Hyperandrogenism
| Hyperandrogenism | |
|---|---|
| Other names: | |
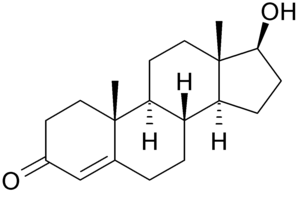 | |
| Testosterone is a type of androgen that is important in the development of hyperandrogenism since high levels of it can cause this condition. | |
| Pronunciation |
|
| Specialty | Endocrinology |
| Symptoms | Acne, hair loss on scalp, increased body or facial hair, infrequent or absent menstruation[1][2] |
| Causes | Polycystic ovary syndrome (PCOS), adrenal hyperplasia, Cushing's disease, cancer[1][3] |
| Diagnostic method | Blood tests, ultrasound[1][4] |
| Treatment | Birth control pills, cyproterone acetate[1] |
| Frequency | 5% (reproductive age women)[2] |
Hyperandrogenism is a medical condition characterized by high levels of androgens in females.[4] Symptoms may include acne, seborrhea (inflamed skin), hair loss on the scalp, increased body or facial hair, and infrequent or absent menstruation.[1][2] Complications may include high blood cholesterol.[4]
The cause in about 70% of cases is polycystic ovary syndrome (PCOS).[1] Other causes include adrenal hyperplasia, Cushing's disease, certain types of cancers, and certain medications.[1][3][4] Diagnosis often involves blood tests for testosterone, 17-hydroxyprogesterone, and prolactin as well as a pelvic ultrasound.[1][4]
Treatment depends on the underlying cause.[4] Symptoms of hyperandrogenism can be improved with birth control pills or antiandrogens such as cyproterone acetate or spironolactone.[1][4] Other measures may include hair removal techniques.[3] It occurs in about 5% of women of reproductive age.[2]
The earliest known descriptions of the condition are by Hippocrates in the 5th century BCE.[5][6] In 2011 the International Association of Athletics Federations ruled that women must have testosterone levels below that of men to compete.[7] There are concerns that these rules are both unscientific and unfair.[7]
Signs and symptoms

Hyperandrogenism affects 5-10% of females of reproductive age.[8] Hyperandrogenism can affect both males and females, but is more noticeable in females since elevated levels of androgens in females often facilitates virilization. Because hyperandrogenism is characterized by the elevation of male sex hormone levels, symptoms of hyperandrogenism in men are often negligible. Hyperandrogenism in females is typically diagnosed in late adolescence with a medical evaluation. The medical evaluation tends to consist of a pelvic exam, observation of external symptoms, and a blood test measuring androgen levels.[9]
- Hirsutism - male-pattern hair growth
- Alopecia - balding
- Masculine appearance
- Hidradenitis suppurativa
- Polycystic ovarian syndrome
- Oligomenorrhea - menstrual irregularities
- Acne
- Obesity
- Infertility
- Deepening of voice
- Oily skin
- Seborrhea - skin inflammation
- Libido - increased sex drive
- Type 2 diabetes
Women
Hyperandrogenism, especially high levels of testosterone, can cause serious adverse effects on women's bodies if left untreated. High testosterone levels have been seen to be associated with obesity, hypertension, amenorrhea (cessation of menstrual cycles), and ovulatory dysfunction, which can lead to infertility. The more prominent signs of hyperandrogenism are hirsutism (unwanted growth of hair especially in the abdominal region and places on the back), acne after adolescence, deepening of voice, and alopecia (balding).[10]
Hyperandrogenism has also been seen to cause individuals to have a high tolerance to insulin, which can lead to type two diabetes, and dyslipidemia, such as high cholesterol. These effects have also been seen to have a large psychological impact on the individual, sometimes leading to societal anxiety and depression, especially in adolescent girls and young women. Paired with obesity and hirsutism, it can cause the individual to have low self-esteem, and a poor view of oneself.[9][11]
Men
Even though hyperandrogenism is not common in men, there have been studies done to look at the effects of high levels of testosterone in males. A study has shown that even though many of the male participants did not have behavior changes due to the increased levels of testosterone, there were cases where the participants had instances of uncharacteristic aggression. High levels of testosterone in males have not been seen to have a direct impact on their personality, but within those studies, there have been cases of sudden aggression within the male participants.[12]
Causes
While hyperandrogenism in women is caused by external factors, it can also appear from natural causes.
