Hypoxia-inducible factor
Hypoxia-inducible factors (HIFs) are transcription factors that respond to decreases in available oxygen in the cellular environment, or hypoxia.[1][2] They are only present in parahoxozoan animals.[3]
| hypoxia-inducible factor 1, alpha subunit | |||||||
|---|---|---|---|---|---|---|---|
| Identifiers | |||||||
| Symbol | HIF1A | ||||||
| NCBI gene | 3091 | ||||||
| HGNC | 4910 | ||||||
| OMIM | 603348 | ||||||
| RefSeq | NM_001530 | ||||||
| UniProt | Q16665 | ||||||
| Other data | |||||||
| Locus | Chr. 14 q21-q24 | ||||||
| |||||||
| aryl hydrocarbon receptor nuclear translocator | |||||||
|---|---|---|---|---|---|---|---|
| Identifiers | |||||||
| Symbol | ARNT | ||||||
| Alt. symbols | HIF1B, bHLHe2 | ||||||
| NCBI gene | 405 | ||||||
| HGNC | 700 | ||||||
| OMIM | 126110 | ||||||
| RefSeq | NM_001668 | ||||||
| UniProt | P27540 | ||||||
| Other data | |||||||
| Locus | Chr. 1 q21 | ||||||
| |||||||
| endothelial PAS domain protein 1 | |||||||
|---|---|---|---|---|---|---|---|
| Identifiers | |||||||
| Symbol | EPAS1 | ||||||
| Alt. symbols | HIF2A, MOP2, PASD2, HLF | ||||||
| NCBI gene | 2034 | ||||||
| HGNC | 3374 | ||||||
| OMIM | 603349 | ||||||
| RefSeq | NM_001430 | ||||||
| UniProt | Q99814 | ||||||
| Other data | |||||||
| Locus | Chr. 2 p21-p16 | ||||||
| |||||||
| aryl-hydrocarbon receptor nuclear translocator 2 | |||||||
|---|---|---|---|---|---|---|---|
| Identifiers | |||||||
| Symbol | ARNT2 | ||||||
| Alt. symbols | HIF2B, KIAA0307, bHLHe1 | ||||||
| NCBI gene | 9915 | ||||||
| HGNC | 16876 | ||||||
| OMIM | 606036 | ||||||
| RefSeq | NM_014862 | ||||||
| UniProt | Q9HBZ2 | ||||||
| Other data | |||||||
| Locus | Chr. 1 q24 | ||||||
| |||||||
| hypoxia-inducible factor 3, alpha subunit | |||||||
|---|---|---|---|---|---|---|---|
| Identifiers | |||||||
| Symbol | HIF3A | ||||||
| NCBI gene | 64344 | ||||||
| HGNC | 15825 | ||||||
| OMIM | 609976 | ||||||
| RefSeq | NM_152794 | ||||||
| UniProt | Q9Y2N7 | ||||||
| Other data | |||||||
| Locus | Chr. 19 q13 | ||||||
| |||||||
Discovery
The HIF transcriptional complex was discovered in 1995 by Gregg L. Semenza and postdoctoral fellow Guang Wang.[4][5][6] In 2016, William Kaelin Jr., Peter J. Ratcliffe and Gregg L. Semenza were presented the Lasker Award for their work in elucidating the role of HIF-1 in oxygen sensing and its role in surviving low oxygen conditions.[7] In 2019, the same three individuals were jointly awarded the Nobel Prize in Physiology or Medicine for their work in elucidating how HIF senses and adapts cellular response to oxygen availability.[8]
Structure
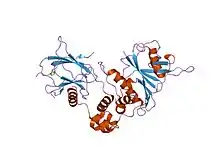
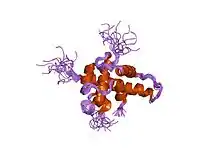
Oxygen-breathing species express the highly conserved transcriptional complex HIF-1, which is a heterodimer composed of an alpha and a beta subunit, the latter being a constitutively-expressed aryl hydrocarbon receptor nuclear translocator (ARNT).[5][9] HIF-1 belongs to the PER-ARNT-SIM (PAS) subfamily of the basic helix-loop-helix (bHLH) family of transcription factors. The alpha and beta subunit are similar in structure and both contain the following domains:[10][11][12]
- N-terminus – a bHLH domain for DNA binding
- central region – Per-ARNT-Sim (PAS) domain, which facilitates heterodimerization
- C-terminus – recruits transcriptional coregulatory proteins
|
| ||||||||||||||||||||||||||||||||||||||||||||||
Members
The following are members of the human HIF family:
| Member | Gene | Protein |
|---|---|---|
| HIF-1α | HIF1A | hypoxia-inducible factor 1, alpha subunit |
| HIF-1β | ARNT | aryl hydrocarbon receptor nuclear translocator |
| HIF-2α | EPAS1 | endothelial PAS domain protein 1 |
| HIF-2β | ARNT2 | aryl-hydrocarbon receptor nuclear translocator 2 |
| HIF-3α | HIF3A | hypoxia inducible factor 3, alpha subunit |
| HIF-3β | ARNT3 | aryl-hydrocarbon receptor nuclear translocator 3 |
Function
HIF1α expression in haematopoietic stem cells explains the quiescence nature of stem cells[15] for being metabolically maintaining at a low rate so as to preserve the potency of stem cells for long periods in a life cycle of an organism.
