machine.
-
6Use plasma exchange therapy if inflammation is the cause. This treatment can help lower your immune response, which will reduce inflammation in your body that is causing your symptoms. While it sounds complicated, you will just need to allow a healthcare provider to draw your blood and remove the antibodies and proteins. They will then inject the clean blood back into your body.[29]
-
7Complete physical therapy if your muscles have become weak. If you’ve experienced muscle weakness or are recovering from walking issues, a physical therapist can help you retrain your muscles. You may be able to maintain your mobility or correct issues with your walking.
- They can also help you adjust to your adaptive devices, such as hand or foot braces, a cane, a walker, or a wheelchair.[30]
-
8Consider surgery if the neuropathy is caused by pressure. If your neuropathy is localized to 1 area, a tumor could be putting pressure on your nerves. While the tumor may be benign, it should be looked at by your physician, and biopsied and removed by a surgeon if necessary.[31]
Expert Q&A
-
QuestionHow do you know you have neuropathy?
 Eric Baron, DODr. Eric P. Baron is a staff ABPN (American Board of Psychiatry and Neurology) board certified Neurologist and a UCNS (United Council for Neurologic Subspecialties) Diplomat board certified in Headache Medicine at Cleveland Clinic Neurological Institute, Center for Neurological Restoration – Headache and Chronic Pain Medicine, in Cleveland, Ohio. With over 15 years of experience practicing medicine, he specializes in helping patients with headaches, migraines, and facial pain. Dr. Baron holds a BS in Biology from the University of Toledo and a DO from The Ohio University Heritage College of Osteopathic Medicine. Following his medical education, he completed his neurology residency and fellowship in headache medicine at Cleveland Clinic. Dr. Baron has authored publications in journals such as The Journal of Headache and Pain and was named one of “America’s Top Physicians."
Eric Baron, DODr. Eric P. Baron is a staff ABPN (American Board of Psychiatry and Neurology) board certified Neurologist and a UCNS (United Council for Neurologic Subspecialties) Diplomat board certified in Headache Medicine at Cleveland Clinic Neurological Institute, Center for Neurological Restoration – Headache and Chronic Pain Medicine, in Cleveland, Ohio. With over 15 years of experience practicing medicine, he specializes in helping patients with headaches, migraines, and facial pain. Dr. Baron holds a BS in Biology from the University of Toledo and a DO from The Ohio University Heritage College of Osteopathic Medicine. Following his medical education, he completed his neurology residency and fellowship in headache medicine at Cleveland Clinic. Dr. Baron has authored publications in journals such as The Journal of Headache and Pain and was named one of “America’s Top Physicians."
Board Certified Neurologist Neuropathy is often characterized by a combination of numbness, tingling, or burning. However, the pain can be more intense such as electrical, stabbing, or shooting too.
Neuropathy is often characterized by a combination of numbness, tingling, or burning. However, the pain can be more intense such as electrical, stabbing, or shooting too. -
QuestionWhat type of neuropathy affects the feet?
 Eric Baron, DODr. Eric P. Baron is a staff ABPN (American Board of Psychiatry and Neurology) board certified Neurologist and a UCNS (United Council for Neurologic Subspecialties) Diplomat board certified in Headache Medicine at Cleveland Clinic Neurological Institute, Center for Neurological Restoration – Headache and Chronic Pain Medicine, in Cleveland, Ohio. With over 15 years of experience practicing medicine, he specializes in helping patients with headaches, migraines, and facial pain. Dr. Baron holds a BS in Biology from the University of Toledo and a DO from The Ohio University Heritage College of Osteopathic Medicine. Following his medical education, he completed his neurology residency and fellowship in headache medicine at Cleveland Clinic. Dr. Baron has authored publications in journals such as The Journal of Headache and Pain and was named one of “America’s Top Physicians."
Eric Baron, DODr. Eric P. Baron is a staff ABPN (American Board of Psychiatry and Neurology) board certified Neurologist and a UCNS (United Council for Neurologic Subspecialties) Diplomat board certified in Headache Medicine at Cleveland Clinic Neurological Institute, Center for Neurological Restoration – Headache and Chronic Pain Medicine, in Cleveland, Ohio. With over 15 years of experience practicing medicine, he specializes in helping patients with headaches, migraines, and facial pain. Dr. Baron holds a BS in Biology from the University of Toledo and a DO from The Ohio University Heritage College of Osteopathic Medicine. Following his medical education, he completed his neurology residency and fellowship in headache medicine at Cleveland Clinic. Dr. Baron has authored publications in journals such as The Journal of Headache and Pain and was named one of “America’s Top Physicians."
Board Certified Neurologist If the pain is more symmetric such as in both feet and slowly spreading up the legs over time, this suggests more of a blood related problem such as diabetes or other diseases that can affect the nerves more symmetrically.
If the pain is more symmetric such as in both feet and slowly spreading up the legs over time, this suggests more of a blood related problem such as diabetes or other diseases that can affect the nerves more symmetrically. -
QuestionWhat are the causes of neuropathy in the legs?
 Eric Baron, DODr. Eric P. Baron is a staff ABPN (American Board of Psychiatry and Neurology) board certified Neurologist and a UCNS (United Council for Neurologic Subspecialties) Diplomat board certified in Headache Medicine at Cleveland Clinic Neurological Institute, Center for Neurological Restoration – Headache and Chronic Pain Medicine, in Cleveland, Ohio. With over 15 years of experience practicing medicine, he specializes in helping patients with headaches, migraines, and facial pain. Dr. Baron holds a BS in Biology from the University of Toledo and a DO from The Ohio University Heritage College of Osteopathic Medicine. Following his medical education, he completed his neurology residency and fellowship in headache medicine at Cleveland Clinic. Dr. Baron has authored publications in journals such as The Journal of Headache and Pain and was named one of “America’s Top Physicians."