Polycystic ovary syndrome

Polycystic ovary syndrome (PCOS) is an endocrine disorder characterized by an excess of androgens produced by the ovaries. It is estimated that approximately 90 percent of women with PCOS demonstrate hypersecretion of these hormones.[13] A concrete cause for this condition is currently unknown. Speculations include genetic predisposition, although the gene or genes in particular have yet to be identified.[14] Evidence suggests that the condition may have a hereditary basis. Other possible causes include the effects from an increase in insulin production. Insulin itself has been observed capable of inducing excess testosterone levels in the ovaries.[15]
Elevated insulin concentration in the body leads to lower production of sex hormone binding globulin (SHBG), a regulatory glycoprotein that suppresses the function of androgens.[16] High blood levels of insulin also work in conjunction with ovarian sensitivity to insulin to cause hyperandrogenemia, the primary symptom of PCOS. Obese individuals may be more biologically inclined to display PCOS due to markedly higher amounts of insulin in their bodies. This hormonal imbalance can lead to chronic anovulation, in which the ovaries experience difficulty releasing mature eggs. These cases of ovulatory dysfunction are linked to infertility and to menstrual disturbances.[13][17]
Hyperthecosis and hyperinsulinemia
Hyperthecosis occurs when the cells of the ovarian stroma transition from interstitial cells, which are cells located in between other cells, into luteinized theca cells. Theca cells are located in the ovarian follicles and become luteinized when the ovarian follicle breaks and a new corpus luteum is formed. The dispersal of luteinized theca cells throughout the ovarian stroma, in contrast to PCOS where the luteinized theca cells are only around cystic follicles, causes women with hyperthecosis to have higher testosterone levels and male-attributed characteristics (virilization) than women with PCOS. Excess levels of insulin in the blood, known as hyperinsulinemia, is also a characteristic of hyperthecosis.[18] Hyperthecosis is mostly seen in postmenopausal women and is linked to acne, hirsutism, growth of the clitoris, baldness, and voice deepening.[19]
Low levels of insulin can also lead to hyperandrogenism. When the body's insulin levels drop too low, it can force itself to produce too much in an effort to make up for the loss. The result of such an overproduction is a disorder called hyperinsulinemia. An effect of hyperinsulinemia is the body's increased production of androgens in the ovaries.[20] This is all part of HAIR-AN syndrome, a multisystem disorder that involves increased insulin levels that prompt increased androgen levels.[21][22]
Cushing’s syndrome
Cushing syndrome develops due to long-term exposure to the hormone cortisol. Cushing's syndrome can either be exogenous or endogenous, depending on whether it is caused by an external or internal source, respectively. The intake of glucocorticoids, which are a type of steroid hormone, is a common cause for the development of exogenous Cushing's syndrome. Endogenous Cushing's syndrome can occur when the body produces excessive amounts of cortisol. This occurs when the hypothalamus of the brain transmits corticotropin-releasing hormone (CRH) to the pituitary gland, which in turn secretes adrenocorticotropin hormone (ACTH). ACTH then causes the adrenal glands to release cortisol into the blood. Signs of Cushing's syndrome include muscle weakness, easy bruising, weight gain, male-pattern hair growth (hirsutism), colored stretch marks, and an excessively reddish complexion in the face.[23] Cushing's syndrome has been shown to cause androgen excess, which directly links it to the signs and symptoms seen in hyperandrogenism.[19]
Congenital adrenal hyperplasia
Congenital adrenal hyperplasia describes a group of autosomal recessive disorders that cause a lack of an enzyme needed for producing cortisol and/or aldosterone, both of which are steroid hormones. Most cases of CAH are due to 21-hydroxylase deficiencies, an enzyme used by the body to produce cortisol and aldosterone. In females, CAH causes uncertainty in the genitals at birth and later on in adolescence excessive pubic hair, enlargement of the clitoris, hirsutism and although it causes rapid growth in childhood adult women with CAH are shorter than average due to early puberty and closure of growth plates. Symptoms in males include early showings of pubic hair, enlargement of the penis, and rapid body and skeletal growth.[24]