The HIF signaling cascade mediates the effects of hypoxia, the state of low oxygen concentration, on the cell. Hypoxia often keeps cells from differentiating. However, hypoxia promotes the formation of blood vessels, and is important for the formation of a vascular system in embryos and tumors. The hypoxia in wounds also promotes the migration of keratinocytes and the restoration of the epithelium.[16] It is therefore not surprising that HIF-1 modulation was identified as a promising treatment paradigm in wound healing.[17]
In general, HIFs are vital to development. In mammals, deletion of the HIF-1 genes results in perinatal death.[18] HIF-1 has been shown to be vital to chondrocyte survival, allowing the cells to adapt to low-oxygen conditions within the growth plates of bones. HIF plays a central role in the regulation of human metabolism.[19]
Mechanism
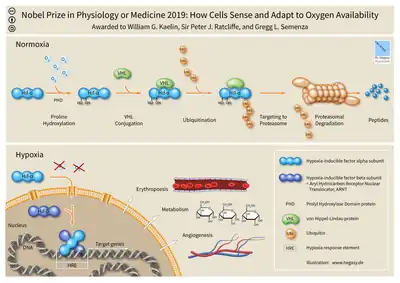
The alpha subunits of HIF are hydroxylated at conserved proline residues by HIF prolyl-hydroxylases, allowing their recognition and ubiquitination by the VHL E3 ubiquitin ligase, which labels them for rapid degradation by the proteasome.[20][21] This occurs only in normoxic conditions. In hypoxic conditions, HIF prolyl-hydroxylase is inhibited, since it utilizes oxygen as a cosubstrate.[22][23]
Inhibition of electron transfer in the succinate dehydrogenase complex due to mutations in the SDHB or SDHD genes can cause a build-up of succinate that inhibits HIF prolyl-hydroxylase, stabilizing HIF-1α. This is termed pseudohypoxia.
HIF-1, when stabilized by hypoxic conditions, upregulates several genes to promote survival in low-oxygen conditions. These include glycolysis enzymes, which allow ATP synthesis in an oxygen-independent manner, and vascular endothelial growth factor (VEGF), which promotes angiogenesis. HIF-1 acts by binding to hypoxia-responsive elements (HREs) in promoters that contain the sequence 5'-RCGTG-3' (where R is a purine, either A or G). Studies demonstrate that hypoxia modulates histone methylation and reprograms chromatin.[24] This paper was published back-to-back with that of 2019 Nobel Prize in Physiology or Medicine winner for Medicine William Kaelin Jr.[25] This work was highlighted in an independent editorial.[26]
It has been shown that muscle A kinase–anchoring protein (mAKAP) organized E3 ubiquitin ligases, affecting stability and positioning of HIF-1 inside its action site in the nucleus. Depletion of mAKAP or disruption of its targeting to the perinuclear (in cardiomyocytes) region altered the stability of HIF-1 and transcriptional activation of genes associated with hypoxia. Thus, "compartmentalization" of oxygen-sensitive signaling components may influence the hypoxic response.[27]
The advanced knowledge of the molecular regulatory mechanisms of HIF1 activity under hypoxic conditions contrast sharply with the paucity of information on the mechanistic and functional aspects governing NF-κB-mediated HIF1 regulation under normoxic conditions. However, HIF-1α stabilization is also found in non-hypoxic conditions through an unknown mechanism. It was shown that NF-κB (nuclear factor κB) is a direct modulator of HIF-1α expression in the presence of normal oxygen pressure. siRNA (small interfering RNA) studies for individual NF-κB members revealed differential effects on HIF-1α mRNA levels, indicating that NF-κB can regulate basal HIF-1α expression. Finally, it was shown that, when endogenous NF-κB is induced by TNFα (tumour necrosis factor α) treatment, HIF-1α levels also change in an NF-κB-dependent manner.[28] HIF-1 and HIF-2 have different physiological roles. HIF-2 regulates erythropoietin production in adult life.[29]
Repair, regeneration and rejuvenation
In normal circumstances after injury HIF-1a is degraded by prolyl hydroxylases (PHDs). In June 2015, scientists found that the continued up-regulation of HIF-1a via PHD inhibitors regenerates lost or damaged tissue in mammals that have a repair response; and the continued down-regulation of Hif-1a results in healing with a scarring response in mammals with a previous regenerative response to the loss of tissue. The act of regulating HIF-1a can either turn off, or turn on the key process of mammalian regeneration.[30][31] One such regenerative process in which HIF1A is involved is skin healing.[32] Researchers at the Stanford University School of Medicine demonstrated that HIF1A activation was able to prevent and treat chronic wounds in diabetic and aged mice. Not only did the wounds in the mice heal more quickly, but the quality of the new skin was even better than the original.[33][34][35] Additionally the regenerative effect of HIF-1A modulation on aged skin cells was described[36][37] and a rejuvenating effect on aged facial skin was demonstrated in patients.[38] HIF modulation has also been linked to a beneficial effect on hair loss.[39] The biotech company Tomorrowlabs GmbH, founded in Vienna in 2016 by the physician Dominik Duscher and pharmacologist Dominik Thor, makes use of this mechanism.[40] Based on the patent-pending HSF ("HIF strengthening factor") active ingredient, products have been developed that are supposed to promote skin and hair regeneration.[41][42][43][44]
