Enoxaparin sodium
Enoxaparin sodium, sold under the brand name Lovenox among others, is an anticoagulant medication (blood thinner).[6] It is used to treat and prevent deep vein thrombosis (DVT) and pulmonary embolism (PE) including during pregnancy and following certain types of surgery.[6] It is also used in those with acute coronary syndrome (ACS) and heart attacks.[6] It is given by injection just under the skin or into a vein.[6] It is also used during hemodialysis.[3][5]
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Lovenox, Clexane, Xaparin, others |
| Biosimilars | Arovi, Inclunox, Inclunox HP, Inhixa, Noromby, Noromby HP, Redesca, Redesca HP, Thorinane |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a696006 |
| License data |
|
| Pregnancy category | |
| Routes of administration | Subcutaneous , intravenous |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Elimination half-life | 4.5 hours |
| Identifiers | |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider |
|
| UNII | |
| KEGG | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.029.698 |
| Chemical and physical data | |
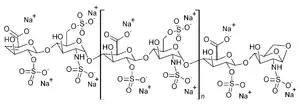
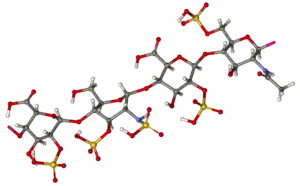
| Formula | (C26H40N2O36S5)n |
| Molar mass | 4500 g/mol (average) |
| | |
Common side effects include bleeding, fever, and swelling of the legs.[6] Bleeding may be serious especially in those who are undergoing a spinal tap.[6] Use during pregnancy appears to be safe for the baby.[6] Enoxaparin is in the low molecular weight heparin family of medications.[6]
Enoxaparin was first made in 1981 and approved for medical use in 1993.[7][6] It is on the World Health Organization's List of Essential Medicines.[8] Enoxaparin is sold under several brand names and is available as a generic medication.[6] Enoxaparin is made from heparin.[7] In 2017, it was the 299th most commonly prescribed medication in the United States, with more than one million prescriptions.[9][10]
Medical uses
- Treatment of unstable angina (UA) and non-Q-wave myocardial infarction (NQMI), administered concurrently with aspirin
- DVT and pulmonary embolism prophylaxis in bed-ridden patients
- DVT prophylaxis in knee replacement surgery
- DVT prophylaxis in hip replacement surgery
- DVT prophylaxis in abdominal surgery
- Treatment of DVT with or without pulmonary embolism
- Treatment of DVT inpatient, with ST-segment elevation myocardial infarction (STEMI)[4]
- Bridging treatment for those with INR below therapeutic range
Monitoring
Enoxaparin has predictable absorption, bioavailability, and distribution therefore monitoring is not typically done. However, there are instances where monitoring may be beneficial for special populations, for example individuals with kidney insufficiency or those that are obese. In this case, anti-Xa units can be measured and dosing adjusted accordingly.[4]
Reversal agent
Protamine sulfate is less effective at reversing enoxaparin compared to heparin, with a maximum neutralization of approximately 60% of the anti-factor Xa effect.[4]
Pregnancy
- Enoxaparin is a FDA pregnancy category B drug which means enoxaparin is not expected to cause harm to an unborn baby when used during pregnancy. This statement is based on reproductive studies involving pregnant rats and rabbits. No birth defects or toxic effects to an unborn fetus due to enoxaparin were observed during these animals studies. However a human's response to enoxaparin might be different from that of a small animal, therefore enoxaparin should be used during pregnancy only if there is a definite need.[4]
- Enoxaparin does not cross the placenta therefore it is unlikely an unborn baby would be exposed to it.[4]
- Some fetal deaths have been reported by women who used enoxaparin during pregnancy, but it is unclear if enoxaparin caused these deaths.[4]