Tumors
Adrenocortical carcinoma and tumors
A highly uncommon disease with incidence of 1–2 per million annually. This disease causes cancerous cells to form in the cortex of one or both of the adrenal glands. Adrenocortical tumors produce an additional number of hormones, often leading patients with steroid hormone-producing tumors to develop Cushing's syndrome, Conn syndrome and Hyperandrogenism.[25]
Adenoma of the adrenal gland
Adrenal Adenomas are benign tumors on the adrenal gland. In most cases the tumors display no symptoms and require no treatment. In rare cases, however, some Adrenal Adenomas may become activated, in that they begin to produce hormones in much larger quantities than what adrenal glands tend to produce leading to a number of health complications including Primary aldosteronism and Hyperandrogenism.[26]
Arrhenoblastoma
An arrhenoblastoma is an uncommon tumor of the ovary. It is often composed of sterol cells, leydig cells or some combination of the two. The tumor can produce male or female hormones in the patient and may cause masculinization. In a prepubescent child, a tumor may cause precocious puberty. Malignant Arrhenoblastoma accounts for 30% of all cases of Arrhenoblastoma, the other 70% being largely benign and curable with surgery.[27]
Hilar cell tumor
An ovarian, Androgen producing tumor afflicting older women in most cases and often leading to the development of virilization. This tumor tends to occur around the region of the ovary where the blood vessels enter the organ otherwise known as the hilum. This type of tumor tends to be rather small in size and in most cases could be entirely removed and its symptoms reversed through surgery.[28]
Krukenberg tumor
A quickly developing malignant tumor that is normally found in one of or both ovaries. The tumor is caused by the transcoelomic spread. It primarily grows in the stomach and intestinal regions.[29]
Menopause
One such cause is the end of ovulation and the beginning of menopause. When the body transitions from ovulation to menopause, it stops releasing estrogen at faster rate than it stops releasing androgens. In some cases, estrogen levels can drop enough that there are substantially higher androgen levels leading to hyperandrogenism. A decrease in sex hormone levels while the free androgen index increases helps to aid this process, as well.[30]
Drug-induced
Symptoms generally considered hyperandrogenic can also manifest as results of consuming certain drugs. This can happen according to one of five major mechanisms, namely the direct introduction of androgens to the body, the binding of the drug to androgen receptors and subsequent participation in androgenic action (as is the case with anabolic-androgenic steroids), the reduction of sex hormone-binding globulin plasma concentration that leads to a resulting increase in free testosterone, the interference with and alteration of the hypothalamic–pituitary–ovarian (HPO) axis, or the increase in release of adrenal androgens.[31]
Heredity
Because hyperandrogenism can appear as a symptom of numerous different genetic and medical conditions, it is difficult to make a general statement on whether hyperandrogenic symptoms can be passed from parent to offspring. However, a collection of the conditions with hyperandrogenic symptoms, including polycystic ovary syndrome, have been observed as hereditary in certain cases. One potential cause of polycystic ovary syndrome is maternal hyperandrogenism, where the hormonal irregularities of the mother can affect the development of the child during gestation, resulting in the passing of polycystic ovary syndrome from mother to child.[32]
Diagnosis
Female patients may show symptoms of hyperandrogenism in their early life, but physicians become more concerned when the patient is in her late teens or older.[9]
Hyperandrogenism is most often diagnosed by checking for signs of hirsutism according to a standardized method that scores the range of excess hair growth.[8][9]
