This article was co-authored by Chris M. Matsko, MD. Dr. Chris M. Matsko is a retired physician based in Pittsburgh, Pennsylvania. With over 25 years of medical research experience, Dr. Matsko was awarded the Pittsburgh Cornell University Leadership Award for Excellence. He holds a BS in Nutritional Science from Cornell University and an MD from the Temple University School of Medicine in 2007. Dr. Matsko earned a Research Writing Certification from the American Medical Writers Association (AMWA) in 2016 and a Medical Writing & Editing Certification from the University of Chicago in 2017.
There are 13 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 47,599 times.
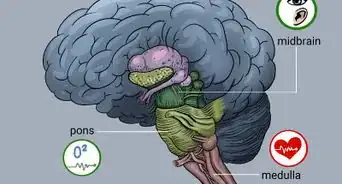
An autonomic dysfunction, also known as an autonomic nerve disorder, occurs when your autonomic nervous system (ANS) breaks down or begins to function abnormally. Your autonomic nervous system controls your involuntary functions, and if you have an autonomic dysfunction, you may experience problems with your blood pressure, your body temperature, perspiration, your heart rate, and your bowel and bladder functions. An autonomic dysfunction can also be caused by another medical issue, like diabetes or an infection.[1] To have a full life with an autonomic dysfunction, it’s important that you identify the underlying symptoms of your condition and treat those symptoms accordingly. There are also coping methods you can use to live and function with your diagnosis.
Steps
Identifying the Symptoms and Underlying Causes
-
1Get an official diagnosis from your doctor. An autonomic dysfunction can be the result of several other disease or disorders. Your doctor will administer tests that correspond with the symptoms you are experiencing and provide you with treatment options based on their diagnosis.[2] Some autonomic dysfunctions can improve over time with the right treatment, but other autonomic dysfunctions have no cure and the goal of treatment will be to maintain your standard of living and manage your symptoms.[3]
- If you have a condition that increases your risk of developing an autonomic dysfunction, like diabetes, your doctor may perform a physical exam and ask you questions about your symptoms. Other treatments, like cancer treatment with a drug known to cause nerve damage, can lead to an autonomic dysfunction. Your doctor may check for signs of an autonomic dysfunction if you are on drugs for cancer treatment.
- If you have symptoms of an autonomic dysfunction, but no obvious risk factors, your doctor may run other tests to confirm your diagnosis. They will review your medical history, ask you about your symptoms, and conduct a physical exam to check for several other disorders or diseases.
- If you have type 2 diabetes, you should be screened annually for an autonomic dysfunction as soon as you receive your diagnosis. If you have type 1 diabetes, you should be screened annually for an autonomic dysfunction five years after your diagnosis.
-
2Recognize the most common symptoms associated with an autonomic dysfunction. There are several common medical issues that can occur as a result of an autonomic dysfunction:[4]
- Urinary issues: You may have difficulty urinating, incontinence or involuntary leaking of urine, or chronic urinary tract infections.
- Digestive issues: You may feel full after only a few bites of food, have a complete loss of appetite, constipation, diarrhea, bloating in the abdominal area, nausea, vomiting, a hard time swallowing, or heartburn.
- Sexual difficulties: Men may have difficulty achieving or maintaining an erection, also known as erectile dysfunction, or ejaculation issues. Women may experience vaginal dryness, low sex drive, or difficulty achieving an orgasm.
- Heart rate issues: You may experience dizziness or fainting when you stand up due to a sudden drop in your blood pressure. This is called orthostatic hypotension and is common with autonomic dysfunction. You may also have sweating abnormalities, sweating too much or too little. This will make it difficult for you to regulate your body temperature. Your heart rate may stay the same even during exercise, leading to an inability or intolerance of physical activity.
Advertisement -
3Discuss treatment options with your doctor. Once you receive a diagnosis of any underlying causes, your doctor will likely recommend a combination of home treatments and medication. They may also recommend coping methods to help you live a full life with the autonomic dysfunction.[5]
- There are also several alternative medicines you can try to help you manage your symptoms, including acupuncture and electrical nerve stimulation. Always talk to your doctor before using any alternative medicines to ensure it will not have a negative effect.[6]
Treating Your Symptoms
-
1Modify your diet and take medications for digestive issues. To help improve your digestion, you should increase the amount of fiber and fluids in your diet slowly. Doing this over a period of time will prevent you from feeling gassy or bloated. You should also eat smaller meals throughout the day to avoid overloading your digestive system. Drinking more water throughout the day will also encourage your digestive system to function properly.
