This article was medically reviewed by Luba Lee, FNP-BC, MS. Luba Lee, FNP-BC is a Board-Certified Family Nurse Practitioner (FNP) and educator in Tennessee with over a decade of clinical experience. Luba has certifications in Pediatric Advanced Life Support (PALS), Emergency Medicine, Advanced Cardiac Life Support (ACLS), Team Building, and Critical Care Nursing. She received her Master of Science in Nursing (MSN) from the University of Tennessee in 2006.
There are 8 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 26,863 times.
Peak flow meters are used for monitoring and controlling asthma, a lung disease that causes repeated episodes of wheezing, coughing, tightness in the chest, and shortness of breath.[1] If you have moderate to severe asthma, your doctor might recommend you use a peak flow meter to help you evaluate the severity of an attack by measuring how efficiently you are pushing air out of your lungs. Peak flow meters are usually available by prescription and can be helpful for anyone with moderate to severe asthma who is over the age of seven years.
Steps
Using Your Meter
-
1Check the meter for obstructions. Peak flow meters only work properly if air is able to freely pass through them. Blowing into a meter that is obstructed by a foreign object will not provide an accurate reading and could cause unnecessary strain on your lungs.
- Peak flow meters usually have an open orifice in the mouthpiece of the device; this is the area most likely to become obstructed, so check here first before use.
- When grasping the meter in your hand, make sure your fingers do not obstruct the sliding scale on top of the device.
-
2Stand or sit up straight. It is important to maintain good posture while using your peak flow meter because this will allow you to maximize your pre-test inhalation as well as your exhalation (which is measured by the device). Slouching or lying down while using the meter will not allow you to get a good reading.[2]Advertisement
-
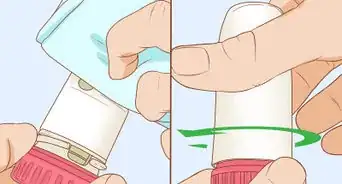
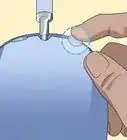
3Set the cursor to zero. The sliding cursor on the back of the peak flow meter is what measures the force of your exhalation. If you do not zero the cursor before you use the meter, your reading will not be accurate.[3]
- You can adjust the cursor by simply placing your finger on it and manually sliding it to the "zero" end of the scale, which is toward the mouthpiece of the meter.
-
4Inhale deeply. In order to register the most powerful exhalation you are capable of, you must first fill your lungs with air. Do this before inserting the peak flow meter into your mouth in order to ensure the fullest inward breath possible.[4]
- Be sure to remove gum or anything else from your mouth before inhaling. Not only do you want to prevent blowing a foreign object into your peak flow meter, but you also don't want to accidentally inhale anything when you take your deep breath in.
-
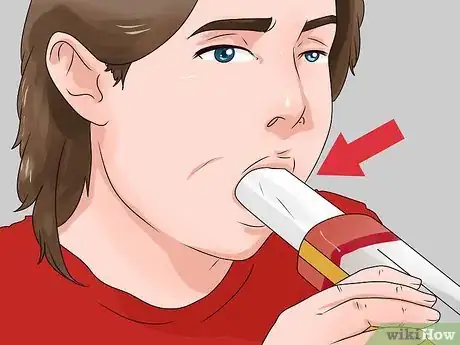
5Place the mouthpiece in your mouth. In order to get the best reading possible on the meter, you should place the mouthpiece between your front teeth and seal your lips around the opening. This will stabilize the meter and ensure that no air escapes from the sides of your mouth when you exhale.[5]
- Pull your tongue backward, away from the mouthpiece, so you do not accidentally block the opening of the meter.
-
6Blow forcefully into the meter. The idea here is to get a hard, fast burst of air out of your lungs to push the sliding cursor on the meter as far as possible down the length of the device. This means that your initial burst of breath is the most important for getting a good reading.[6]
- Don't worry about blowing for a long time or getting all the air out of your lungs when you exhale; only your most forceful rate of exhalation will register on the meter.
- If you cough or sneeze into the device, you will have to do it over again, as these will give you false readings that are higher than your actual peak exhalation.[7]
- Don't forget to write down the meter reading!
