Moyamoya disease
| Moyamoya disease | |
|---|---|
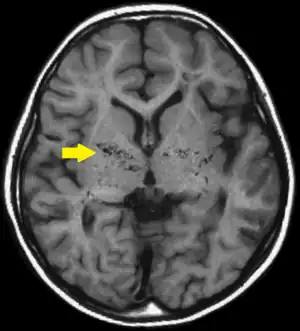 | |
| T1-weighted MR image of moyamoya disease. Flow void in the basal ganglia is indicated by the arrow. | |
| Specialty | Neurosurgery |
Moyamoya disease is a disease in which certain arteries in the brain are constricted. Blood flow is blocked by constriction and blood clots (thrombosis).[1] A collateral circulation develops around the blocked vessels to compensate for the blockage, but the collateral vessels are small, weak, and prone to bleeding, aneurysm and thrombosis. On conventional angiography, these collateral vessels have the appearance of a "puff of smoke" (described as "もやもや (moyamoya)" in Japanese).[1]
When moyamoya is diagnosed by itself, with no underlying correlational conditions, it is diagnosed as moyamoya disease. This is also the case when the arterial constriction and collateral circulation are bilateral. Moyamoya syndrome is unilateral arterial constriction, or occurs when one of the several specified conditions is also present.[2] This may also be considered as moyamoya being secondary to the primary condition. Mainly, occlusion of the distal internal carotid artery occurs. On angiography, a "puff of smoke" appearance is seen, and the treatment of choice is surgical bypass.
Signs and symptoms
Patients usually present with TIA, ischemic/hemorrhagic stroke, or seizure.[3] The age distribution is bimodal being either young adolescence or mid-forties.[4]
Cause
About 10% of cases of moyamoya disease are familial, and some cases result from specific genetic mutations. Susceptibility to moyamoya disease-2 (MYMY2; 607151) is caused by variation in the RNF213 gene (613768) on the long arm of chromosome 17 (17q25). Moyamoya disease-5 (MYMY5; 614042) is caused by mutation in the ACTA2 gene (102620) on the long arm of chromosome 10 (10q23.3); and moyamoya disease-6 with achalasia (MYMY6; 615750) is caused by mutation in the GUCY1A3 gene (139396) on the long arm of chromosome 4 (4q32). Loci for the disorder have been mapped to the short arm of chromosome 3 (MYMY1) and the long arm of chromosome 8 (8q23) (MYMY3; 608796). See also MYMY4 (300845), an X-linked recessive syndromic disorder characterized by moyamoya disease, short stature, hypergonadotropic hypogonadism, and facial dysmorphism, and linked to q25.3, on chromosome 17.[5]
In Japan the overall incidence is higher (0.35 per 100,000).[6] In North America, women in the third or fourth decade of life are most often affected, but the condition may also occur during infancy or childhood. These women frequently experience transient ischaemic attacks (TIA), cerebral hemorrhage, or may not experience any symptoms at all. They have a higher risk of recurrent stroke and may be experiencing a distinct underlying pathophysiology compared to patients from Japan.[7]
Moyamoya disease can be either congenital or acquired. Patients with Down syndrome, sickle cell anemia, neurofibromatosis type 1, congenital heart disease, fibromuscular dysplasia, activated protein C resistance, or head trauma can develop moyamoya malformations.[8] It is more common in women than in men, although about a third of those affected are male.[9]
Pathophysiology
The disease moyamoya, which is a Japanese mimetic word, gets its characteristic name due to the appearance of smoke on relevant angiographs resultant from the tangle of tiny vessels in response to stenosis. This makes the blood leak out of the arteries, causing pressure to the brain and subsequent headaches. Over the last six decades since the disease was first described, pathogenesis of moyamoya disease remained elusive, although the gene ring finger protein 213 (RNF213) has been implicated.[10] In September 2021, a south Indian researcher has proposed a pathbreaking theory on moyamoya pathogenesis. Coined the "Mechano-biological theory", the disease has a multifactorial pathogenesis. The authors provide a tangible explanation of the occurrence of moyamoya phenomenon in the idiopathic and syndromic variants of the disease.[11] In short, the authors report that Moyamoya disease likely occurs due to a number of factors (ex. differences in vascular anatomy) that ultimately contribute to broad cerebral blood vessel occlusion and consequent shifts in vessel connections to try to provide blood for the compromised brain.[12]