As a therapeutic target
Anemia
Several drugs that act as selective HIF prolyl-hydroxylase inhibitors have been developed.[45][46] The most notable compounds are: Roxadustat (FG-4592);[47] Vadadustat (AKB-6548),[48] Daprodustat (GSK1278863),[49] Desidustat (ZYAN-1),[50] and Molidustat (Bay 85-3934),[51] all of which are intended as orally acting drugs for the treatment of anemia.[52] Other significant compounds from this family, which are used in research but have not been developed for medical use in humans, include MK-8617,[53] YC-1,[54] IOX-2,[55] 2-methoxyestradiol,[56] GN-44028,[57] AKB-4924,[58] Bay 87-2243,[59] FG-2216[60] and FG-4497.[61] By inhibiting prolyl-hydroxylase enzyme, the stability of HIF-2α in the kidney is increased, which results in an increase in endogenous production of erythropoietin.[62] Both FibroGen compounds made it through to Phase II clinical trials, but these were suspended temporarily in May 2007 following the death of a trial participant taking FG-2216 from fulminant hepatitis (liver failure), however it is unclear whether this death was actually caused by FG-2216. The hold on further testing of FG-4592 was lifted in early 2008, after the FDA reviewed and approved a thorough response from FibroGen.[63] Roxadustat, vadadustat, daprodustat and molidustat have now all progressed through to Phase III clinical trials for treatment of renal anemia.[47][48][49]
Inflammation and cancer
In other scenarios and in contrast to the therapy outlined above, research suggests that HIF induction in normoxia is likely to have serious consequences in disease settings with a chronic inflammatory component.[64][65][66] It has also been shown that chronic inflammation is self-perpetuating and that it distorts the microenvironment as a result of aberrantly active transcription factors. As a consequence, alterations in growth factor, chemokine, cytokine, and ROS balance occur within the cellular milieu that in turn provide the axis of growth and survival needed for de novo development of cancer and metastasis. These results have numerous implications for a number of pathologies where NF-κB and HIF-1 are deregulated, including rheumatoid arthritis and cancer.[67][68][69][70][71][72] Therefore, it is thought that understanding the cross-talk between these two key transcription factors, NF-κB and HIF, will greatly enhance the process of drug development.[28][73]
HIF activity is involved in angiogenesis required for cancer tumor growth, so HIF inhibitors such as phenethyl isothiocyanate and Acriflavine[74] are (since 2006) under investigation for anti-cancer effects.[75][76][77]
Neurology
Research conducted on mice suggests that stabilizing HIF using an HIF prolyl-hydroxylase inhibitor enhances hippocampal memory, likely by increasing erythropoietin expression.[78] HIF pathway activators such as ML-228 may have neuroprotective effects and are of interest as potential treatments for stroke and spinal cord injury.[79][80]
von Hippel–Lindau disease-associated renal cell carcinoma
Belzutifan is an hypoxia-inducible factor-2α inhibitor[81] under investigation for the treatment of von Hippel–Lindau disease-associated renal cell carcinoma.[82][83][84][85]
See also
References
- Smith TG, Robbins PA, Ratcliffe PJ (May 2008). "The human side of hypoxia-inducible factor". British Journal of Haematology. 141 (3): 325–34. doi:10.1111/j.1365-2141.2008.07029.x. PMC 2408651. PMID 18410568.
- Wilkins SE, Abboud MI, Hancock RL, Schofield CJ (April 2016). "Targeting Protein-Protein Interactions in the HIF System". ChemMedChem. 11 (8): 773–86. doi:10.1002/cmdc.201600012. PMC 4848768. PMID 26997519.
- Mills DB, Francis WR, Vargas S, Larsen M, Elemans CP, Canfield DE, Wörheide G (February 2018). "The last common ancestor of animals lacked the HIF pathway and respired in low-oxygen environments". eLife. 7. doi:10.7554/eLife.31176. PMC 5800844. PMID 29402379.
- Wang GL, Semenza GL (January 1995). "Purification and characterization of hypoxia-inducible factor 1". The Journal of Biological Chemistry. 270 (3): 1230–7. doi:10.1074/jbc.270.3.1230. PMID 7836384. S2CID 41659164.
- Wang GL, Jiang BH, Rue EA, Semenza GL (June 1995). "Hypoxia-inducible factor 1 is a basic-helix-loop-helix-PAS heterodimer regulated by cellular O2 tension". Proceedings of the National Academy of Sciences of the United States of America. 92 (12): 5510–4. Bibcode:1995PNAS...92.5510W. doi:10.1073/pnas.92.12.5510. PMC 41725. PMID 7539918.