Checking medical history and a physical examination of symptoms are used for an initial diagnosis.[9] Patient history assessed includes age at thelarche, adrenarche, and menarche; patterns of menstruation; obesity; reproductive history; and the start and advancement of hyperandrogenism symptoms.[9] Patterns of menstruation are examined since irregular patterns may appear with hirsutism.[8] Family history is also assessed for occurrences of hyperandrogenism symptoms or obesity in other family members.[9]
A laboratory test can also be done on the patient to evaluate levels of FSH, LH, DHEAS, prolactin, 17OHP, and total and free testosterone in the patient's blood.[9] Abnormally high levels of any of these hormones help in diagnosing hyperandrogenism.[9]
Prevention
Since risk factors are not known and vary among individuals with hyperandrogenism, there is no sure method to prevent this medical condition.[33] Therefore, more longterm studies are needed first to find a cause for the condition before being able to find a sufficient method of prevention.[33]
However, there are a few things that can help avoid long-term medical issues related to hyperandrogenism like PCOS. Getting checked by a medical professional for hyperandrogenism; especially if one has a family history of the condition, irregular periods, or diabetes; can be beneficial.[34] Watching your weight and diet is also important in decreasing your chances, especially in obese females, since continued exercise and maintaining a healthy diet leads to an improved menstrual cycle as well as to decreased insulin levels and androgen concentrations.[33]
Treatment
Treatment of hyperandrogenism varies with the underlying condition that causes it. As a hormonal symptom of polycystic ovary syndrome, menopause, and other endocrine disorders, it is primarily treated as a symptom of these disorders. Systemically, it is treated with antiandrogens such as cyproterone acetate, flutamide and spironolactone to control the androgen levels in the patient's body. For Hyperandrogenism caused by Late-Onset Congenital Adrenal Hyperplasia (CAH), treatment is primarily focused on providing the patient with Glucocorticoids to combat the low cortisol production and the corresponding increase in androgens caused by the swelling of the Adrenal Glands.[35][36] Oestrogen-based oral contraceptives are used to treat both CAH and PCOS caused hyperandrogenism. These hormonal treatments have been found to reduce the androgen excess and suppress adrenal androgen production and cause a significant decrease in hirsutism.[37][38]
Hyperandrogenism is often managed symptomatically. Hirsutism and acne both respond well to the hormonal treatments described above, with 60-100% reporting an improvement in hirsutism.[37] Androgenic alopecia however, does not show a significant improvement with hormonal treatments and requires other treatments, such as hair transplantation.[39]
Society and culture
Because androgen excess is manifested in noticeable physical features (ex. hirsutism), a certain social stigma is associated with it. In the athletic world, multiple cases of female athletes being banned for their testosterone levels being too high have been recorded. Such social and cultural redefinitions of hyperandrogenism are important to consider outside of the clinical usage.
Sports

Following the case of South African athlete Caster Semenya, the International Association of Athletics Federations (IAAF) introduced a now suspended policy to exclude women athletes from competing as women if they have hyperandrogenism, on the ground that the condition could confer an unfair advantage.[40][41] The rules state that women may compete in the male category if their performance qualifies.[42] The IAAF states that testosterone is linked to lean body mass (LBM), so it influences athletes' strength, speed and power.[43]
The permissible testosterone limit was set at 10 nmol/L, based on a study of women competing in the World Championships in 2011 and 2013.[44] 99% of the female athletes at those competitions had testosterone levels below 3.08 nmol/L.[44] However, a study of endocrine profiles in 693 elite female and male athletes published in 2014 found that only 13.7% of the elite female athletes had high levels of testosterone while as many as 16.5% of the elite male athletes had low levels of testosterone.[45] The authors noted that there is "complete overlap of the range of concentrations seen [between the genders]. This shows that the recent decision of the IOC and IAAF to limit participation in elite events to women with a ‘normal’ serum testosterone is unsustainable."