Eric Baron, DODr. Eric P. Baron is a staff ABPN (American Board of Psychiatry and Neurology) board certified Neurologist and a UCNS (United Council for Neurologic Subspecialties) Diplomat board certified in Headache Medicine at Cleveland Clinic Neurological Institute, Center for Neurological Restoration – Headache and Chronic Pain Medicine, in Cleveland, Ohio. With over 15 years of experience practicing medicine, he specializes in helping patients with headaches, migraines, and facial pain. Dr. Baron holds a BS in Biology from the University of Toledo and a DO from The Ohio University Heritage College of Osteopathic Medicine. Following his medical education, he completed his neurology residency and fellowship in headache medicine at Cleveland Clinic. Dr. Baron has authored publications in journals such as The Journal of Headache and Pain and was named one of “America’s Top Physicians."
Board Certified Neurologist If the pain you're feeling is focused in one area such as a leg, it suggests more of a single nerve irritation (such as sciatica pain down the leg). Regardless of the pattern, you should discuss it with your doctor.
If the pain you're feeling is focused in one area such as a leg, it suggests more of a single nerve irritation (such as sciatica pain down the leg). Regardless of the pattern, you should discuss it with your doctor.
References
- ↑ Eric Baron, DO. Board Certified Neurologist. Expert Interview. 13 September 2021.
- ↑ https://www.webmd.com/pain-management/guide/neuropathic-pain
- ↑ https://www.niddk.nih.gov/health-information/diabetes/overview/preventing-problems/nerve-damage-diabetic-neuropathies/peripheral-neuropathy
- ↑ Eric Baron, DO. Board Certified Neurologist. Expert Interview. 13 September 2021.
- ↑ https://www.foundationforpn.org/what-is-peripheral-neuropathy/symptoms/
- ↑ https://my.clevelandclinic.org/health/diseases/14737-neuropathy
- ↑ https://www.foundationforpn.org/what-is-peripheral-neuropathy/causes/vitamin-nutrition-deficiency/
- ↑ https://www.nhs.uk/conditions/peripheral-neuropathy/symptoms/
- ↑ https://www.ninds.nih.gov/Disorders/Patient-Caregiver-Education/Fact-Sheets/Peripheral-Neuropathy-Fact-Sheet
- ↑ https://www.webmd.com/brain/nerve-pain-and-nerve-damage-symptoms-and-causes
- ↑ https://www.niddk.nih.gov/health-information/diabetes/overview/preventing-problems/nerve-damage-diabetic-neuropathies
- ↑ https://www.niddk.nih.gov/health-information/diabetes/overview/preventing-problems/nerve-damage-diabetic-neuropathies
- ↑ Eric Baron, DO. Board Certified Neurologist. Expert Interview. 13 September 2021.
- ↑ https://www.ninds.nih.gov/Disorders/Patient-Caregiver-Education/Fact-Sheets/Peripheral-Neuropathy-Fact-Sheet
- ↑ https://www.mayoclinic.org/diseases-conditions/peripheral-neuropathy/diagnosis-treatment/drc-20352067
- ↑ hhttps://www.ninds.nih.gov/Disorders/Patient-Caregiver-Education/Fact-Sheets/Peripheral-Neuropathy-Fact-Sheet
- ↑ https://www.aafp.org/afp/2010/0401/p887.html
- ↑ https://www.mayoclinic.org/diseases-conditions/peripheral-neuropathy/diagnosis-treatment/drc-20352067
- ↑ https://www.webmd.com/brain/emg-and-nerve-conduction-study#2
- ↑ https://www.ninds.nih.gov/Disorders/Patient-Caregiver-Education/Fact-Sheets/Peripheral-Neuropathy-Fact-Sheet
- ↑ https://care.diabetesjournals.org/content/24/2/250
- ↑ https://med.uth.edu/neurology/specialty-programs/neuromuscular-program/biopsy-services/nerve-biopsy/
- ↑ https://www.mayoclinic.org/diseases-conditions/peripheral-neuropathy/diagnosis-treatment/drc-20352067
- ↑ https://www.mayoclinic.org/diseases-conditions/peripheral-neuropathy/diagnosis-treatment/drc-20352067
- ↑ https://www.mayoclinic.org/diseases-conditions/peripheral-neuropathy/diagnosis-treatment/drc-20352067
- ↑ https://www.mayoclinic.org/diseases-conditions/peripheral-neuropathy/diagnosis-treatment/drc-20352067
- ↑ https://www.mayoclinic.org/diseases-conditions/peripheral-neuropathy/diagnosis-treatment/drc-20352067
- ↑ https://www.webmd.com/pain-management/tc/transcutaneous-electrical-nerve-stimulation-tens-topic-overview
- ↑ https://www.mayoclinic.org/diseases-conditions/peripheral-neuropathy/diagnosis-treatment/drc-20352067
- ↑ https://www.mayoclinic.org/diseases-conditions/peripheral-neuropathy/diagnosis-treatment/drc-20352067
- ↑ https://www.mayoclinic.org/diseases-conditions/peripheral-neuropathy/diagnosis-treatment/drc-20352067













































































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...