Bivalirudin
 | |
| Names | |
|---|---|
| Trade names | Angiomax, Angiox, others |
| Clinical data | |
| Drug class | Direct thrombin inhibitor (DTI)[1] |
| Main uses | Percutaneous coronary intervention (PCI)[1] |
| Side effects | Bleeding[1] |
| WHO AWaRe | UnlinkedWikibase error: ⧼unlinkedwikibase-error-statements-entity-not-set⧽ |
| Routes of use | Intravenous |
| External links | |
| AHFS/Drugs.com | Monograph |
| Legal | |
| License data | |
| Legal status |
|
| Pharmacokinetics | |
| Bioavailability | N/A (IV application only) |
| Metabolism | cleared from plasma by a combination of kidneys and proteolytic cleavage |
| Elimination half-life | ~25 minutes with normal kidney function |
| Chemical and physical data | |
| Formula | C98H138N24O33 |
| Molar mass | 2180.317 g·mol−1 |
| 3D model (JSmol) | |
SMILES
| |
InChI
| |
Bivalirudin, sold under the brand names Angiomax and Angiox, is a medication used during percutaneous coronary intervention (PCI).[1] It can be used in people with heparin-induced thrombocytopenia (HIT).[1] It is given by injection into a vein.[1]
Common side effects include bleeding.[1] Safety in pregnancy is unclear.[1] It is a direct thrombin inhibitor (DTI) and a manufactured version of hirudin.[1][2]
Bivalirudin was approved for medical use in the United States in 2000.[1] While it was approved in Europe in 2004, this approval was subsequently withdrawn.[3] It is available as a generic medication.[2] In the United States 250 mg costs about 115 USD as of 2022.[4]
Medical uses
- Bivalirudin is indicated for use as an anticoagulant in patients with unstable angina undergoing percutaneous transluminal coronary angioplasty (PTCA).
- Bivalirudin with provisional use of glycoprotein IIb/IIIa inhibitor (GPI) is indicated for use as an anticoagulant in patients undergoing percutaneous coronary intervention (PCI).
- Bivalirudin is indicated for patients with, or at risk of HIT/HITTS undergoing PCI.
- Bivalirudin is intended for use with aspirin and has been studied only in patients receiving concomitant aspirin
It appears to behave in a manner similar to that in adults.[5]
Dosage
Bivalirudin is intended for IV use and is supplied as a sterile, lyophilized product in single-use, glass vials. After reconstitution, each vial delivers 250 mg of bivalirudin.
US dosing:
- PCI bolus: 0.75 mg/kg
- PCI infusion: 1.75 mg/kg/h
EU dosing:[6]
- UA/NSTEMI
-Bolus: 0.1 mg/kg -Infusion: 0.25 mg/kg/h for up to 72 hours for medical management -If patient proceeds to PCI, an additional bolus of 0.5 mg/kg of bivalirudin should be administered before the procedure and the infusion increased to 1.75 mg/kg/h for the duration of the procedure.
- PCI
-Bolus: 0.75 mg/kg -Infusion: 1.75 mg/kg/h
- Coronary Artery Bypass Graft (CABG)
-Patients proceeding to CABG surgery off-pump:
The IV infusion of bivalirudin should be continued until the time of surgery. Just prior to surgery, a 0.5 mg/kg bolus dose should be administered followed by a 1.75 mg/kg/h infusion for the duration of the surgery. -Patients proceeding to CABG surgery on-pump:
The IV infusion of bivalirudin should be continued until 1 hour prior to surgery after which the infusion should be discontinued
Five minutes after the bolus dose has been administered, an activating clotting time (ACT) should be performed and an additional bolus of 0.3 mg/kg should be given if needed.
