Seborrhoeic dermatitis
| Seborrhoeic dermatitis | |
|---|---|
| Other names: Seborrhoea, sebopsoriasis, seborrhoeic eczema, pityriasis capitis[1] | |
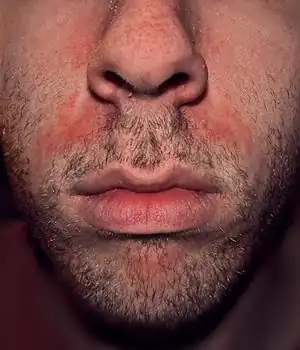 | |
| An example of seborrhoeic dermatitis between the nose and mouth | |
| Specialty | Dermatology |
| Symptoms | Itchy, flaking, greasy, red, and inflamed skin[2][3] |
| Duration | Long term[4] |
| Causes | Multiple factors[4] |
| Risk factors | Stress, winter, poor immune function, Parkinson disease[4] |
| Diagnostic method | Based on symptoms[4] |
| Differential diagnosis | Psoriasis, atopic dermatitis, tinea capitis, rosacea, systemic lupus erythematosus[4] |
| Medication | Antifungal cream, anti-inflammatory agents, coal tar, phototherapy[3] |
| Frequency | ~5% (adults),[4] ~10% (babies)[5] |
Seborrhoeic dermatitis, also known as seborrhoea, is a long-term skin disorder.[4][6] Symptoms include red, scaly, greasy, itchy, and inflamed skin.[2][3] Areas of the skin rich in oil-producing glands are often affected including the scalp, face, and chest.[4] It can result in social or self-esteem problems.[4] In babies, when the scalp is primarily involved, it is called cradle cap.[2] Dandruff is a milder form of the condition without inflammation.[7]
The cause is unclear but believed to involve a number of genetic and environmental factors.[2][4] Risk factors include poor immune function, Parkinson disease, and alcoholic pancreatitis.[4][7] The condition may worsen with stress or during the winter.[4] The Malassezia yeast is believed to play a role.[7] It is not a result of poor hygiene.[8] Diagnosis is typically based on the symptoms.[4]
The typical treatment is antifungal cream and anti-inflammatory agents.[3] Specifically, ketoconazole or ciclopirox are effective in half of people at 4 weeks.[9][10] It is unclear if other antifungals, such as miconazole, are equally effective as they have been poorly studied.[9] Other options may include salicylic acid, coal tar, benzoyl peroxide, and phototherapy.[3]
The condition is most common in the 3 first months of life in adults aged 30 to 70 years.[2] In adults between 1% and 10% of people are affected.[4] Males are more often affected than females.[4] Up to 70% of babies may be affected at some point in time.[5]
Signs and symptoms
Seborrhoeic dermatitis' symptoms appear gradually, and usually the first signs are flaky skin and scalp.[11] Symptoms occur most commonly anywhere on the skin of the scalp, behind the ears, on the face, and in areas where the skin folds. Flakes may be yellow, white or grayish.[12] Redness and flaking may also occur on the skin near the eyelashes, on the forehead, around the sides of the nose, on the chest, and on the upper back.