- Acker T, Plate KH (2004). "Hypoxia and hypoxia inducible factors (HIF) as important regulators of tumor physiology". Cancer Treatment and Research. 117: 219–48. doi:10.1007/978-1-4419-8871-3_14. ISBN 978-1-4613-4699-9. PMID 15015563.
- "Oxygen sensing – an essential process for survival". Albert Lasker Basic Medical Research Award. Albert And Mary Lasker Foundation. 2016.
- "How cells sense and adapt to oxygen availability". The Nobel Prize in Physiology or Medicine 2019. NobelPrize.org. Nobel Media AB. 7 October 2019.
- Jiang BH, Rue E, Wang GL, Roe R, Semenza GL (July 1996). "Dimerization, DNA binding, and transactivation properties of hypoxia-inducible factor 1". The Journal of Biological Chemistry. 271 (30): 17771–8. doi:10.1074/jbc.271.30.17771. PMID 8663540. S2CID 33729273.
- Zhulin IB, Taylor BL, Dixon R (September 1997). "PAS domain S-boxes in Archaea, Bacteria and sensors for oxygen and redox". Trends in Biochemical Sciences. 22 (9): 331–3. doi:10.1016/S0968-0004(97)01110-9. PMID 9301332.
- Ponting CP, Aravind L (November 1997). "PAS: a multifunctional domain family comes to light". Current Biology. 7 (11): R674-7. doi:10.1016/S0960-9822(06)00352-6. PMID 9382818. S2CID 14105830.
- Yang J, Zhang L, Erbel PJ, Gardner KH, Ding K, Garcia JA, Bruick RK (October 2005). "Functions of the Per/ARNT/Sim domains of the hypoxia-inducible factor". The Journal of Biological Chemistry. 280 (43): 36047–54. doi:10.1074/jbc.M501755200. PMID 16129688. S2CID 46626545.
- Min JH, Yang H, Ivan M, Gertler F, Kaelin WG, Pavletich NP (June 2002). "Structure of an HIF-1alpha -pVHL complex: hydroxyproline recognition in signaling". Science. 296 (5574): 1886–9. Bibcode:2002Sci...296.1886M. doi:10.1126/science.1073440. PMID 12004076. S2CID 19641938.
- Freedman SJ, Sun ZY, Poy F, Kung AL, Livingston DM, Wagner G, Eck MJ (April 2002). "Structural basis for recruitment of CBP/p300 by hypoxia-inducible factor-1 alpha". Proceedings of the National Academy of Sciences of the United States of America. 99 (8): 5367–72. Bibcode:2002PNAS...99.5367F. doi:10.1073/pnas.082117899. PMC 122775. PMID 11959990.
- Srikanth L, Sunitha MM, Venkatesh K, Kumar PS, Chandrasekhar C, Vengamma B, Sarma PV (2015). "Anaerobic Glycolysis and HIF1α Expression in Haematopoietic Stem Cells Explains Its Quiescence Nature". Journal of Stem Cells. 10 (2): 97–106. PMID 27125138.
- Benizri E, Ginouvès A, Berra E (April 2008). "The magic of the hypoxia-signaling cascade". Cellular and Molecular Life Sciences. 65 (7–8): 1133–49. doi:10.1007/s00018-008-7472-0. PMID 18202826. S2CID 44049779.
- Duscher D, Januszyk M, Maan ZN, Whittam AJ, Hu MS, Walmsley GG, et al. (March 2017). "Comparison of the Hydroxylase Inhibitor Dimethyloxalylglycine and the Iron Chelator Deferoxamine in Diabetic and Aged Wound Healing". Plastic and Reconstructive Surgery. 139 (3): 695e–706e. doi:10.1097/PRS.0000000000003072. PMC 5327844. PMID 28234841.
- Duscher D, Maan ZN, Whittam AJ, Sorkin M, Hu MS, Walmsley GG, et al. (November 2015). "Fibroblast-Specific Deletion of Hypoxia Inducible Factor-1 Critically Impairs Murine Cutaneous Neovascularization and Wound Healing". Plastic and Reconstructive Surgery. 136 (5): 1004–13. doi:10.1097/PRS.0000000000001699. PMC 5951620. PMID 26505703.
- Formenti F, Constantin-Teodosiu D, Emmanuel Y, Cheeseman J, Dorrington KL, Edwards LM, et al. (July 2010). "Regulation of human metabolism by hypoxia-inducible factor". Proceedings of the National Academy of Sciences of the United States of America. 107 (28): 12722–7. Bibcode:2010PNAS..10712722F. doi:10.1073/pnas.1002339107. PMC 2906567. PMID 20616028.
- Maxwell PH, Wiesener MS, Chang GW, Clifford SC, Vaux EC, Cockman ME, et al. (May 1999). "The tumour suppressor protein VHL targets hypoxia-inducible factors for oxygen-dependent proteolysis". Nature. 399 (6733): 271–5. Bibcode:1999Natur.399..271M. doi:10.1038/20459. PMID 10353251. S2CID 4427694.
- Perkel J (May 2001). "Seeking a Cellular Oxygen Sensor". The Scientist. Retrieved 7 October 2019.