Continuation of the bivalirudin infusion following PCI for up to 4 hours post-procedure is optional, at the discretion of the treating physician. After 4 hours, an additional IV infusion of bivalirudin may be initiated at a rate of 0.2 or 0.25 mg/kg/h for up to 20 hours, if needed.[6]
Bivalirudin should be administered with optimal antiplatelet therapy (aspirin plus clopidogrel).[6]
Kidney problems
A reduction in the infusion dose of bivalirudin should be considered in patients with moderate or severe renal impairment. If a patient is on hemodialysis, the infusion should be reduced to 0.25 mg/kg/h. No reduction in the bolus dose is needed.[6]
Side effects
Bivalirudin is contraindicated in people with active major bleeding and hypersensitivity to bivalirudin or its components. (In the EU bivalirudin is also contraindicated in patients with an increased risk of bleeding due to hemostasis disorders and/or irreversible coagulation disorders, severe uncontrolled hypertension, subacute bacterial endocarditis, and severe renal impairment [GFR<30 ml/min] and in dialysis-dependent patients).[6]
Bivalirudin is an anticoagulant. Therefore, bleeding is an expected adverse event. In clinical trials, bivalirudin treated patients exhibited statistically significantly lower rates of bleeding than patients treated with heparin plus a GP IIb/IIIa inhibitor. The most common (≥10%) adverse events of bivalirudin are back pain, pain, nausea, headache, and hypotension.[6]
Bivalirudin is classified as Pregnancy Category B.[6]
Mechanism of action
Bivalirudin directly inhibits thrombin by specifically binding both to the catalytic site and to the anion-binding exosite of circulating and clot-bound thrombin. Thrombin is a serine proteinase that plays a central role in the thrombotic process. It cleaves fibrinogen into fibrin monomers, activates Factor V, VIII, and XIII, allowing fibrin to develop a covalently cross-linked framework that stabilizes the thrombus. Thrombin also promotes further thrombin generation, and activates platelets, stimulating aggregation and granule release. The binding of bivalirudin to thrombin is reversible as thrombin slowly cleaves the bivalirudin-Arg3-Pro4 bond, resulting in recovery of thrombin active site functions.[7]
A short, synthetic peptide, it is a potent and highly specific inhibitor of thrombin that inhibits both circulating and clot-bound thrombin, while also inhibiting thrombin-mediated platelet activation and aggregation.[8] Bivalirudin has a quick onset of action and a short half-life. It does not bind to plasma proteins (other than thrombin) or to red blood cells. Therefore, it has a predictable antithrombotic response. There is no risk for heparin-induced thrombocytopenia or heparin-induced thrombosis-thrombocytopenia syndrome. It does not require a binding cofactor such as antithrombin and does not activate platelets.[9]
Pharmacokinetics
- Following an IV bolus of bivalirudin of 1 mg/kg and a 4-hour 2.5 mg/kg/h IV infusion a mean steady state concentration of 12.3 ± 1.7 µg/mL is achieved
- Bivalirudin is cleared from plasma by a combination of renal mechanisms and proteolytic cleavage
- Half-life:
-Normal renal function (≥ 90 mL/min) = 25 minutes
-Mild renal dysfunction (60–89 mL/min) = 22 minutes
-Moderate renal dysfunction (30-59 mL/min) = 34 minutes
-Severe renal dysfunction (≤ 29 mL/min) = 57 minutes
-Dialysis-dependent = 3.5 hours
- Clearance is reduced approximately 20% in patients with moderate and severe renal impairment and by 80% in dialysis-dependent patients
- Bivalirudin is hemodialyzable and approximately 25% is cleared by hemodialysis.
Pharmacodynamics
Coagulation times return to baseline approximately 1 hour following cessation of bivalirudin administration.
Chemistry
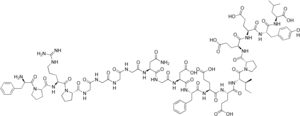
Bivalirudin is a 20 amino acid long peptide with the sequence D-Phe-Pro-Arg-Pro-Gly-Gly-Gly-Gly-Asn-Gly-Asp-Phe-Glu-Glu-Ile-Pro-Glu-Glu-Tyr-Leu (FPRPGGGGNGDFEEIPEEYL), where the first residue is D-phenylalanine instead of the natural L-phenylalanine.