In more severe cases, yellowish to reddish scaly pimples appear along the hairline, behind the ears, in the ear canal, on the eyebrows, on the bridge of the nose, around the nose, on the chest, and on the upper back.[13]
Commonly, patients experience mild redness, scaly skin lesions and in some cases hair loss.[14] Other symptoms include patchy scaling or thick crusts on the scalp, red, greasy skin covered with flaky white or yellow scales, itching, soreness and yellow or white scales that may attach to the hair shaft.[15]
Seborrhoeic dermatitis can occur in infants younger than three months and it causes a thick, oily, yellowish crust around the hairline and on the scalp. Itching is not common among infants. Frequently, a stubborn diaper rash accompanies the scalp rash.[13]
.jpg.webp) Seborrhoeic dermatitis ear
Seborrhoeic dermatitis ear.jpg.webp) Seborrhoeic dermatitis chest
Seborrhoeic dermatitis chest Seborrhoeic dermatitis scalp
Seborrhoeic dermatitis scalp.jpg.webp) Seborrhoeic dermatitis around eyebrows
Seborrhoeic dermatitis around eyebrows.jpg.webp) Seborrhoeic dermatitis underarms
Seborrhoeic dermatitis underarms
Causes
The cause of seborrhoeic dermatitis has not been fully clarified.[1][16] The condition is thought to be due to a local inflammatory response to colonization by Malassezia fungi species in sebum-producing skin areas including the scalp, face, chest, back, underarms, and groin.[3][16] This is based on observations of high counts of Malassezia species in skin affected by seborrhoeic dermatitis and on the effectiveness of antifungals in treating the condition.[16] Such species of Malassezia include M. furfur (formerly P. ovale), M. globosa, M. restricta, M. sympodialis, and M. slooffiae.[3] Although Malassezia appears to be the central predisposing factor in seborrhoeic dermatitis, it is thought that other factors are necessary for the presence of Malassezia to result in the pathology characteristic of the condition.[16] This is based on the fact that high counts of Malassezia in the skin alone do not result in seborrhoeic dermatitis.[16] Besides antifungals, the effectiveness of anti-inflammatory drugs, which reduce inflammation, and antiandrogens, which reduce sebum production, provide further insights into the pathophysiology of seborrhoeic dermatitis.[3][17][18] Eunuchs, owing to their low androgen levels and small sebaceous glands, do not develop seborrheic dermatitis.[19]
In addition to the presence of Malassezia, genetic, environmental, hormonal, and immune-system factors are necessary for and/or modulate the expression of seborrhoeic dermatitis.[20][21] The condition may be aggravated by illness, psychological stress, fatigue, sleep deprivation, change of season, and reduced general health.[22] In children and babies, excessive vitamin A intake[23] or issues with Δ6-desaturase enzymes[22] have been correlated with increased risk. Seborrhoeic dermatitis-like eruptions are also associated with vitamin B6 deficiency.[24] Those with immunodeficiency (especially infection with HIV) and with neurological disorders such as Parkinson's disease (for which the condition is an autonomic sign) and stroke are particularly prone to it.[25]
Management
Medications
A variety of different types of medications are able to reduce symptoms of seborrhoeic dermatitis.[3] These include certain antifungals, anti-inflammatory agents like corticosteroids and nonsteroidal anti-inflammatory drugs, antiandrogens, and antihistamines, among others.[3][1]
Antifungals
Regular use of an over-the-counter or prescription antifungal shampoo or cream may help those with recurrent episodes. The topical antifungal medications ketoconazole and ciclopirox have the best evidence.[9] It is unclear if other antifungals are equally effective as this has not been sufficiently studied.[9] Antifungals that have been studied and found to be effective in the treatment of seborrhoeic dermatitis include ketoconazole, fluconazole, miconazole, bifonazole, sertaconazole, clotrimazole, flutrimazole, ciclopirox, terbinafine, butenafine, selenium sulfide, and lithium salts such as lithium gluconate and lithium succinate.[9][3] Topical climbazole appears to have little effectiveness in the treatment of seborrhoeic dermatitis.[9] Systemic therapy with oral antifungals including itraconazole, fluconazole, ketoconazole, and terbinafine is effective.[3]
Anti-inflammatory treatments
Topical corticosteroids have been shown to be effective in short-term treatment of serborrhoeic dermatitis, and are as effective or more effective than antifungal treatment with azoles. There is also evidence for the effectiveness of calcineurin inhibitors like tacrolimus and pimecrolimus as well as lithium salt therapy.[26]
Oral immunosuppressive treatment, such as with prednisone, has been used in short courses as a last resort in seborrhoeic dermatitis due to its potential side effects.[27]
Antiandrogens
Seborrhoea is recognized as an androgen-sensitive condition – that is, it is caused or aggravated by androgen sex hormones such as testosterone and dihydrotestosterone – and is a common symptom of hyperandrogenism (e.g., that seen in polycystic ovary syndrome).[28][29] In addition, seborrhoea, as well as acne, are commonly associated with puberty due to the steep increase of androgen levels at that time.[30]
In accordance with the involvement of androgens in seborrhoea, antiandrogens, such as cyproterone acetate,[31] spironolactone,[32] flutamide,[33][34] and nilutamide,[35][36] are highly effective in alleviating the condition.[28][37] As such, they are used in the treatment of seborrhoea,[28][37] particularly severe cases.[38] While beneficial in seborrhoea, effectiveness may vary with different antiandrogens; for instance, spironolactone (which is regarded as a relatively weak antiandrogen) has been found to produce a 50% improvement after three months of treatment, whereas flutamide has been found to result in an 80% improvement within three months.[28][34] Cyproterone acetate is similarly more potent and effective than spironolactone, and results in considerable improvement or disappearance of acne and seborrhoea in 90% of patients within three months.[39]
Systemic antiandrogen therapy are generally used to treat seborrhoea only in women, and not in men, as these medications can result in feminization (e.g., gynecomastia), sexual dysfunction, and infertility in males.[40][41] In addition, antiandrogens theoretically have the potential to feminize male fetuses in pregnant women, and for this reason, are usually combined with effective birth control in sexually active women who can or may become pregnant.[39]
Antihistamines
Antihistamines are used primarily to reduce itching, if present. However, research studies suggest that some antihistamines have anti-inflammatory properties.[42]
Other treatments
- Coal tar can be effective, but, although no significant increased risk of cancer in human treatment with coal tar shampoos has been found,[43] caution is advised since coal tar is carcinogenic in animals, and heavy human occupational exposures do increase cancer risks.