Once it begins, the vascular occlusion tends to continue despite any known medical management. In some people this leads to transient ischemic attacks or repeated strokes with severe functional impairment or even death. In others, the blockage may not cause any symptoms.[13]
The disease causes constrictions primarily in the internal carotid artery, and often extends to the middle and anterior cerebral arteries, branches of the internal carotid artery inside the skull.[1] When the internal carotid artery becomes completely blocked, the fine collateral circulation that it supplies is obliterated. Patients often survive on the collateral circulation from the back (posterior) of the circle of Willis, arising from the basilar artery.[1]
The arterial constrictions in moyamoya disease are unlike the constrictions in atherosclerosis. In atherosclerosis, the walls of arteries are damaged, leading to the deposition of fat and immune cells, and ultimately the accumulation of immune cells laden with fat. In moyamoya, the inner layer of the carotid artery proliferates within the arterial lumen. The artery also fills with blood clots, which may cause strokes.[1]
Moyamoya disease tends to affect adults in the third to fourth decade of life. In children it tends to cause strokes or seizures. In adults it tends to cause strokes or bleeding. The clinical features are strokes, recurrent transient ischemic attacks (TIAs), sensorimotor paralysis (numbness and paralysis of the extremities), convulsions and/or migraine-like headaches. Moreover, following a stroke, secondary bleeding may occur. Such bleeding, called hemorrhagic strokes, may also stem from rupture of the weak neovascular vessel walls.
Diagnosis
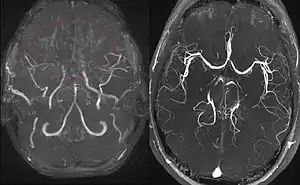
Right: healthy patient, for comparison.
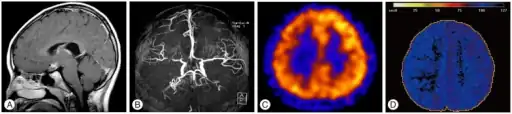
Cerebral angiography is the gold standard of diagnosing moyamoya disease and its progression. According to Suzuki's system, it can be classified into six stages:[14]
- Stage 1 Narrowing of carotid fork
- Stage 2 Initiation of the moyamoya and dilatation of intracranial main arteries
- Stage 3 Intensification of the moyamoya and defects of the anterior cerebral artery and middle cerebral artery
- Stage 4 Minimization of the moyamoya and defects of the posterior cerebral artery
- Stage 5 Reduction of the moyamoya and development of external carotid artery collaterals
- Stage 6 Disappearance of the moyamoya and circulation only via external cerebral artery and vertebral artery
Magnetic resonance angiography (MRA) is also useful in diagnosing the disease with good correlation with Suzuki's grading system.[14]
Proliferation of smooth muscle cells in the walls of the moyamoya-affected arteries has been found to be representative of the disease. A study of six autopsies of six patients who died from moyamoya disease lead to the finding that there is evidence that supports the theory that there is a thickening, or proliferation, of the innermost layer of the vessels affected by moyamoya. These vessels are the ACA (anterior cerebral artery), MCA (middle cerebral artery), and ICA (internal carotid artery). The occlusion of the ICA results in concomitant diminution of the "puff-of-smoke" collaterals, as they are supplied by the ICA.[15]
Often nuclear medicine studies such as SPECT (single photon emission computerized tomography) are used to demonstrate the decreased blood and oxygen supply to areas of the brain involved with moyamoya disease. Conventional angiography provides the conclusive diagnosis of moyamoya disease in most cases and should be performed before any surgical considerations.