- Semenza GL (August 2004). "Hydroxylation of HIF-1: oxygen sensing at the molecular level". Physiology. 19 (4): 176–82. doi:10.1152/physiol.00001.2004. PMID 15304631. S2CID 2434206.
- Russo E (April 2003). "Discovering HIF Regulation". The Scientist. Retrieved 7 October 2019.
- Batie M, Frost J, Frost M, Wilson JW, Schofield P, Rocha S (March 2019). "Hypoxia induces rapid changes to histone methylation and reprograms chromatin". Science. 363 (6432): 1222–1226. Bibcode:2019Sci...363.1222B. doi:10.1126/science.aau5870. PMID 30872526. S2CID 78093369.
- Chakraborty AA, Laukka T, Myllykoski M, Ringel AE, Booker MA, Tolstorukov MY, et al. (March 2019). "Histone demethylase KDM6A directly senses oxygen to control chromatin and cell fate". Science. 363 (6432): 1217–1222. Bibcode:2019Sci...363.1217C. doi:10.1126/science.aaw1026. PMC 7336390. PMID 30872525.
- Gallipoli P, Huntly BJ (March 2019). "Histone modifiers are oxygen sensors". Science. 363 (6432): 1148–1149. Bibcode:2019Sci...363.1148G. doi:10.1126/science.aaw8373. PMID 30872506. S2CID 78091150.
- Wong W, Goehring AS, Kapiloff MS, Langeberg LK, Scott JD (December 2008). "mAKAP compartmentalizes oxygen-dependent control of HIF-1alpha". Science Signaling. 1 (51): ra18. doi:10.1126/scisignal.2000026. PMC 2828263. PMID 19109240.
- van Uden P, Kenneth NS, Rocha S (June 2008). "Regulation of hypoxia-inducible factor-1alpha by NF-kappaB". The Biochemical Journal. 412 (3): 477–84. doi:10.1042/BJ20080476. PMC 2474706. PMID 18393939.
- Haase VH (July 2010). "Hypoxic regulation of erythropoiesis and iron metabolism". American Journal of Physiology. Renal Physiology. 299 (1): F1-13. doi:10.1152/ajprenal.00174.2010. PMC 2904169. PMID 20444740.
- eurekalert.org staff (3 June 2015). "Scientist at LIMR leads study demonstrating drug-induced tissue regeneration". eurekalert.org. Lankenau Institute for Medical Research (LIMR). Retrieved 3 July 2015.
- Zhang Y, Strehin I, Bedelbaeva K, Gourevitch D, Clark L, Leferovich J, et al. (June 2015). "Drug-induced regeneration in adult mice". Science Translational Medicine. 7 (290): 290ra92. doi:10.1126/scitranslmed.3010228. PMC 4687906. PMID 26041709.
- Hong WX, Hu MS, Esquivel M, Liang GY, Rennert RC, McArdle A, et al. (May 2014). "The Role of Hypoxia-Inducible Factor in Wound Healing". Advances in Wound Care. 3 (5): 390–399. doi:10.1089/wound.2013.0520. PMC 4005494. PMID 24804159.
- Duscher D, Neofytou E, Wong VW, Maan ZN, Rennert RC, Inayathullah M, et al. (January 2015). "Transdermal deferoxamine prevents pressure-induced diabetic ulcers". Proceedings of the National Academy of Sciences of the United States of America. 112 (1): 94–9. Bibcode:2015PNAS..112...94D. doi:10.1073/pnas.1413445112. PMC 4291638. PMID 25535360.
- Duscher D, Trotsyuk AA, Maan ZN, Kwon SH, Rodrigues M, Engel K, et al. (August 2019). "Optimization of transdermal deferoxamine leads to enhanced efficacy in healing skin wounds". Journal of Controlled Release. 308: 232–239. doi:10.1016/j.jconrel.2019.07.009. PMID 31299261. S2CID 196350143.
- Bonham CA, Rodrigues M, Galvez M, Trotsyuk A, Stern-Buchbinder Z, Inayathullah M, et al. (May 2018). "Deferoxamine can prevent pressure ulcers and accelerate healing in aged mice". Wound Repair and Regeneration. 26 (3): 300–305. doi:10.1111/wrr.12667. PMC 6238634. PMID 30152571.
- "duscher hif - Search Results - PubMed". PubMed. Retrieved 2020-12-04.
- Pagani A, Kirsch BM, Hopfner U, Aitzetmueller MM, Brett EA, Thor D, et al. (June 2020). "Deferiprone Stimulates Aged Dermal Fibroblasts Via HIF-1α Modulation". Aesthetic Surgery Journal. 41 (4): 514–524. doi:10.1093/asj/sjaa142. PMID 32479616.
- Duscher D, Maan ZN, Hu MS, Thor D (November 2020). "A single-center blinded randomized clinical trial to evaluate the anti-aging effects of a novel HSF™-based skin care formulation". Journal of Cosmetic Dermatology. 19 (11): 2936–2945. doi:10.1111/jocd.13356. PMID 32306525. S2CID 216031505.