- Isotretinoin, a sebosuppressive agent, may be used to reduce sebaceous gland activity as a last resort in refractory disease. However, isotretinoin has potentially serious side effects and few patients with seborrhoea are appropriate candidates for therapy.[27]
- Keratolytics like topical urea[44]
- Metronidazole[9]
Phototherapy
Another potential option is natural and artificial UV radiation since it can curb the growth of Malassezia yeast [45] Some recommend photodynamic therapy using UV-A and UV-B laser or red and blue LED light to inhibit the growth of Malassezia fungus and reduce seborrhoeic inflammation.[46][47][48]
Epidemiology
Seborrhoea affects 1 to 5% of the general population.[1][49][50] It is slightly more common in men, but affected women tend to have more severe symptoms.[50] The condition usually recurs throughout a person's lifetime.[51] Seborrhoea can occur in any age group[51] but usually starts at puberty and peaks in incidence at around 40 years of age.[52] It can reportedly affect as many as 31% of older people.[50] Severity is worse in dry climates.[51]
See also
References
- 1 2 3 4 Dessinioti, C; Katsambas, A (Jul–Aug 2013). "Seborrheic dermatitis: etiology, risk factors, and treatments: facts and controversies". Clinics in Dermatology. 31 (4): 343–51. doi:10.1016/j.clindermatol.2013.01.001. PMID 23806151.
- 1 2 3 4 5 "Seborrheic Dermatitis - Dermatologic Disorders". Merck Manuals Professional Edition. Archived from the original on 26 January 2020. Retrieved 22 November 2019.
- 1 2 3 4 5 6 7 8 9 10 11 12 Borda, LJ; Perper, M; Keri, JE (March 2019). "Treatment of seborrheic dermatitis: a comprehensive review". The Journal of Dermatological Treatment. 30 (2): 158–169. doi:10.1080/09546634.2018.1473554. PMID 29737895.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 Ijaz, N; Fitzgerald, D (2 June 2017). "Seborrhoeic dermatitis". British Journal of Hospital Medicine. 78 (6): C88–C91. doi:10.12968/hmed.2017.78.6.C88. PMID 28614013.
- 1 2 Nobles, T; Krishnamurthy, K (January 2019). "Cradle Cap". PMID 30285358.
{{cite journal}}: Cite journal requires|journal=(help) - ↑ Lim, Henry W. (2020). "409. Eczemas, photodermatoses, papulomatoses, papulosquamous (including fungal) diseases, and figurate erythema:Seborrhoeic dermatitis". In Goldman, Lee; Schafer, Andrew I. (eds.). Goldman-Cecil Medicine. Vol. 2 (26th ed.). Philadelphia: Elsevier. p. 2613. ISBN 978-0-323-53266-2. Archived from the original on 2023-04-28. Retrieved 2023-04-28.
- 1 2 3 Naldi, L; Diphoorn, J (27 May 2015). "Seborrhoeic dermatitis of the scalp". BMJ Clinical Evidence. 2015. PMC 4445675. PMID 26016669.