- Your doctor may suggest taking a fiber supplement like Metamucil or Citrucel to increase the amount of fiber in your body.[7] Avoid foods that contain lactose and gluten to prevent aggravating your digestive system.
- Patients with autonomic dysfunction of the stomach or diabetic gastroparesis should consume small meals four to five times a day. Meals should be low in fat and contain only soluble fiber.
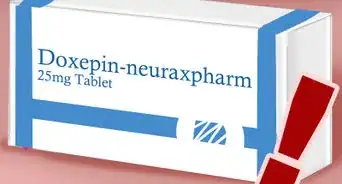
- Your doctor may prescribe medication called metoclopramide (Reglan) to help your stomach empty faster by encouraging your digestive tract to contract; however, this medication can cause drowsiness and may be less effective over time. Your doctor may also recommend medication to help with constipation, such as over-the-counter laxatives. Talk to your doctor about how often you should take these medications.[8]
- Other medications, like antibiotics, can help relieve diarrhea or other bowel issues. Antibiotics can prevent excessive bacterial growth in your intestines, leading to a better functioning digestive system. Erythromycin causes increased functioning of the stomach, and is a prokinetic agent that improves gastric emptying.
- Your doctor may also prescribe antidepressants to treat nerve-related abdominal pain. You may experience side effects like dry mouth and urine retention when on these medications.
-
2Retrain your bladder and take medications for urinary issues. Set up a schedule so you drink fluids and urinate at the same time every day — try to use the bathroom every hour and work up to every three to four hours. This can help to increase your bladder’s capacity and retrain your bladder so it empties at the appropriate times.[9]
- Your doctor may prescribe medication to help empty your bladder, such as bethanechol. You may experience side effects like headache, abdominal cramping, bloating, nausea, and flushing or redness in the face while on this medication.
- Ask your doctor about medication to prevent an overactive bladder, such as tolterodine (Detrol) or oxybutynin (Ditropan XL). You may experience side effects like dry mouth, headache, fatigue, constipation, and abdominal pain while on these drugs.
- Conditioning your pelvic floor muscles may also help. Talk to your doctor about how to isolate and exercise these muscles.
- Your doctor may recommend a more invasive solution like urinary assistance via a catheter. For this procedure, a tube will be guided through your urethra to empty your bladder.
-
3Use medications and other treatments to manage any sexual issues. If you are struggling with erectile dysfunction, your doctor may recommend medications like sildenafil (Viagra), vardenafil (Levitra), or tadalafil (Cialis) to help you achieve and maintain an erection. You may experience side effects like mild headache, flushing or redness of your face, upset stomach, and changes in your ability to see color.[10]
- Use these medications with caution if you have a history of heart disease, arrhythmia, stroke, or high blood pressure. Get immediate medical care if you have an erection that lasts longer than four hours.
- Your doctor may also recommend an external vacuum pump, which helps to pull blood into your penis using a hand pump. This will allow you to maintain an erection for up to 30 minutes.
- For women with sexual issues, your doctor may recommend vaginal lubricants to decrease any dryness and to make intercourse more enjoyable.
-
4Adjust your diet and take heart medications for heart issues or excessive sweating. Your doctor will recommend a high-salt, high-fluid diet if you have a severe case of blood pressure problems. This treatment can cause your blood pressure to spike or your feet, ankles, or legs to swell. Speak to your doctor about the limits of this diet.[11]
- You can also take medication to raise your blood pressure, such as a drug called fludrocortisone. This medication will allow your body to retain salt, thereby regulating your blood pressure. Your doctor may also prescribe other drugs like midodrine or pyridostigmine (Mestinon).
- If you have heart regulation issues, your doctor may prescribe a class of medications called beta blockers. This will help to regulate your heart rate if it goes too high during physical activity.
- If you suffer from excessive sweating, you can take medication called glycopyrrolate (Robinul) to decrease sweating. You may experience side effects like diarrhea, dry mouth, urinary retention, blurred visions, headaches, loss of taste, changes in heart rate, and drowsiness.
-
5Do gentle, low-impact exercises if you have difficulty standing upright. Your heart issues may be coupled with orthostatic hypotension, or difficulty standing upright. It’s important to do gentle seated exercises to build up your muscle tone without the risk of falling down or losing consciousness.
- Water aerobics and water jogging are ideal for individuals with orthostatic intolerance. You can also use an exercise bike to do light cycling and other gentle seated aerobic exercises.