- Houschyar KS, Borrelli MR, Tapking C, Popp D, Puladi B, Ooms M, et al. (2020). "Molecular Mechanisms of Hair Growth and Regeneration: Current Understanding and Novel Paradigms". Dermatology. 236 (4): 271–280. doi:10.1159/000506155. PMID 32163945. S2CID 212693280.
- Tomorrowlabs. "Tomorrowlabs". Tomorrowlabs. Retrieved 2020-12-04.
- "Kosmetikbranche: Wie das Beauty-Start-up Tomorrowlabs den Markt erobert". www.handelsblatt.com (in German). Retrieved 2020-12-04.
- "Das neue Beauty-Investment von Michael Pieper - HZ". Handelszeitung (in German). Retrieved 2020-12-04.
- andrea.hodoschek (2020-08-03). "Milliardenmarkt Anti-Aging: Start-up aus Österreich mischt mit". kurier.at (in German). Retrieved 2020-12-04.
- "Ein Protein gegen das Altern und für das Geldverdienen". nachrichten.at (in German). Retrieved 2020-12-04.
- Bruegge K, Jelkmann W, Metzen E (2007). "Hydroxylation of hypoxia-inducible transcription factors and chemical compounds targeting the HIF-alpha hydroxylases". Current Medicinal Chemistry. 14 (17): 1853–62. doi:10.2174/092986707781058850. PMID 17627521.
- Maxwell PH, Eckardt KU (March 2016). "HIF prolyl hydroxylase inhibitors for the treatment of renal anaemia and beyond". Nature Reviews. Nephrology. 12 (3): 157–68. doi:10.1038/nrneph.2015.193. PMID 26656456. S2CID 179020.
- Becker K, Saad M (April 2017). "A New Approach to the Management of Anemia in CKD Patients: A Review on Roxadustat". Advances in Therapy. 34 (4): 848–853. doi:10.1007/s12325-017-0508-9. PMID 28290095. S2CID 9818825.
- Pergola PE, Spinowitz BS, Hartman CS, Maroni BJ, Haase VH (November 2016). "Vadadustat, a novel oral HIF stabilizer, provides effective anemia treatment in nondialysis-dependent chronic kidney disease". Kidney International. 90 (5): 1115–1122. doi:10.1016/j.kint.2016.07.019. PMID 27650732.
- Ariazi JL, Duffy KJ, Adams DF, Fitch DM, Luo L, Pappalardi M, et al. (December 2017). "Discovery and Preclinical Characterization of GSK1278863 (Daprodustat), a Small Molecule Hypoxia Inducible Factor-Prolyl Hydroxylase Inhibitor for Anemia". The Journal of Pharmacology and Experimental Therapeutics. 363 (3): 336–347. doi:10.1124/jpet.117.242503. PMID 28928122. S2CID 25100284.
- Kansagra KA, Parmar D, Jani RH, Srinivas NR, Lickliter J, Patel HV, et al. (January 2018). "Phase I Clinical Study of ZYAN1, A Novel Prolyl-Hydroxylase (PHD) Inhibitor to Evaluate the Safety, Tolerability, and Pharmacokinetics Following Oral Administration in Healthy Volunteers". Clinical Pharmacokinetics. 57 (1): 87–102. doi:10.1007/s40262-017-0551-3. PMC 5766731. PMID 28508936.
- Flamme I, Oehme F, Ellinghaus P, Jeske M, Keldenich J, Thuss U (2014). "Mimicking hypoxia to treat anemia: HIF-stabilizer BAY 85-3934 (Molidustat) stimulates erythropoietin production without hypertensive effects". PLOS ONE. 9 (11): e111838. Bibcode:2014PLoSO...9k1838F. doi:10.1371/journal.pone.0111838. PMC 4230943. PMID 25392999.
- Cases A (December 2007). "The latest advances in kidney diseases and related disorders". Drug News & Perspectives. 20 (10): 647–54. PMID 18301799.
- Debenham JS, Madsen-Duggan C, Clements MJ, Walsh TF, Kuethe JT, Reibarkh M, et al. (December 2016). "Discovery of N-[Bis(4-methoxyphenyl)methyl]-4-hydroxy-2-(pyridazin-3-yl)pyrimidine-5-carboxamide (MK-8617), an Orally Active Pan-Inhibitor of Hypoxia-Inducible Factor Prolyl Hydroxylase 1-3 (HIF PHD1-3) for the Treatment of Anemia". Journal of Medicinal Chemistry. 59 (24): 11039–11049. doi:10.1021/acs.jmedchem.6b01242. PMID 28002958.
- Yeo EJ, Chun YS, Cho YS, Kim J, Lee JC, Kim MS, Park JW (April 2003). "YC-1: a potential anticancer drug targeting hypoxia-inducible factor 1". Journal of the National Cancer Institute. 95 (7): 516–25. doi:10.1093/jnci/95.7.516. PMID 12671019.
- Deppe J, Popp T, Egea V, Steinritz D, Schmidt A, Thiermann H, et al. (May 2016). "Impairment of hypoxia-induced HIF-1α signaling in keratinocytes and fibroblasts by sulfur mustard is counteracted by a selective PHD-2 inhibitor". Archives of Toxicology. 90 (5): 1141–50. doi:10.1007/s00204-015-1549-y. PMID 26082309. S2CID 16938364.