-
7Repeat the test twice more. Each time you take a reading using your peak flow meter, you should do the test three times in order to eliminate the possibility that your reading was affected by user or device error. The highest of the three readings is the one you should keep for your records.[8] This is also why it is important to write down each of your test readings as you go.
- Do not average your readings; you need to keep a record of your peak flow rate, which means you need to get the highest reading possible.
- If you don't have enough energy or are out of breath after the first test, make a note of this for your records and stick with your first test reading.
Maximizing the Benefits of Your Meter
-
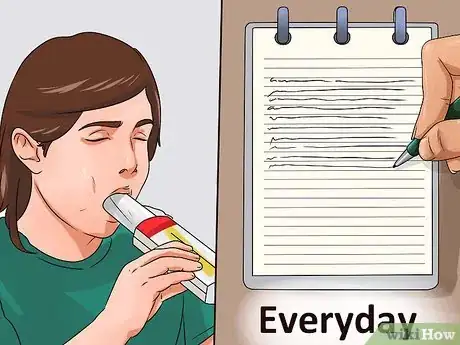
1Take readings every day. In order to track your air flow rate and determine whether your condition is improving, staying the same, or worsening, you need to take readings frequently. It is recommended that you use your peak flow meter once every morning and again in the evening.[9]
- Your readings will be most consistent if you take them at the same time(s) each day.
- If you become ill and experience more difficulty than usual breathing, testing your peak flow will not be beneficial. In fact, doing so could skew your records such that you notice a false improvement in your asthma once you are no longer sick.
-
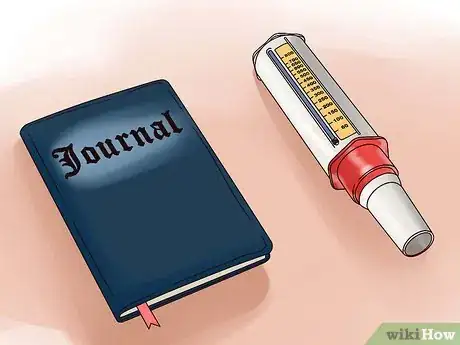
2Keep a journal. This is essential to monitoring your condition and adopting an appropriate course of action if your asthma worsens. Use your journal to record not only your peak flow readings, but also any additional details about your condition that you think might be useful for your doctor to know.[10]
- Your journal should include information about your daily readings (including time of day), your personal best peak flow rate, any unusual respiratory issues you experience, and details about your testing experiences (for example, if testing causes you to become wheezy or lightheaded).
-
3Share information with your doctor. Take your journal with you any time you go to see your doctor. Information about how your condition may have changed over time is essential for helping your doctor determine the proper course of action.[11]
- Since your doctor might not have time to go through your notes, you should create a summary of important points from your journal. Be sure to at least have your information well-organized so your doctor can find the information he needs.
- If you are up to the challenge, consider creating a chart tracking your peak flow readings over the past few weeks to show your doctor. This can be done by hand or on a computer and is a nice way to visualize any trends that may appear in your flow rate readings.
-
4Find your personal best. It is important to know how your flow rate at any given time stacks up to your personal best reading. Establish your personal best by doing an additional flow test once a day for about two to three weeks. The highest reading over this period will be your personal best, and you can judge all other readings by this benchmark.[12]
- Do your personal best testing between the hours of noon and 2 pm each day.
- Make sure your condition is under control during your several-week personal best testing period. If you become sick during this time, you will likely not find your personal best.
- If you are taking medication for your asthma, make sure you do your personal best tests shortly after taking your medication. This applies to both "quick-relief" medications and those you take regularly to prevent attacks.