- ↑ "Seborrheic dermatitis". American Academy of Dermatology. Archived from the original on 21 October 2017. Retrieved 20 October 2017.
- 1 2 3 4 5 6 7 Okokon, EO; Verbeek, JH; Ruotsalainen, JH; Ojo, OA; Bakhoya, VN (28 April 2015). "Topical antifungals for seborrhoeic dermatitis". The Cochrane Database of Systematic Reviews. 4 (5): CD008138. doi:10.1002/14651858.CD008138.pub3. PMC 4448221. PMID 25933684.
- ↑ Moe, Samantha (30 October 2023). "#351 Flaked out? Topical treatment for seborrheic dermatitis (Free)". CFPCLearn. Archived from the original on 31 October 2023. Retrieved 31 October 2023.
- ↑ "Dermatitis Seborrheic Treatment". Archived from the original on 2010-06-02. Retrieved June 11, 2010.
- ↑ "Seborrheic Dermatitis". Archived from the original on June 15, 2010. Retrieved June 11, 2010.
- 1 2 "Dermatitis". Archived from the original on September 25, 2011. Retrieved June 11, 2010.
- ↑ "What is Seborrheic Dermatitis?". Archived from the original on April 20, 2010. Retrieved June 11, 2010.
- ↑ "Symptoms". Archived from the original on May 26, 2010. Retrieved June 11, 2010.
- 1 2 3 4 5 Wikramanayake TC, Borda LJ, Miteva M, Paus R (September 2019). "Seborrheic dermatitis-Looking beyond Malassezia". Exp. Dermatol. 28 (9): 991–1001. doi:10.1111/exd.14006. PMID 31310695.
- ↑ Trivedi, M.K.; Shinkai, K.; Murase, J.E. (2017). "A Review of hormone-based therapies to treat adult acne vulgaris in women". International Journal of Women's Dermatology. 3 (1): 44–52. doi:10.1016/j.ijwd.2017.02.018. ISSN 2352-6475. PMC 5419026. PMID 28492054.
- ↑ Paradisi, Roberto; Fabbri, Raffaella; Porcu, Eleonora; Battaglia, Cesare; Seracchioli, Renato; Venturoli, Stefano (2010). "Retrospective, observational study on the effects and tolerability of flutamide in a large population of patients with acne and seborrhea over a 15-year period". Gynecological Endocrinology. 27 (10): 823–829. doi:10.3109/09513590.2010.526664. ISSN 0951-3590. PMID 21117864.
- ↑ Orfanos, C. E.; Frost, Ph. (1990). "Seborrhoeic Dermatitis, Scalp Psoriasis and Hair". Hair and Hair Diseases. pp. 641–661. doi:10.1007/978-3-642-74612-3_25. ISBN 978-3-642-74614-7.
- ↑ Johnson, Betty Anne; Nunley, Julia R. (May 2000). "Treatment of seborrheic dermatitis". American Family Physician. 61 (9): 2703–10, 2713–4. PMID 10821151. Archived from the original on 2010-07-06.
- ↑ Janniger CK, Schwartz RA (July 1995). "Seborrheic dermatitis". American Family Physician. 52 (1): 149–55, 159–60. PMID 7604759.
- 1 2 Schwartz, Robert A.; Janusz, Christopher A.; Janniger, Camila K. (July 2006). "Seborrheic dermatitis: an overview". American Family Physician. 74 (1): 125–30. PMID 16848386. Archived from the original on 2020-01-26. Retrieved 2010-04-15.
- ↑ MedlinePlus Encyclopedia: Hypervitaminosis A
- ↑ Alamgir, A.N.M. (2018). Therapeutic Use of Medicinal Plants and their Extracts: Volume 2: Phytochemistry and Bioactive Compounds. Springer. p. 435. ISBN 978-3319923871.
- ↑ "Seborrhoeic dermatitis and dandruff (seborrheic eczema). DermNet NZ". . DermNet NZ. 2012-03-20. Archived from the original on 2012-06-15. Retrieved 2012-06-10.