- The use of antihypertensive medication (thiazide diuretics, calcium channel blockers, ACE inhibitors, etc.) can worsen orthostatic hypotension, especially in the elderly.
-
6Adjust your posture and elevate your bed if you have blood pressure issues. Make small adjustments like elevating your bed so the head of your bed is four inches higher. Use blocks or risers under the head of your bed to keep your head raised and help with low blood pressure.[12]
- You should also practice sitting with your legs dangling over the side of your bed for a few minutes before getting out of bed. Try to flex your feet and grip your hands together for a minute before standing to increase blood flow. You should also do basic standing exercises to improve blood flow like tensing your leg muscles and crossing one leg over the other.
-
7Take insulin and monitor your blood sugar to manage your diabetes. You should maintain strict control of your blood glucose by taking your insulin before or after a meal and monitoring your blood sugar levels.[13]
- Doing this will help to lessen your symptoms and delay or prevent more serious issues as a result of your diabetes.
- In addition to symptoms like urinary and digestive issues and erectile dysfunction, you may also experience peripheral neuropathy (numbness) if you have diabetes. Talk to your doctor if you experience any of these issues.
Coping with Your Diagnosis
-
1Talk to a counselor or therapist about your condition. Many people who have an autonomic dysfunction also suffer from depression and anxiety. If you are experiencing impotence or difficulty with sexual arousal, you may have relationship issues with your partner. Talking to a counselor or therapist can help you work through this issues and get professional support.[14]
-
2Join a support group. Talk to your doctor about support groups for autonomic dysfunctions in your area. If there is not a specific group near you, you can look for a support group for your underlying condition, such as a diabetes support group or a sexual difficulties support group.[15]
- It can be helpful to talk to others who understand what you are going through and are dealing with many of the same struggles as you. You may also learn some coping mechanisms from the support group to make life with an autonomic dysfunction easier.
-
3Reach out to family and friends. Lean on those closest to you to create a support system for yourself. Be willing to ask for and accept help when it is needed. Try not to shut yourself off from your family and friends and focus on maintaining a positive attitude to tackle any challenges or struggles you are facing due to your disorder.[16]
References
- ↑ http://www.mayo.edu/research/departments-divisions/department-neurology/programs/autonomic-nerve-disorders
- ↑ https://my.clevelandclinic.org/health/diseases/15631-autonomic-neuropathy-or-autonomic-dysfunction-syncope-information-and-instructions
- ↑ https://www.nlm.nih.gov/medlineplus/autonomicnervoussystemdisorders.html
- ↑ https://www.aafp.org/pubs/afp/issues/2005/0601/p2123.html
- ↑ https://healthcare.utah.edu/neurosciences/neurology/autonomic-dysfunction.php
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3677642/
- ↑ https://my.clevelandclinic.org/health/symptoms/22843-diabetic-diarrhea
- ↑ https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/017854s062lbl.pdf
- ↑ https://my.clevelandclinic.org/health/diseases/15631-autonomic-neuropathy-or-autonomic-dysfunction-syncope-information-and-instructions
- ↑ https://step1.medbullets.com/reproductive/116004/male-sexual-response
- ↑ https://www.niddk.nih.gov/health-information/diabetes/overview/preventing-problems/nerve-damage-diabetic-neuropathies/autonomic-neuropathy
- ↑ https://my.clevelandclinic.org/health/diseases/15631-autonomic-neuropathy-or-autonomic-dysfunction-syncope-information-and-instructions
- ↑ https://www.niddk.nih.gov/health-information/diabetes/overview/preventing-problems/nerve-damage-diabetic-neuropathies/autonomic-neuropathy
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4764485/
- ↑ https://www.dysautonomiasupport.org/
- ↑ https://www.health.harvard.edu/staying-healthy/understanding-the-stress-response
About This Article
To cope with autonomic dysfunction, try to eat smaller meals throughout the day to make it easier for your digestive system. Additionally, ask your doctor about which medications to take, such as antibiotics to relieve bowel issues or metoclopramide to speed up digestion. If you’re having issues urinating, try setting up a schedule so you drink fluids and go to the bathroom at the same times each day, which can help retrain your bladder. For exercise options, try using an exercise bike or doing water aerobics, which will be easier if you’re having difficulty standing upright. To learn more from our Medical co-author, including how to take medication to deal with related heart problems, read on!



































































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...