-
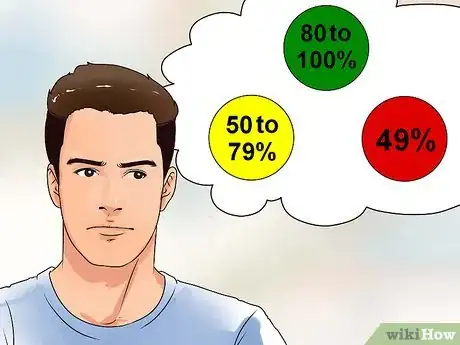
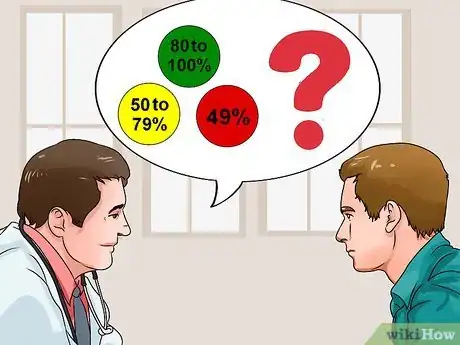
5Track your flow zone. Once you have established a personal best flow reading, you can use this to judge the state of your condition thereafter. Many peak flow meters have indicators built into them that will help you with this, but they must be pre-set with your personal best reading in order to get accurate information.[13]
- There are three flow "zones," which are each based on the a percentage range of your personal best. The green zone is 80 to 100% of your best; the yellow zone is 50 to 79% of your best; and the red zone is 49% or less of your best.
- Use your flow zone to gauge whether your condition is changing and what steps to take in response to those changes (if any).
- If your condition is getting worse and you are already taking daily medication to treat your asthma, you should consider adding quick-relief meds to your normal regimen (but speak to a doctor before taking new or additional medications).
- If your reading is in the red zone at any point, seek immediate medical attention!
-
6Refrain from comparing yourself to others. Everyone is different and as such there are no "standard" readings for peak flow; however, there are expectations for what is "normal," and these are based on your age, sex, height, and race. The only relevant comparisons you can make are to your own previous peak flow readings.[14]
- See your doctor before attempting to determine what your peak flow rate should be.
Warnings
- Never increase medication dosages or begin a new medication without first getting approval from your doctor.⧼thumbs_response⧽
- If at any point you cannot catch your breath or become faint or dizzy during an asthma attack, seek immediate medical attention to avoid a potentially life-threatening situation.⧼thumbs_response⧽
- Always follow your medical provider's instructions.⧼thumbs_response⧽
References
- ↑ https://my.clevelandclinic.org/health/articles/4298-peak-flow-meter
- ↑ https://www.nhs.uk/conditions/peak-flow-test/
- ↑ https://www.lung.org/lung-health-diseases/lung-disease-lookup/asthma/living-with-asthma/managing-asthma/measuring-your-peak-flow-rate
- ↑ https://medlineplus.gov/ency/patientinstructions/000043.htm
- ↑ https://www.aafa.org/asthma/asthma-diagnosis/lung-function-tests/peak-flow-meters.aspx
- ↑ https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/peak-flow-measurement
- ↑ https://www.aafa.org/asthma/asthma-diagnosis/lung-function-tests/peak-flow-meters.aspx
- ↑ https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/peak-flow-measurement
- ↑ https://my.clevelandclinic.org/health/articles/4298-peak-flow-meter
- ↑ https://www.nhs.uk/conditions/peak-flow-test/
- ↑ https://www.lung.ca/lung-health/get-help/how-use-your-inhaler/peak-flow-meter
- ↑ https://medlineplus.gov/ency/patientinstructions/000043.htm
- ↑ https://www.urmc.rochester.edu/encyclopedia/content.aspx?contenttypeid=92&contentid=p07755
- ↑ https://www.lung.org/lung-health-diseases/lung-disease-lookup/asthma/living-with-asthma/managing-asthma/measuring-your-peak-flow-rate
About This Article
To use a peak flow meter, start by standing or sitting up straight so you get the best reading. Additionally, set the cursor to zero on the back of your meter for an accurate reading. Next, inhale as deeply as you can, and place the meter into your mouth with your lips sealed around the opening. Then, blow forcefully into the meter to get your reading, and repeat the test twice more for accuracy. For tips on how to keep a journal of your results, read on!


























































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...