- ↑ Kastarinen, Helena; Oksanen, Tuija; Okokon, Enembe O; Kiviniemi, Vesa V; Airola, Kristiina; Jyrkkä, Johanna; Oravilahti, Tuomas; Rannanheimo, Piia K; Verbeek, Jos H (2014-05-19). "Topical anti-inflammatory agents for seborrhoeic dermatitis of the face or scalp". Cochrane Database of Systematic Reviews (5): CD009446. doi:10.1002/14651858.CD009446.pub2. ISSN 1465-1858. PMC 6483543. PMID 24838779. Archived from the original on 2018-06-30. Retrieved 2018-06-30.
- 1 2 Gupta, AK; Richardson, M; Paquet, M (January 2014). "Systematic review of oral treatments for seborrheic dermatitis". Journal of the European Academy of Dermatology and Venereology : JEADV. 28 (1): 16–26. doi:10.1111/jdv.12197. PMID 23802806.
- 1 2 3 4 Singh, Shankar; Gauthier, Sylvain; Labrie, Fernand (2000). "Androgen Receptor Antagonists (Antiandrogens) Structure-Activity Relationships". Current Medicinal Chemistry. 7 (2): 211–247. doi:10.2174/0929867003375371. ISSN 0929-8673. PMID 10637363.
- ↑ Zouboulis, Christos C.; Degitz, Klaus (2004). "Androgen action on human skin – from basic research to clinical significance". Experimental Dermatology. 13 (s4): 5–10. doi:10.1111/j.1600-0625.2004.00255.x. ISSN 0906-6705. PMID 15507105.
- ↑ De Groot LJ, Beck-Peccoz P, Chrousos G, Dungan K, Grossman A, Hershman JM, Koch C, McLachlan R, New M, Rebar R, Singer F, Vinik A, Weickert MO, Handelsman DJ (2000). "Androgen Physiology, Pharmacology and Abuse". PMID 25905231.
{{cite journal}}: Cite journal requires|journal=(help) - ↑ Kenneth L. Becker (2001). Principles and Practice of Endocrinology and Metabolism. Lippincott Williams & Wilkins. pp. 1004–. ISBN 978-0-7817-1750-2. Archived from the original on 2013-06-02.
- ↑ G. Plewig; A.M. Kligman (6 December 2012). ACNE and ROSACEA. Springer Science & Business Media. pp. 66, 685, 687. ISBN 978-3-642-59715-2. Archived from the original on 19 March 2017.
- ↑ NADIR R. FARID; Evanthia Diamanti-Kandarakis (27 February 2009). Diagnosis and Management of Polycystic Ovary Syndrome. Springer Science & Business Media. pp. 240–. ISBN 978-0-387-09718-3. Archived from the original on 19 March 2017.
- 1 2 Bentham Science Publishers (September 1999). Current Pharmaceutical Design. Bentham Science Publishers. pp. 717–. Archived from the original on 2020-07-27. Retrieved 2016-10-06.
- ↑ Couzinet B, Thomas G, Thalabard JC, Brailly S, Schaison G (1989). "Effects of a pure antiandrogen on gonadotropin secretion in normal women and in polycystic ovarian disease". Fertil. Steril. 52 (1): 42–50. doi:10.1016/s0015-0282(16)60786-0. PMID 2744186.
- ↑ Namer M (1988). "Clinical applications of antiandrogens". J. Steroid Biochem. 31 (4B): 719–29. doi:10.1016/0022-4731(88)90023-4. PMID 2462132.
- 1 2 Mutschler; Hartmut Derendorf (1995). Drug Actions: Basic Principles and Theraputic Aspects. CRC Press. pp. 304–. ISBN 978-0-8493-7774-7. Archived from the original on 2017-11-05.
- ↑ Joseph T. DiPiro; Robert L. Talbert; Gary C. Yee; Gary R. Matzke; Barbara G. Wells; L. Michael Posey (6 July 2008). Pharmacotherapy: A Pathophysiologic Approach. McGraw Hill Professional. p. 1598. ISBN 978-0-07-164325-2. Archived from the original on 19 March 2017.
- 1 2 A. Hughes; S. H. Hasan; G. W. Oertel; H. E. Voss; F. Bahner; F. Neumann; H. Steinbeck; K.-J. Gräf; J. Brotherton; H. J. Horn; R. K. Wagner (27 November 2013). Androgens II and Antiandrogens / Androgene II und Antiandrogene. Springer Science & Business Media. pp. 351, 516. ISBN 978-3-642-80859-3. Archived from the original on 19 March 2017.