Darren B. Orbach explains how the disease progresses as well as the role angiography plays in detecting the progression of moyamoya in a short video.[16] In 2019, author and artist Sarah Lippett published a graphic novel about her decade-long struggle to get a diagnosis and treatment for moyamoya disease, called A Puff of Smoke (published with Jonathan Cape). The book was praised in the newspaper The Guardian as a "wonderfully drawn memoir of a serious childhood illness."[17] It was one of the paper's "graphic novels of the year" in 2019 and The Observer newspaper's graphic novel of the month in November 2019.[18]
Associated biomarkers
Smith (2015) conducted a study that looked into specific biological markers that correlate to moyamoya disease. Some of the categories of these biomarkers include phenotypes - conditions commonly related to moyamoya, radiographical markers for the diagnosis of moyamoya, and proteins as well as cellular changes that occur in cases of moyamoya.[19]
Similar to moyamoya disease, there are conditions that are closely associated with moyamoya disease. Some of the more common medical conditions that are closely associated with moyamoya disease include trisomy 21 (Down Syndrome), sickle cell disease, and neurofibromatosis type 1. There is also evidence that identifies hyperthyroidism and congenital dwarfing syndromes as two of the more loosely associated syndromes that correlate with the possibility of being diagnosed with moyamoya disease later in life.[19]
There is also research that has shown that certain radiographic biomarkers that lead to the diagnosis of moyamoya disease have been identified. The specific radiographic markers are now considered an acceptable key component to moyamoya disease and have been added to the International Classification of Diseases (ICD). These biomarkers of moyamoya are "stenosis of the distal ICA's up to and including the bifurcation, along with segments of the proximal ACA and MCA...dilated basal collateral vessels must be present" [19] Some other common findings that have not been added to the classification index of those with moyamoya disease which are found using radiography involve very distinct changes in the vessels of the brain. These changes include newly formed vessels made to compensate for another change noted, ischemia and cerebrovascular reserve, both found on MRI. Functional changes include evidence of ischemia in vessels of the brain (ICA, ACA, MCA, specifically). It is important to also note that the radiographic biomarkers, in order to be classified as moyamoya disease, all findings must be bilateral. If this is not the case and the findings are unilateral, it is diagnosed as moyamoya syndrome.[19]
There are also several protein biomarkers that have been linked to the moyamoya disease diagnosis. Although the sample size of the studies performed are small due to the rarity of the disease, the findings are indicative of a correlation between the disease and several specific protein biomarkers.[19] Other studies have confirmed the correlation of moyamoya and adhesion molecule 1 (ICAM-1) being increased as compared to normal vascular function counterparts.[20][21] Furthermore, it has been concluded that the localization of inflammatory cells suggests that the inflammation stimulus itself may be responsible for the proliferation and occlusion in the ICA, ACA, and MCA found in those with moyamoya disease.[2]
Treatment
Drugs such as antiplatelet agents (including aspirin) are usually given to prevent clots, but surgery is usually recommended. Because moyamoya tends to affect only the internal carotid artery and nearby sections of the adjacent anterior and middle cerebral arteries, surgeons can direct other arteries, such as the external carotid artery or the superficial temporal artery to replace its circulation. The arteries are either sewn directly into the brain circulation, or placed on the surface of the brain to reestablish new circulation after a few weeks.[1]
There are many operations that have been developed for the condition, but currently the most favored are the in-direct procedures EDAS, EMS, and multiple burr holes and the direct procedure STA-MCA. Combined revascularisation procedure, which includes both the direct superficial temporal artery (STA) to middle cerebral artery (MCA) bypass performed with a combination of in-direct procedures, is considered the treatment of choice. Although its efficacy, particularly for hemorrhagic disease, remains uncertain, the procedure is thought to reduce the hemodynamic burden on the engorged collateral blood vessels. Multiple burr holes have been used in frontal and parietal lobes with good neovascularisation achieved.