The test has been controversial, with suggestions that it is discriminatory.[46] There is evidence that women from developing countries have been subjected to partial clitoridectomies and gonadectomies following test results revealing hyperandrogenism.[47] In September 2014, Dutee Chand, a sprinter from India who was barred by the IAAF from competing against other female runners, sought to appeal the ruling and asked for reinstatement.[48] In July 2015, the Court of Arbitration for Sport suspended the IAAF ban, thus reinstating Chand's right to compete. The IAAF was given two years in which to file scientific evidence justifying the ban. In the absence of evidence, the ban will be declared void.[49][50][51]
The suspension of the IAAF test for hyperandrogenism led to controversy in the Rio 2016 Olympic Games,[52] in particular related to the participation and performance of South African middle distance runner Caster Semenya. Competitors Lynsey Sharp and Joanna Jóźwik spoke out about their belief that Semenya has a competitive advantage, Jóźwik (who finished fifth) reportedly claimed that she was the "first European" and "second white" to finish the race, putting into doubt not just Semenya's gold medal result but also that of the (also African) silver and bronze medallist, who were not known at the time to have hyperandrogenism although silver medalist Francine Niyonsaba later confirmed her hyperandrogenism in a 2019 interview. [53] [54] Many bioethicists and gender equality advocates argue that preventing women with higher levels of testosterone from participating is a form of discrimination, penalizing the athlete for a natural trait of her body, much akin to the natural advantage possessed by taller basketball players or marathoners who train at higher altitudes.[52][55]
Social definition
Cultural variation can define hyperandrogenism socially—aside from clinical and chemical definitions—to make some hair growth unacceptable even if it is considered clinically normal based on metrics like the Ferriman-Gallwey score. For example, only pubic and axillary hair in North American women is tolerated, while other androgen-dependent hair such as growth on the upper lip, over the linea alba, over the thighs, and any periareolar hair is not.[56]
Organizations
Professional organizations like the Androgen Excess and PCOS Society exist to promote the research, treatment, diagnosis, and prevention of such disorders along with educating the public and scientific community about them.[57]
See also
References
- 1 2 3 4 5 6 7 8 9 Peigné, M; Villers-Capelle, A; Robin, G; Dewailly, D (November 2013). "[Hyperandrogenism in women]". Presse Médicale. 42 (11): 1487–99. doi:10.1016/j.lpm.2013.07.016. PMID 24184282.
- 1 2 3 4 Curtis, Michele; Antoniewicz, Leah; Linares, Silvia T. (2014). Glass' Office Gynecology. Lippincott Williams & Wilkins. p. 39. ISBN 9781608318209. Archived from the original on 28 August 2021. Retrieved 6 May 2019.
- 1 2 3 Catteau-Jonard, S; Cortet-Rudelli, C; Richard-Proust, C; Dewailly, D (2012). "Hyperandrogenism in adolescent girls". Endocrine Development. 22: 181–93. doi:10.1159/000326688. ISBN 978-3-8055-9336-6. PMID 22846529.
- 1 2 3 4 5 6 7 Carlson, Karen J.; Eisenstat, Stephanie A. (2004). The New Harvard Guide to Women's Health. Harvard University Press. p. 286. ISBN 9780674012820.
- ↑ Banker, Manish (2019). Nova IVI Textbook of Infertility & Assisted Reproductive Technology. JP Medical Ltd. p. 237. ISBN 9789388958844. Archived from the original on 28 August 2021. Retrieved 6 May 2019.
- ↑ Pathobiology of Human Disease: A Dynamic Encyclopedia of Disease Mechanisms. Elsevier. 2014. p. 1385. ISBN 9780123864574. Archived from the original on 28 August 2021. Retrieved 6 May 2019.
- 1 2 Burki, TK (October 2016). "Hyperandrogenism rule no longer in play at Rio Olympics". The Lancet. Diabetes & Endocrinology. 4 (10): 820. doi:10.1016/S2213-8587(16)30213-3. PMID 27503334.
- 1 2 3 Yildiz, Bulent O. (June 2006). "Diagnosis of hyperandrogenism: clinical criteria". Best Practice & Research Clinical Endocrinology & Metabolism. 20 (2): 167–176. doi:10.1016/j.beem.2006.02.004. ISSN 1521-690X. PMID 16772149.