- ↑ Larry E. Millikan (19 April 2016). Drug Therapy in Dermatology. CRC Press. pp. 295–. ISBN 978-0-203-90831-0. Archived from the original on 29 July 2017.
- ↑ Sara Brenner (13 December 2013). The Clinical Nanomedicine Handbook. CRC Press. pp. 97–. ISBN 978-1-4398-3478-7. Archived from the original on 5 November 2017.
- ↑ Grob, JJ; Castelain, M.; Richard, MA; Bonniol, JP; Beraud, V.; Adhoute, H.; Guillou, N.; Bonerandi, JJ (1998). "Antiinflammatory properties of cetirizine in a human contact dermatitis model. Clinical evaluation of patch tests is not hampered by antihistamines". Acta Dermato-Venereologica. 78 (3): 194–7. doi:10.1080/000155598441512. PMID 9602225.
- ↑ Roelofzen JH, Aben KK, Oldenhof UT, et al. (April 2010). "No increased risk of cancer after coal tar treatment in patients with psoriasis or eczema" (PDF). J. Invest. Dermatol. 130 (4): 953–61. doi:10.1038/jid.2009.389. PMID 20016499. Archived (PDF) from the original on 2020-07-28. Retrieved 2020-03-27.
- ↑ Piquero-Casals J, Hexsel D, Mir-Bonafé JF, Rozas-Muñoz E (September 2019). "Topical Non-Pharmacological Treatment for Facial Seborrheic Dermatitis". Dermatol Ther (Heidelb). 9 (3): 469–477. doi:10.1007/s13555-019-00319-0. PMC 6704200. PMID 31396944.
- ↑ Wikler, JR.; Janssen N.; Bruynzeel DP.; Nieboer C. (1990). "The effect of UV-light on pityrosporum yeasts: ultrastructural changes and inhibition of growth". Acta Dermato-venereologica. Stockholm. 70 (1): 69–71. PMID 1967880.
- ↑ Wikler JR, Janssen N, Bruynzeel DP, Nieboer C (1990). "The effect of UV-light on pityrosporum yeasts: ultrastructural changes and inhibition of growth". Acta Dermato-venereologica. 70 (1): 69–71. PMID 1967880.
- ↑ Calzavara-Pinton PG, Venturini M, Sala R (2005). "A comprehensive overview of photodynamic therapy in the treatment of superficial fungal infections of the skin". Photochem Photobiol. 78 (1): 1–6. doi:10.1016/j.jphotobiol.2004.06.006. PMID 15629243.
- ↑ Abels, Christoph; Jori, Giulio; Szeimies, Rolf-Markus; Maisch, Tim (2004-10-11). "Antibacterial photodynamic therapy in dermatology – Photochemical & Photobiological Sciences (RSC Publishing)". Photochemical & Photobiological Sciences. rsc.org. 3 (10): 907–917. doi:10.1039/B407622B. PMID 15480480.
- ↑ Mark A. Goldstein; Myrna Chandler Goldstein; Larry P. Credit (17 March 2009). Your Best Medicine: From Conventional and Complementary Medicine--Expert-Endorsed Therapeutic Solutions to Relieve Symptoms and Speed Healing. Rodale. pp. 462–. ISBN 978-1-60529-656-2. Archived from the original on 5 November 2017.
- 1 2 3 Miranda A. Farage; Kenneth W. Miller; Howard I. Maibach (2 December 2009). Textbook of Aging Skin. Springer Science & Business Media. pp. 534–. ISBN 978-3-540-89655-5. Archived from the original on 5 November 2017.
- 1 2 3 Jeanette Jacknin (2001). Smart Medicine for Your Skin: A Comprehensive Guide to Understanding Conventional and Alternative Therapies to Heal Common Skin Problems. Penguin. pp. 271–. ISBN 978-1-58333-098-2. Archived from the original on 2017-11-05.
- ↑ Ooi ET, Tidman MJ (2014). "Improving the management of seborrhoeic dermatitis". Practitioner. 258 (1768): 23–6, 3. PMID 24689165.
External links
| Classification | |
|---|---|
| External resources |
- American Academy of Dermatology: Seborrheic dermatitis Archived 2017-10-21 at the Wayback Machine