The EDAS (encephaloduroarteriosynangiosis) procedure is a synangiosis procedure that requires dissection of a scalp artery over a course of several centimeters and then making a small temporary opening in the skull directly beneath the artery. The artery is then sutured to a branch of the middle cerebral artery on the surface of the brain and the bone is replaced.
In the EMS (encephalomyosynangiosis) procedure, the temporalis muscle, which is in the temple region of the forehead, is dissected and through an opening in the skull placed onto the surface of the brain.
In the multiple burr holes procedure, multiple small holes (burr holes) are placed in the skull to allow for growth of new vessels into the brain from the scalp.
In the STA-MCA procedure, the scalp artery (superficial temporal artery or STA) is directly sutured to an artery on the surface of the brain (middle cerebral artery or MCA). This procedure is also commonly referred to as an EC-IC (External Carotid-Internal Carotid) bypass.
All of these operations have in common the concept of a blood and oxygen "starved" brain reaching out to grasp and develop new and more efficient means of bringing blood to the brain and bypassing the areas of blockage. The modified direct anastomosis and encephalo-myo-arterio-synangiosis play a role in this improvement by increasing cerebral blood flow (CBF) after the operation. A significant correlation is found between the postoperative effect and the stages of preoperative angiograms. It is crucial for surgery that the anesthesiologist have experience in managing children being treated for moyamoya, as the type of anesthesia they require is very different from the standard anesthetic children get for almost any other type of neurosurgical procedure.
Prognosis
The natural history of this disorder is not well known. The long term outlook for patients with treated moyamoya seems to be good when direct bypass is used.[22] Although symptoms may seem to improve almost immediately after the in-direct EDAS, EMS, and multiple burr holes surgeries, it will take probably 6 to 12 months before new vessels can develop to give a sufficient blood supply. With the direct STA-MCA surgery, increased blood supply is immediate.
Once a major stroke or bleeding takes place, even with treatment, the patient may be left with permanent loss of function so it is very important to treat this condition promptly.
Research
Recent investigations have established that both moyamoya disease and arteriovenous fistulas (AVFs) of the lining of the brain, the dura, are associated with dural angiogenesis. These factors may represent a mechanism for ischemia contributing to the formation of dural AVFs. At least one case of simultaneous unilateral moyamoya syndrome and ipsilateral dural arteriovenous fistula has been reported at the Barrow Neurological Institute. In this case a 44-year-old man presented with headache, tinnitus, and an intraventricular hemorrhage, as seen on computed tomographic scans. Cerebral angiography showed a right moyamoya pattern and an ipsilateral dural AVF fed by branches of the external carotid artery and draining into the transverse sinus. This extremely rare coincidental presentation may have deeper pathogenic implications.[23]
The research into the pathogenesis of Moyamoya disease has found a breakthrough with the proposal of a "Mechano-biological theory" of pathogenesis of this disease. A research group in southern India have proposed this unifying theory based on computational fluid dynamics studies and longitudinal data. This proposal unifies the pathogenesis of moyamoya disease and moyamoya syndromes described in literature under a single mechanism.[11]
References
- 1 2 3 4 5 6 Scott, R. Michael; Smith, Edward R. (2009). "Moyamoya Disease and Moyamoya Syndrome". New England Journal of Medicine. 360 (12): 1226–1237. doi:10.1056/NEJMra0804622. PMID 19297575. S2CID 26151018. Archived from the original on 2022-01-11. Retrieved 2021-12-01.
- 1 2 Ganesan, Vijeya; Smith, Edward R. (2015). "Moyamoya: Defining current knowledge gaps". Developmental Medicine & Child Neurology. 57 (9): 786–787. doi:10.1111/dmcn.12708. PMID 25683905. S2CID 34816246.