- Pregnant woman on enoxaparin should be monitored on a regular basis for bleeding and/or "excessive anticoagulation" especially when the delivery date is approaching. The risk of hemorrhage is higher during delivery if the person is still using enoxaparin and this could endanger the life of the baby and/or the mother.[4]
- The multiple-dose vials of the brand name enoxaparin (Lovenox) contain 15 mg benzyl alcohol per 1 mL as a preservative. Premature infants who have been given large amounts of benzyl alcohol (99–405 mg/kg/day) have experienced "gasping syndrome".[4][11]
- Although enoxaparin is used to prevent blood clots, pregnancy alone can raise a woman's risk of clotting.[4]
Side effects
Uncommon (<1%)
- In people with unstable angina or non-Q-wave myocardial infarction:
- Atrial fibrillation, heart failure, lung edema, pneumonia: ≥ 0.5%v
Common (>1%)
- Thrombocytopenia, i.e. can be associated with heparin-induced thrombocytopenia (0.5-5.0% of persons treated for at least five days)[12]
- Elevations in serum aminotransferases: 5.9%-6.1%[4]
- In people undergoing abdominal or colorectal surgery:
- Bleeding, anemia, ecchymosis: ≥ 2%[4]
- In persons undergoing hip or knee replacement:
- In persons with severely restricted mobility during acute illness:
- In people being treated for deep vein thrombosis:
Frequency under investigation
- Local reactions: local irritation, pain, hematoma, ecchymosis, erythema[4]
- Bleeding[4]
- Hyperkalemia[4]
- Transaminitis[4]
- Hemorrhage[4]
Boxed warning
The FDA issued a revision to the boxed warning for enoxaparin in October 2013.[13] The revision recommends exercising caution regarding when spinal catheters are placed and removed in persons taking enoxaparin for spinal puncture or neuroaxial anesthesia.[14] It may be necessary to delay anticoagulant dosing in these persons in order to decrease the risk for spinal or epidural hematomas, which can manifest as permanent or long-term paralysis.[14] Persons at risk for hematomas may present with indwelling epidural catheters, concurrent use of medications that worsen bleeding states such as non-steroidal anti-inflammatory drugs (NSAIDs), or a past medical history of epidural or spinal punctures, spinal injury, or spinal deformations.[13] The FDA recommends that at-risk persons be monitored for bleeding and neurological changes.[13][15]
Pharmacology
Mechanism of action
Enoxaparin binds to and potentiates antithrombin (a circulating anticoagulant) to form a complex that irreversibly inactivates clotting factor Xa.[16] It has less activity against factor IIa (thrombin) compared to unfractionated heparin (UFH) due to its low molecular weight.[17]
Pharmacokinetics
Absorption: Bioavailability (subcutaneous injection) ~ 100%[13]
Distribution: Volume of distribution (anti-Factor Xa activity) = 4.3 liters[13]
Metabolism: Enoxaparin is metabolized in the liver into low molecular weight species by either or both desulfation and depolymerization.[13]
Elimination: A single dose of a subcutaneous injection of enoxaparin has an elimination half-life of 4.5 hours.[13] Approximately 10–40% of the active and inactive fragments from a single dose are excreted by the kidneys.[13] Dose adjustments based on kidney function are necessary in persons with reduced kidney function.[13]
Drug class
Enoxaparin belongs to the class of drugs known as low molecular weight heparins. Other drugs in this class include dalteparin, fondaparinux and tinzaparin.[18]
Biosimilars
In September 2016, Inhixa and Thorinane were approved for use in the European Union.[5][19] Thorinane was withdrawn from the market in October 2019.[20]
In March 2017, Enoxaparin BECAT, Laboratorios ROVI (Spain) obtained marketing authorization in twenty six countries in Europe. The product is now available in Europe.[21]
In October 2020, Noromby and Noromby HP, were approved for medical use in Canada.[22]
In November 2020, and Inclunox HP were approved for medical use in Canada.[23]
In December 2020, Redesca and Redesca HP were approved for medical use in Canada.[24]
References
- "Enoxaparin Use During Pregnancy". Drugs.com. 15 July 2019. Retrieved 16 August 2020.