It is also known as d-Phenylalanyl-l-prolyl-l-arginyl-l-prolylglycylglycylglycylglycyl-l-asparaginylglycyl-l-alpha-aspartyl-l-phenylalanyl-l-alpha-glutamyl-l-alpha-glutamyl-l-isoleucyl-l-prolyl-l-alpha-glutamyl-l-alpha-glutamyl-l-tyrosyl-l-leucine
Chemically, it is a synthetic congener of the naturally occurring drug hirudin, found in the saliva of the medicinal leech Hirudo medicinalis.
Research
Bivalirudin studies demonstrated positive outcomes in patients with stable angina, unstable angina (UA), non–ST-segment elevation myocardial infarction (NSTEMI), and ST-segment elevation myocardial infarction (STEMI) undergoing PCI in seven major randomized trials.[8][10][11]
Guidelines
Bivalirudin has Class I recommendations in multiple national guidelines.
| Patient Type | Guidelines | Recommendations |
|---|---|---|
| STEMI and primary PCI | ACC/AHA/SCAI 2009 Joint STEMI/PCI Focused Update | Class I-B, IIa-B |
| UA/NSTEMI | ACC/AHA 2007 guidelines for UA/NSTEMI patients | Class I-B, IIa-B |
| NSTE-ACS patients | ACCP 2008 clinical practice guidelines for patients with NSTE-ACS | Grade 1A, 2B |
| PCI | ACCP 2008 clinical practice guidelines for patients with NSTE-ACS | Grade 1B |
| Patient Type | Guidelines | Recommendations |
|---|---|---|
| STEMI | European Society of Cardiology 2008 | Class IIa – B |
| NSTE-ACS | European Society of Cardiology 2007 | Class IIa-B, IB |
| PCI | European Society of Cardiology 2005 | Class IIa C, IC |
See also
References
- 1 2 3 4 5 6 7 8 9 10 "DailyMed - BIVALIRUDIN injection". dailymed.nlm.nih.gov. Archived from the original on 11 April 2021. Retrieved 10 January 2022.
- 1 2 "Bivalirudin Monograph for Professionals". Drugs.com. Archived from the original on 5 March 2021. Retrieved 11 January 2022.
- ↑ "Angiox". Archived from the original on 24 March 2021. Retrieved 10 January 2022.
- ↑ "Bivalirudin Prices, Coupons & Patient Assistance Programs". Drugs.com. Retrieved 11 January 2022.
- ↑ Zamora R, Forbes T, Hijazi Z, Qureshi A, Ringewald J, Rome J, Vincent R (2009). "Bivalirudin (Angiomax®) As a Procedural Anticoagulant in the Pediatric Population Undergoing Intravascular Procedures for Congenital Heart Disease". Catheterization and Cardiovascular Interventions. 73 (S1): S8.
- 1 2 3 4 5 6 7 "Annex 1 - Summary of Product Characteristics" (PDF). www.themedicinescompany.com. The Medicines Company UK Ltd. March 2010. Archived from the original (PDF) on 26 April 2012. Retrieved 2 December 2011.
- ↑ "Angiomax US PI June 2013" (PDF). Angiomax.com. Archived from the original (PDF) on 2015-02-03.
- 1 2 Stone GW, McLaurin BT, Cox DA, Bertrand ME, Lincoff AM, Moses JW, et al. (November 2006). "Bivalirudin for patients with acute coronary syndromes" (PDF). The New England Journal of Medicine. 355 (21): 2203–16. doi:10.1056/NEJMoa062437. hdl:2445/49765. PMID 17124018. Archived (PDF) from the original on 2017-08-09. Retrieved 2021-07-10.