- 1 2 3 4 5 6 7 8 9 Goodman, Neil (March 2001). American association of clinical endocrinologists medical guidelines for clinical practice for the diagnosis and treatment of hyperandrogenic disorders. p. 121.
- ↑ Simon, James (22 June 2015). "Androgen". Health Women. National Women's Health Resource Center. Archived from the original on 15 November 2016. Retrieved 14 November 2016.
- ↑ Brettenthaler, Nora; De Geyter, Christian; R. Huber, Peter; Keller, Ulrich (21 April 2004). "Effect of the Insulin Sensitizer Pioglitazone on Insulin Resistance, Hyperandrogenism, and Ovulatory Dysfunction in Women with Polycystic Ovary Syndrome". The Journal of Clinical Endocrinology & Metabolism (published 28 April 2011). 89 (8): 3835–3840. doi:10.1210/jc.2003-031737. PMID 15292314.
- ↑ G. Pope Jr., Harrison; M. Kouri, Elena; I.Hudson, James (5 March 1999). "Effects of Supraphysiologic Doses of Testosterone on Mood and Aggression in Normal Men". Archives of General Psychiatry. 57 (2): 133–40, discussion 155–6. doi:10.1001/archpsyc.57.2.133. PMID 10665615.
- 1 2 Franks, Stephen. "Polycystic Ovary Syndrome — NEJM." New England Journal of Medicine. N Engl J Med, 28 September 1995. Web. 14 November 2016.
- ↑ "Polycystic Ovary Syndrome (PCOS)." Causes. Mayo Clinic, n.d. Web. 9 November 2016.
- ↑ "Defining PCOS." - The University of Chicago Medicine. The University of Chicago Medical Center, n.d. Web. 10 November 2016.
- ↑ Hammond GL, Bocchinfuso WP (1996). "Sex hormone-binding globulin: gene organization and structure/function analyses". Hormone Research. 45 (3–5): 197–201. doi:10.1159/000184787. PMID 8964583.
- ↑ Burd, Irina, David Zieve, and Isla Ogilvie. "Polycystic Ovary Syndrome: MedlinePlus Medical Encyclopedia." Polycystic Ovary Syndrome: MedlinePlus Medical Encyclopedia. A.D.A.M Inc., n.d. Web. 9 November 2016.
- ↑ Pasquali, Renato (April 2011). "Research in Polycystic Ovary Syndrome Today and Tomorrow". Medscape. Blackwell Publishing. Archived from the original on 2 January 2017. Retrieved 14 November 2016.
- 1 2 Atmaca, Murat (16 December 2014). "An Interesting Cause of Hyperandrogenemic Hirsutism". Case Reports in Endocrinology. 2014: 987272. doi:10.1155/2014/987272. PMC 4280803. PMID 25580312.
- ↑ Barbieri; Hornstein MD (1988). "Hyperinsulinemia and Ovarian Hyperandrogenism. Cause and Effect". Endocrinology and Metabolism Clinics of North America. 17 (4): 685–703. doi:10.1016/S0889-8529(18)30405-5. PMID 3058472.
- ↑ James, William; Berger, Timothy; Elston, Dirk (2005). Andrews' Diseases of the Skin: Clinical Dermatology. (10th ed.). Saunders.
- ↑ Somani N, Harrison S, Bergfeld WF (2008). "The clinical evaluation of hirsutism". Dermatol Ther. 21 (5): 376–91. doi:10.1111/j.1529-8019.2008.00219.x. PMID 18844715.
- ↑ "Cushing's Syndrome". National Institute of Diabetes and Digestive and Kidney Diseases. April 2012. Archived from the original on 4 October 2016. Retrieved 14 November 2016.
- ↑ Wilson, Thomas (23 June 2016). "Congenital Adrenal Hyperplasia". Medscape. Archived from the original on 15 November 2016. Retrieved 14 November 2016.
- ↑ "Adrenocortical Carcinoma." National Cancer Institute. N.p., n.d. Web. 10 November 2016.