- Wang R, Zhou S, Li S (2011). "Cancer therapeutic agents targeting hypoxia-inducible factor-1". Current Medicinal Chemistry. 18 (21): 3168–89. doi:10.2174/092986711796391606. PMID 21671859.
- Minegishi H, Fukashiro S, Ban HS, Nakamura H (February 2013). "Discovery of Indenopyrazoles as a New Class of Hypoxia Inducible Factor (HIF)-1 Inhibitors". ACS Medicinal Chemistry Letters. 4 (2): 297–301. doi:10.1021/ml3004632. PMC 4027554. PMID 24900662.
- Okumura CY, Hollands A, Tran DN, Olson J, Dahesh S, von Köckritz-Blickwede M, et al. (September 2012). "A new pharmacological agent (AKB-4924) stabilizes hypoxia inducible factor-1 (HIF-1) and increases skin innate defenses against bacterial infection". Journal of Molecular Medicine. 90 (9): 1079–89. doi:10.1007/s00109-012-0882-3. PMC 3606899. PMID 22371073.
- Görtz GE, Horstmann M, Aniol B, Reyes BD, Fandrey J, Eckstein A, Berchner-Pfannschmidt U (December 2016). "Hypoxia-Dependent HIF-1 Activation Impacts on Tissue Remodeling in Graves' Ophthalmopathy-Implications for Smoking". The Journal of Clinical Endocrinology and Metabolism. 101 (12): 4834–4842. doi:10.1210/jc.2016-1279. PMID 27610652.
- Beuck S, Schänzer W, Thevis M (November 2012). "Hypoxia-inducible factor stabilizers and other small-molecule erythropoiesis-stimulating agents in current and preventive doping analysis". Drug Testing and Analysis. 4 (11): 830–45. doi:10.1002/dta.390. PMID 22362605.
- Silva PL, Rocco PR, Pelosi P (August 2015). "FG-4497: a new target for acute respiratory distress syndrome?". Expert Review of Respiratory Medicine. 9 (4): 405–9. doi:10.1586/17476348.2015.1065181. PMID 26181437. S2CID 5817105.
- Hsieh MM, Linde NS, Wynter A, Metzger M, Wong C, Langsetmo I, et al. (September 2007). "HIF prolyl hydroxylase inhibition results in endogenous erythropoietin induction, erythrocytosis, and modest fetal hemoglobin expression in rhesus macaques". Blood. 110 (6): 2140–7. doi:10.1182/blood-2007-02-073254. PMC 1976368. PMID 17557894.
- "The FDA Accepts the Complete Response for Clinical Holds of FG-2216/FG-4592 for the Treatment of Anemia" (PDF). Archived from the original (PDF) on 2015-09-23. Retrieved 2008-10-28.
- Eltzschig HK, Bratton DL, Colgan SP (November 2014). "Targeting hypoxia signalling for the treatment of ischaemic and inflammatory diseases". Nature Reviews. Drug Discovery. 13 (11): 852–69. doi:10.1038/nrd4422. PMC 4259899. PMID 25359381.
- Salminen A, Kaarniranta K, Kauppinen A (August 2016). "AMPK and HIF signaling pathways regulate both longevity and cancer growth: the good news and the bad news about survival mechanisms". Biogerontology. 17 (4): 655–80. doi:10.1007/s10522-016-9655-7. PMID 27259535. S2CID 4386269.
- Taylor CT, Doherty G, Fallon PG, Cummins EP (October 2016). "Hypoxia-dependent regulation of inflammatory pathways in immune cells". The Journal of Clinical Investigation. 126 (10): 3716–3724. doi:10.1172/JCI84433. PMC 5096820. PMID 27454299.
- Cummins EP, Keogh CE, Crean D, Taylor CT (2016). "The role of HIF in immunity and inflammation". Molecular Aspects of Medicine. 47–48: 24–34. doi:10.1016/j.mam.2015.12.004. hdl:10197/9767. PMID 26768963.
- Hua S, Dias TH (2016). "Hypoxia-Inducible Factor (HIF) as a Target for Novel Therapies in Rheumatoid Arthritis". Frontiers in Pharmacology. 7: 184. doi:10.3389/fphar.2016.00184. PMC 4921475. PMID 27445820.
- Ezzeddini R, Taghikhani M, Somi MH, Samadi N, Rasaee, MJ (May 2019). "Clinical importance of FASN in relation to HIF-1α and SREBP-1c in gastric adenocarcinoma". Life Sciences. 224: 169–176. doi:10.1016/j.lfs.2019.03.056. PMID 30914315. S2CID 85532042.
- Singh D, Arora R, Kaur P, Singh B, Mannan R, Arora S (2017). "Overexpression of hypoxia-inducible factor and metabolic pathways: possible targets of cancer". Cell & Bioscience. 7: 62. doi:10.1186/s13578-017-0190-2. PMC 5683220. PMID 29158891.