- ↑ Weitz JI, Bates SM (April 2002). "Acute coronary syndromes: a focus on thrombin". The Journal of Invasive Cardiology. 14 Suppl B: 2B–7B. PMID 11967385.
- ↑ Bittl JA, Chaitman BR, Feit F, Kimball W, Topol EJ (December 2001). "Bivalirudin versus heparin during coronary angioplasty for unstable or postinfarction angina: Final report reanalysis of the Bivalirudin Angioplasty Study". American Heart Journal. 142 (6): 952–9. doi:10.1067/mhj.2001.119374. PMID 11717596.
- ↑ Lincoff AM, Bittl JA, Harrington RA, Feit F, Kleiman NS, Jackman JD, et al. (February 2003). "Bivalirudin and provisional glycoprotein IIb/IIIa blockade compared with heparin and planned glycoprotein IIb/IIIa blockade during percutaneous coronary intervention: REPLACE-2 randomized trial". JAMA. 289 (7): 853–63. doi:10.1001/jama.289.7.853. PMID 12588269.
- ↑ Kushner FG, Hand M, Smith SC, King SB, Anderson JL, Antman EM, et al. (December 2009). "2009 focused updates: ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction (updating the 2004 guideline and 2007 focused update) and ACC/AHA/SCAI guidelines on percutaneous coronary intervention (updating the 2005 guideline and 2007 focused update) a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines". Journal of the American College of Cardiology. 54 (23): 2205–41. doi:10.1016/j.jacc.2009.10.015. PMID 19942100.
- ↑ Anderson JL, Adams CD, Antman EM, Bridges CR, Califf RM, Casey DE, et al. (August 2007). "ACC/AHA 2007 guidelines for the management of patients with unstable angina/non-ST-Elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 2002 Guidelines for the Management of Patients With Unstable Angina/Non-ST-Elevation Myocardial Infarction) developed in collaboration with the American College of Emergency Physicians, the Society for Cardiovascular Angiography and Interventions, and the Society of Thoracic Surgeons endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation and the Society for Academic Emergency Medicine". Journal of the American College of Cardiology. 50 (7): e1–e157. doi:10.1016/j.jacc.2007.02.013. PMID 17692738.
- ↑ Harrington RA, Becker RC, Cannon CP, Gutterman D, Lincoff AM, Popma JJ, et al. (June 2008). "Antithrombotic therapy for non-ST-segment elevation acute coronary syndromes: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition)". Chest. 133 (6 Suppl): 670S–707S. doi:10.1378/chest.08-0691. PMID 18574276.
- ↑ Silber S, Albertsson P, Avilés FF, Camici PG, Colombo A, Hamm C, et al. (April 2005). "Guidelines for percutaneous coronary interventions. The Task Force for Percutaneous Coronary Interventions of the European Society of Cardiology". European Heart Journal. 26 (8): 804–47. doi:10.1093/eurheartj/ehi138. PMID 15769784.
- ↑ Bassand JP, Hamm CW, Ardissino D, Boersma E, Budaj A, Fernández-Avilés F, et al. (July 2007). "Guidelines for the diagnosis and treatment of non-ST-segment elevation acute coronary syndromes". European Heart Journal. 28 (13): 1598–660. doi:10.1093/eurheartj/ehm161. PMID 17569677.
- ↑ Van de Werf F, Bax J, Betriu A, Blomstrom-Lundqvist C, Crea F, Falk V, et al. (December 2008). "Management of acute myocardial infarction in patients presenting with persistent ST-segment elevation: the Task Force on the Management of ST-Segment Elevation Acute Myocardial Infarction of the European Society of Cardiology". European Heart Journal. 29 (23): 2909–45. doi:10.1093/eurheartj/ehn416. PMID 19004841.
External links
| Identifiers: |
|---|
- Heparin More Effective Than Bivalirudin in Treating Patients During PCI - Diagnostic and interventional cardiology magazine Archived 2016-05-16 at the Wayback Machine