- ↑ "Adenoma of the Adrenal Gland | Genetic and Rare Diseases Information Center(GARD) – an NCATS Program." U.S National Library of Medicine. U.S. National Library of Medicine, n.d. Web. 10 November 2016.
- ↑ Martin, Elizabeth. Arrhenoblastoma N. Arrhenoblastoma. n.p.: Oxford University Press, 2015. Oxford Reference. Web. 10 November 2016
- ↑ Martin, Elizabeth. "hilar cell tumour." Concise Medical Dictionary. : Oxford University Press, 2015. Oxford Reference. 2015. Date Accessed 10 November 2016
- ↑ Uyeturk, Ummugul, Serife Hulya Arslan, Oznur Bal, Ulku Yalcintas Arslan, and Omur Berna Cakmak Oksuzoglu. "Isolated Ovarian Metastasis of Gastric Cancer: Krukenberg Tumor." Contemporary Oncology. Termedia Publishing House, 19 December 2013. Web. 10 November 2016.
- ↑ "R. H. Fogle, F. Z. Stanczyk, X. Zhang, and R. J. Paulson, "Ovarian androgen production in postmenopausal women"". Journal of Clinical Endocrinology and Metabolism. 92 (8, pp. 3040– 3043, 2007).
- ↑ Neraud, Barbara; Dewailly, Didier. Contemporary Endocrinology: Androgen Excess Disorders in Women: Polycystic Ovary Syndrome and Other Disorders, Second Edition. Edited by: R. Azziz et al. © Humana Press Inc., Totowa, NJ.
- ↑ Puttabyatappa, Muraly; Cardoso, Rodolfo C.; Padmanabhan, Vasantha (5 November 2016). "Puttabyatappa Muraly, Cardoso Rodolfo C., Padmanabhan Vasantha. In Special issue: Impact of maternal metabolism on newborn health". Molecular and Cellular Endocrinology. 435: 29–39. doi:10.1016/j.mce.2015.11.030. PMC 4884168. PMID 26639019.
- 1 2 3 Apter D (1998). "How Possible Is The Prevention Of Polycystic Ovary Syndrome Development In Adolescent Patients With Early Onset Of Hyperandrogenism". Journal of Endocrinological Investigation. 21 (9): 613–617. doi:10.1007/bf03350786. PMID 9856415.
- ↑ Nader S (2013). "Hyperandrogenism during puberty in the development of polycystic ovary syndrome". Fertility and Sterility (Review). 100 (1): 39–42. doi:10.1016/j.fertnstert.2013.03.013. PMID 23642453.
- ↑ Hughes I. A. (1988). "Management of Congenital Adrenal Hyperplasia". Archives of Disease in Childhood. 63 (11): 1399–1404. doi:10.1136/adc.63.11.1399. PMC 1779155. PMID 3060026.
- ↑ Merke D., Bornstein S. R. (2005). "Congenital adrenal hyperplasia". Lancet. 365 (9477): 2125–2136. doi:10.1016/S0140-6736(05)66736-0. PMID 15964450.
- 1 2 Burkman R.T. Jr (1995). "The Role of Oral Contraceptives in the Treatment of Hyperandrogenic Disorders". Am J Med. 98 (1A): 130S–136S. doi:10.1016/s0002-9343(99)80071-0. PMID 7825633.
- ↑ George Mastorakos; Carolina Koliopoulos; George Creatsas (2002). "Androgen and lipid profiles in adolescents with polycystic ovary syndrome who were treated with two forms of combined oral contraceptives". Fertility and Sterility. 77 (5): 919–927. doi:10.1016/s0015-0282(02)02993-x. PMID 12009344.
- ↑ Sinclair R, Wewerinke M, Jolley D (March 2005). "Treatment of female pattern hair loss with oral antiandrogens". Br J Dermatol. 152 (3): 466–73. doi:10.1111/j.1365-2133.2005.06218.x. PMID 15787815.