- Huang Y, Lin D, Taniguchi CM (October 2017). "Hypoxia inducible factor (HIF) in the tumor microenvironment: friend or foe?". Science China Life Sciences. 60 (10): 1114–1124. doi:10.1007/s11427-017-9178-y. PMC 6131113. PMID 29039125.
- Ezzeddini R, Taghikhani M, Salek Farrokhi A, Somi MH, Samadi N, Esfahani A, Rasaee, MJ (May 2021). "Downregulation of fatty acid oxidation by involvement of HIF-1α and PPARγ in human gastric adenocarcinoma and its related clinical significance". Journal of Physiology and Biochemistry. 77 (2): 249–260. doi:10.1007/s13105-021-00791-3. PMID 33730333. S2CID 232300877.
- D'Ignazio L, Bandarra D, Rocha S (February 2016). "NF-κB and HIF crosstalk in immune responses". The FEBS Journal. 283 (3): 413–24. doi:10.1111/febs.13578. PMC 4864946. PMID 26513405.
- Lee K, Zhang H, Qian DZ, Rey S, Liu JO, Semenza GL (October 2009). "Acriflavine inhibits HIF-1 dimerization, tumor growth, and vascularization". Proceedings of the National Academy of Sciences of the United States of America. 106 (42): 17910–5. Bibcode:2009PNAS..10617910L. doi:10.1073/pnas.0909353106. PMC 2764905. PMID 19805192.
- Syed Alwi SS, Cavell BE, Telang U, Morris ME, Parry BM, Packham G (November 2010). "In vivo modulation of 4E binding protein 1 (4E-BP1) phosphorylation by watercress: a pilot study". The British Journal of Nutrition. 104 (9): 1288–96. doi:10.1017/S0007114510002217. PMC 3694331. PMID 20546646.
- Semenza GL (October 2007). "Evaluation of HIF-1 inhibitors as anticancer agents". Drug Discovery Today. 12 (19–20): 853–9. doi:10.1016/j.drudis.2007.08.006. PMID 17933687.
- Melillo G (September 2006). "Inhibiting hypoxia-inducible factor 1 for cancer therapy". Molecular Cancer Research. 4 (9): 601–5. doi:10.1158/1541-7786.MCR-06-0235. PMID 16940159. S2CID 21525087.
- Adamcio B, Sperling S, Hagemeyer N, Walkinshaw G, Ehrenreich H (March 2010). "Hypoxia inducible factor stabilization leads to lasting improvement of hippocampal memory in healthy mice". Behavioural Brain Research. 208 (1): 80–4. doi:10.1016/j.bbr.2009.11.010. PMID 19900484. S2CID 20395457.
- Xing J, Lu J (2016). "HIF-1α Activation Attenuates IL-6 and TNF-α Pathways in Hippocampus of Rats Following Transient Global Ischemia". Cellular Physiology and Biochemistry. 39 (2): 511–20. doi:10.1159/000445643. PMID 27383646. S2CID 30553076.
- Chen H, Li J, Liang S, Lin B, Peng Q, Zhao P, et al. (March 2017). "Effect of hypoxia-inducible factor-1/vascular endothelial growth factor signaling pathway on spinal cord injury in rats". Experimental and Therapeutic Medicine. 13 (3): 861–866. doi:10.3892/etm.2017.4049. PMC 5403438. PMID 28450910.
- Choueiri TK, Bauer TM, Papadopoulos KP, Plimack ER, Merchan JR, McDermott DF, et al. (April 2021). "Inhibition of hypoxia-inducible factor-2α in renal cell carcinoma with belzutifan: a phase 1 trial and biomarker analysis". Nat Med. 27 (5): 802–805. doi:10.1038/s41591-021-01324-7. PMC 9128828. PMID 33888901. S2CID 233371559.
- "Belzutifan". SPS - Specialist Pharmacy Service. 18 March 2021. Retrieved 25 April 2021.
- "MHRA awards first 'innovation passport' under new pathway". RAPS (Press release). Retrieved 25 April 2021.
- "Merck Receives Priority Review From FDA for New Drug Application for HIF-2α Inhibitor Belzutifan (MK-6482)" (Press release). Merck. 16 March 2016. Retrieved 25 April 2021 – via Business Wire.
- "FDA Grants Priority Review to Belzutifan for von Hippel-Lindau Disease–Associated RCC". Cancer Network. Retrieved 2021-04-26.
External links
- Hypoxia-Inducible+Factor+1 at the U.S. National Library of Medicine Medical Subject Headings (MeSH)
- PDBe-KB provides an overview of all the structure information available in the PDB for Human Hypoxia-inducible factor 1-alpha
- PDBe-KB provides an overview of all the structure information available in the PDB for Human Aryl hydrocarbon receptor nuclear translocator
- PDBe-KB provides an overview of all the structure information available in the PDB for Human Endothelial PAS domain-containing protein 1
- PDBe-KB provides an overview of all the structure information available in the PDB for Human Hypoxia-inducible factor 3-alpha
- short scientific animation visualises the crystal structure of the Heterodimeric HIF-1a:ARNT Complex with HRE DNA