- ↑ Kleinloog, R (May 2012). "Regional differences in incidence and patient characteristics of moyamoya disease: a systematic review". J Neurol Neurosurg Psychiatry. 83 (5): 531–6. doi:10.1136/jnnp-2011-301387. PMID 22378916. S2CID 207004883.
- ↑ Duan, Lian; Bao, Xiang-Yang; Yang, Wei-Zhong; Shi, Wan-Chao; Li, De-Sheng; Zhang, Zheng-Shan; Zong, Rui; Han, Cong; Zhao, Feng; Feng, Jie (2012). "Moyamoya Disease in China". Stroke. 43 (1): 56–60. doi:10.1161/STROKEAHA.111.621300. PMID 22020027.
- ↑ Online Mendelian Inheritance in Man, https://omim.org/entry/252350 Archived 2021-04-16 at the Wayback Machine
- ↑ Wakai K, Tamakoshi A, Ikezaki K, et al. (1997). "Epidemiological features of moyamoya disease in Japan: findings from a nationwide survey". Clin Neurol Neurosurg. 99 (Suppl 2): S1–5. doi:10.1016/S0303-8467(97)00031-0. PMID 9409395. S2CID 24203502.
- ↑ Hallemeier C, Rich K, Brubb R, Chicoine M, Moran C, Cross D, Zipfel G, Dacey R, Derdeyn CP (2006). "Epidemiological features of moyamoya disease in Japan: findings from a nationwide survey". Stroke. 37 (6): 1490–1496. doi:10.1161/01.STR.0000221787.70503.ca. PMID 16645133.
- ↑ Janda, Paul; Bellew, Jonathan; Veerappan, Venkatachalam (2009). "Moyamoya disease: case report and literature review". The Journal of the American Osteopathic Association. 109 (10): 547–553. PMID 19861596.
- ↑ Kuriyama S, Kusaka Y, Fujimura M, et al. (2008). "Prevalence and clinicoepidemiological features of moyamoya disease in Japan: findings from a nationwide epidemiological survey". Stroke. 39 (1): 42–7. doi:10.1161/STROKEAHA.107.490714. PMID 18048855.
- ↑ You, Chao; Ma, Junpeng; Liu, Yi; Ma, Lu; Huang, Siqing; Li, Hao (2013). "RNF213 polymorphism and moyamoya disease: A systematic review and meta-analysis". Neurology India. 61 (1): 35–9. doi:10.4103/0028-3886.107927. PMID 23466837.
- 1 2 Sudhir, Bhanu Jayanand; Keelara, Arun Gowda; Venkat, Easwer Harihara; Kazumata, Ken; Sundararaman, Ananthalakshmy (2021-09-01). "The mechanobiological theory: a unifying hypothesis on the pathogenesis of moyamoya disease based on a systematic review". Neurosurgical Focus. 51 (3): E6. doi:10.3171/2021.6.FOCUS21281. ISSN 1092-0684. PMID 34469862. S2CID 237388814. Archived from the original on 2022-01-03. Retrieved 2021-12-01.
- ↑ Sudhir, Bhanu Jayanand; Keelara, Arun Gowda; Venkat, Easwer Harihara; Kazumata, Ken; Sundararaman, Ananthalakshmy (2021-09-01). "The mechanobiological theory: a unifying hypothesis on the pathogenesis of moyamoya disease based on a systematic review". Neurosurgical Focus. 51 (3): E6. doi:10.3171/2021.6.FOCUS21281. ISSN 1092-0684. PMID 34469862. S2CID 237388814. Archived from the original on 2022-01-03. Retrieved 2021-12-01.
- ↑ "Moyamoya disease". Genetics Home Reference. Archived from the original on May 6, 2019. Retrieved May 6, 2019.
- 1 2 Hishikawa, Tomohito; Sugiu, Kenji; Date, Isao (August 2016). "Moyamoya Disease: A Review of Clinical Research". Acta Medica Okayama. 70 (4): 229–236. doi:10.18926/amo/54497. PMID 27549666. Archived from the original on 2022-01-11. Retrieved 2021-12-01.