- "Enoxapo Australian prescription medicine decision summary". Therapeutic Goods Administration (TGA). 28 February 2020. Retrieved 17 August 2020.
- "Clexane Forte Syringes - Summary of Product Characteristics (SmPC)". emc. Retrieved 12 October 2020.
- "Lovenox- enoxaparin sodium injection". DailyMed. 28 April 2020. Retrieved 16 August 2020.
- "Inhixa EPAR". European Medicines Agency (EMA). Retrieved 2 April 2020.
- "Enoxaparin Sodium". The American Society of Health-System Pharmacists. Archived from the original on 21 December 2016. Retrieved 8 December 2016.
- Network, Northern Neonatal (2008). Neonatal Formulary: Drug Use in Pregnancy and the First Year of Life. John Wiley & Sons. p. 96. ISBN 9780470750353. Archived from the original on 20 December 2016.
- World Health Organization (2019). World Health Organization model list of essential medicines: 21st list 2019. Geneva: World Health Organization. hdl:10665/325771. WHO/MVP/EMP/IAU/2019.06. License: CC BY-NC-SA 3.0 IGO.
- "The Top 300 of 2020". ClinCalc. Retrieved 11 April 2020.
- "Enoxaparin Sodium - Drug Usage Statistics". ClinCalc. Archived from the original on 28 January 2020. Retrieved 11 April 2020.
- Gershanik, Juan; Boecler, Betty; Ensley, Harry; McCloskey, Sharon; George, William (25 November 1982). "The Gasping Syndrome and Benzyl Alcohol Poisoning". New England Journal of Medicine. 307 (22): 1384–1388. doi:10.1056/NEJM198211253072206. ISSN 0028-4793. PMID 7133084.
- "Reducing Thrombotic Complications in the Perioperative Setti... : Anesthesia & Analgesia" (PDF). LWW. Retrieved 5 November 2015.
- "DailyMed - ENOXAPARIN SODIUM- enoxaparin sodium injection". dailymed.nlm.nih.gov. Archived from the original on 19 October 2015. Retrieved 5 November 2015.
- Research, Center for Drug Evaluation and. "Drug Safety and Availability - FDA Drug Safety Communication: Updated recommendations to decrease risk of spinal column bleeding and paralysis in patients on low molecular weight heparins". www.fda.gov. Archived from the original on 30 October 2015. Retrieved 5 November 2015.
- Commissioner, Office of the. "Safety Information - Lovenox (enoxaparin sodium) injection". www.fda.gov. Archived from the original on 4 March 2016. Retrieved 5 November 2015.
- Alldredge, Brian; Corelli, Robin; Ernst, Michael; Guglielmo, B. Joseph; Jacobson, Pamela; Kradjan, Wayne; Williams, Bradley (February 2012). Koda-Kimble and Young's Applied Therapeutics: The Clinical Use of Drugs (Tenth ed.). pp. 347–348. ISBN 978-1-60913-713-7.
- Trevor, Anthony J., Bertram G. Katzung, and Susan B. Masters. Basic & clinical pharmacology. McGraw-Hill Medical, 2012.
- "LowMolecularWeightHeparins". livertox.nih.gov. Archived from the original on 28 August 2015. Retrieved 5 November 2015.
- "Thorinane EPAR". European Medicines Agency (EMA). Retrieved 2 April 2020.
- "Public statement on Thorinane: Cessation of validity of the marketing authorisation in the European Union" (PDF). Retrieved 2 April 2020.
- "To The National Stock Market Commission" (PDF). Retrieved 29 May 2020.
- "Summary Basis of Decision (SBD) for Noromby/Noromby HP". Health Canada. Retrieved 29 May 2022.
- "Summary Basis of Decision (SBD) for Inclunox/Inclunox HP". Health Canada. Retrieved 29 May 2022.
- "Summary Basis of Decision (SBD) for Redesca/Redesca HP". Health Canada. Retrieved 29 May 2022.
External links
- "Enoxaparin sodium". Drug Information Portal. U.S. National Library of Medicine.