- ↑ "STANDARD OPERATIVE PROCEDURE to identify Circumstances (Female Hyperandrogenism) in Which A Particular Sports Person will not be eligible to participate in Competitions in the Female Category". Archived from the original on 4 March 2016. Retrieved 4 April 2013.
- ↑ "Archive copy" (PDF). Archived (PDF) from the original on 4 March 2016. Retrieved 4 April 2013.
{{cite web}}: CS1 maint: archived copy as title (link) - ↑ International Olympic Committee (November 2015), IOC Consensus Meeting on Sex Reassignment and Hyperandrogenism (PDF), archived (PDF) from the original on 7 February 2016, retrieved 14 November 2016
- ↑ "The biggest issue in women's sports is about to come to a head". Mother Jones. Archived from the original on 18 March 2018. Retrieved 12 November 2016.
- 1 2 "Hyperandrogenism and women vs women vs men in sport: A Q&A with Joanna Harper". 23 May 2016. Archived from the original on 17 August 2016. Retrieved 18 August 2016.
- ↑ Healy, M. L.; Gibney, J.; Pentecost, C.; Wheeler, M. J.; Sonksen, P. H. (August 2014). "Endocrine profiles in 693 elite athletes in the postcompetition setting". Clinical Endocrinology. 81 (2): 294–305. doi:10.1111/cen.12445. ISSN 0300-0664. PMID 24593684.
- ↑ Padawer, Ruth (28 June 2016). "The Humiliating Practice of Sex-Testing Female Athletes". The New York Times. ISSN 0362-4331. Archived from the original on 28 June 2016. Retrieved 28 June 2016.
- ↑ Jordan-Young, R. M.; Sonksen, P. H.; Karkazis, K. (April 2014). "Sex, health, and athletes". BMJ. 348 (apr28 9): –2926–g2926. doi:10.1136/bmj.g2926. ISSN 1756-1833. PMID 24776640. Archived from the original on 29 August 2020. Retrieved 16 December 2019.
- ↑ "Fighting for the Body She Was Born With". The New York Times. 7 October 2014. Archived from the original on 12 January 2015. Retrieved 2 March 2017.
- ↑ "Dutee Chand, Female Sprinter With High Testosterone Level, Wins Right to Compete". The New York Times. 28 July 2015. Archived from the original on 14 August 2016. Retrieved 2 March 2017.
- ↑ "Archived copy" (PDF). Archived from the original (PDF) on 16 August 2016. Retrieved 27 July 2015.
{{cite web}}: CS1 maint: archived copy as title (link) - ↑ "Dutee Chand cleared to race as IAAF suspends 'gender test' rules". BBC News Online. 27 July 2015. Archived from the original on 28 July 2015. Retrieved 27 July 2015.
- 1 2 REID, SCOTT M. "Caster Semenya's Olympic dream a topic of controversy". The Orange County Register. Archived from the original on 11 November 2016. Retrieved 10 November 2016.
- ↑ "Francine Niyonsaba of OTC Elite opens up, and good for her: Oregon track & field rundown". 17 April 2019. Archived from the original on 1 May 2019. Retrieved 1 May 2019.
- ↑ "Fifth-placed runner behind Semenya 'feels like silver medalist' and glad she was the 'second white'". The Independent. 22 August 2016. Archived from the original on 24 August 2016. Retrieved 10 November 2016.
- ↑ Longman, Jeré (18 August 2016). "Understanding the Controversy Over Caster Semenya". The New York Times. ISSN 0362-4331. Archived from the original on 11 January 2017. Retrieved 10 November 2016.
- ↑ Krishna; R, Usha (1 January 2000). "9. Hyperandrogenism in Adolescence". Adolescent Gynecology (pb). Orient Blackswan. p. 119. ISBN 9788125017936. Archived from the original on 28 August 2021. Retrieved 24 February 2019.
- ↑ wang, stephanie qian. "Androgen Excess and PCOS Society". www.ae-society.org. Archived from the original on 16 October 2016. Retrieved 10 November 2016.
External links
| Classification | |
|---|---|
| External resources |