- ↑ Smith, Edward R. (2012). "Moyamoya Arteriopathy". Current Treatment Options in Neurology. 14 (6): 549–556. doi:10.1007/s11940-012-0195-4. PMID 22865293. S2CID 37402408.
- ↑ Moyamoya disease program: Moyamoya treatment videos | Boston Children's Hospital [Video file]. (n.d.). Retrieved from http://www.childrenshospital.org/centers-and-services/programs/f-_-n/moyamoya-disease-program/patient-resources/videos-about-moyamoya/moyamoya-treatment-videos Archived 2022-01-03 at the Wayback Machine
- ↑ Cooke, Rachel (15 October 2019). "A Puff of Smoke by Sarah Lippett review – growing pains". The Guardian. Archived from the original on 3 January 2022. Retrieved 1 December 2021.
- ↑ "Best comics and graphic novels of 2019". The Guardian. 30 November 2019. Archived from the original on 9 February 2020. Retrieved 22 June 2020.
- 1 2 3 4 5 Smith, Edward R. (2015). "Moyamoya Biomarkers". Journal of Korean Neurosurgical Society. 57 (6): 415–21. doi:10.3340/jkns.2015.57.6.415. PMC 4502237. PMID 26180608.
- ↑ Koh, Eun-Jeong; Kim, Han-Na; Ma, Tian-Ze; Choi, Ha-Young; Kwak, Yong-Geun (2010). "Comparative analysis of serum proteomes of moyamoya disease and normal controls". Journal of Korean Neurosurgical Society. 48 (1): 8–13. doi:10.3340/jkns.2010.48.1.8. PMC 2916155. PMID 20717506.
- ↑ Kawakami, Akio; Aikawa, Masanori; Alcaide, Pilar; Luscinskas, Francis W.; Libby, Peter; Sacks, Frank M. (2006). "Apolipoprotein CIII Induces Expression of Vascular Cell Adhesion Molecule-1 in Vascular Endothelial Cells and Increases Adhesion of Monocytic Cells". Circulation. 114 (7): 681–687. doi:10.1161/CIRCULATIONAHA.106.622514. PMID 16894036.
- ↑ Sun, Hai; Wilson, Christopher; Ozpinar, Alp; Safavi-Abbasi, Sam; Zhao, Yan; Nakaji, Peter; Wanebo, John E.; Spetzler, Robert F. (August 2016). "Perioperative complications and long-term outcomes after bypasses in adults with moyamoya disease: a systematic review and meta-analysis". World Neurosurgery. 92: 179–188. doi:10.1016/j.wneu.2016.04.083. ISSN 1878-8769. PMID 27150649.
- ↑ Killory BD, Gonzalez LF, Wait SD, Ponce FA, Albuquerque FC, Spetzler RF (Jun 2008). "Simultaneous unilateral moyamoya disease and ipsilateral dural arteriovenous fistula: case report". Neurosurgery. 62 (6): E1375–6, discussion E1376. doi:10.1227/01.neu.0000333311.87554.9c. PMID 18824958.
External links
- International website for information about diagnostics and treatment of moyamoya patients: https://www.moyamoya.eu Archived 2022-01-03 at the Wayback Machine
- Orphanet's disease page on moyamoya disease Archived 2022-01-03 at the Wayback Machine
- The Indian website for information and treatment of Moyamoya disease: http://moyamoya.sctimst.ac.in Archived 2022-01-03 at the Wayback Machine [1]
| Classification |
|---|
- ↑ "Moyamoya Disease Portal - Sree Chitra Tirunal Institute for Medical Sciences and Technology, Trivandrum (SCTIMST)". moyamoya.sctimst.ac.in. Archived from the original on 2021-09-26. Retrieved 2021-09-26.