Cholestasis
| Cholestasis | |
|---|---|
| Other names: Cholestatic liver disease, cholestatic jaundice | |
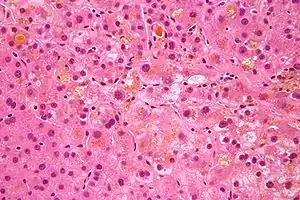 | |
| Micrograph showing bile (yellow) stasis, i.e. cholestasis. H&E stain. | |
| Specialty | Gastroenterology |
| Symptoms | Itchiness, fatty stool, tiredness, fatty deposits in the skin, yellowish skin and eyes[1] |
| Complications | Fat soluble vitamin deficiency[1] |
| Types | Extrahepatic, intrahepatic[1] |
| Causes | Extrahepatic: Common bile duct stones, bile duct strictures, sclerosing cholangitis, bile duct cancer, pancreatic cancer[1] Intrahepatic: Viral hepatitis, alcoholic hepatitis, certain medications, pregnancy, sepsis, cystic fibrosis, primary biliary cholangitis[1] |
| Diagnostic method | High direct bilirubin and high serum alkaline phosphatase[1] |
| Treatment | Surgery, medication[1] |
| Medication | Cholestyramine, ursodeoxycholic acid, antihistamines, naloxone[1] |
| Frequency | Commons[2] |
Cholestasis is a condition of decreased bile production or flow from the liver to the intestines.[1] Symptoms may include itchiness, fatty stool, tiredness, fatty deposits in the skin, and yellowish skin and eyes.[1] Complications may include deficiencies of fat soluble vitamins.[1]
The causes are divided into those outside the liver and those within the liver.[1] Causes outside the liver include common bile duct stones, bile duct strictures, sclerosing cholangitis, bile duct cancer, and pancreatic cancer.[1] Causes within the liver include viral hepatitis, alcoholic hepatitis, certain medications, pregnancy, sepsis, cystic fibrosis, and primary biliary cholangitis.[1] Blood tests may show a high direct bilirubin and serum alkaline phosphatase.[1]
Treatment depends on the underlying cause and symptoms.[1] Blockages of the bile ducts may be treated by surgery.[1] Itchiness may be improved with cholestyramine, ursodeoxycholic acid, antihistamines, and naloxone.[1] Other options for itchiness may include light therapy and plasmapheresis.[1] Cholestasis is common, with blockage of bile ducts the most frequent type.[3][2] The term "cholestasis" is from the Greek for "standing still of bile".[4]
Signs and symptoms
- Itchiness is the primary symptom of cholestasis and is thought to be due to interactions of serum bile acids with opioidergic nerves. In fact, the opioid antagonist naltrexone is used to treat pruritus due to cholestasis.
- Jaundice is an uncommon occurrence in intrahepatic (metabolic) cholestasis, but is common in obstructive cholestasis.
- Pale stool implies obstructive cholestasis.
- Dark urine
Causes
Possible causes:
- pregnancy
- androgens
- birth control pills
- antibiotics (such as TMP/SMX)
- abdominal mass (e.g. cancer)
- biliary atresia and other pediatric liver diseases
- biliary trauma
- congenital anomalies of the biliary tract
- gallstones
- biliary dyskinesia
- acute hepatitis
- cystic fibrosis
- intrahepatic cholestasis of pregnancy (obstetric cholestasis)
- primary biliary cholangitis, an autoimmune disorder
- primary sclerosing cholangitis, associated with inflammatory bowel disease
- some drugs (e.g. flucloxacillin and erythromycin)
Drugs such as gold salts, nitrofurantoin, anabolic steroids, chlorpromazine, prochlorperazine, sulindac, cimetidine, erythromycin, estrogen, and statins can cause cholestasis and may result in damage to the liver.
Mechanism
Bile is secreted by the liver to aid in the digestion of fats. Bile formation begins in bile canaliculi that form between two adjacent surfaces of liver cells (hepatocytes) similar to the terminal branches of a tree. The canaliculi join each other to form larger and larger structures, sometimes referred to as the canals of Hering, which themselves join to form small bile ductules that have an epithelial surface. The ductules join to form bile ducts that eventually form either the right main hepatic duct that drains the right lobe of the liver, or the left main hepatic duct draining the left lobe of the liver. The two ducts join to form the common hepatic duct, which in turn joins the cystic duct from the gall bladder, to give the common bile duct. This duct then enters the duodenum at the ampulla of Vater.
In cholestasis, bile accumulates in the hepatic parenchyma.[5]
Diagnosis
Cholestasis can be suspected when there is an elevation of both 5'-nucleotidase and ALP enzymes. With a few exceptions, the optimal test for cholestasis would be elevations of serum bile acid levels. However, this is not normally available in most clinical settings. The gamma-glutamyl transferase (GGT) enzyme was previously thought to be helpful in confirming a hepatic source of ALP; however, GGT elevations lack the necessary specificity to be a useful confirmatory test for ALP. Normally GGT and ALP are anchored to membranes of hepatocytes and are released in small amounts in hepatocellular damage. In cholestasis, synthesis of these enzymes is induced and they are made soluble. GGT is elevated because it leaks out from the bile duct cells due to pressure from inside bile ducts.
In a later stage of cholestasis AST, ALT and unconjugated bilirubin may be elevated due to hepatocyte damage as a secondary effect of cholestasis.
Histopathology
Under a microscope, the individual hepatocytes will have a brownish-green stippled appearance within the cytoplasm, representing bile that cannot get out of the cell. Canalicular bile plugs between individual hepatocytes or within bile ducts may also be seen, representing bile that has been excreted from the hepatocytes but cannot go any further due to the obstruction. When these plugs occur within the bile duct, sufficient pressure (caused by bile accumulation) can cause them to rupture, spilling bile into the surrounding tissue, causing hepatic necrosis. These areas are known as bile lakes, and are typically seen only with extra-hepatic obstruction.
Management
Extrahepatic cholestasis can usually be treated by surgery.
Pruritus in cholestatic jaundice is treated by antihistamines, ursodeoxycholic acid, and phenobarbital. Nalfurafine hydrochloride can also treat pruritus caused by chronic liver disease and was recently approved in Japan for this purpose.
See also
- Liver function tests
- Lipoprotein-X - an abnormal low density lipoprotein found in cholestasis
- Intrahepatic cholestasis of pregnancy
- Progressive familial intrahepatic cholestasis
- Feathery degeneration - a histopathologic finding associated with cholestasis
References
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 Shah, R; John, S (January 2020). "Cholestatic Jaundice". PMID 29489239.
{{cite journal}}: Cite journal requires|journal=(help) - 1 2 Samant, H; Manatsathit, W; Dies, D; Shokouh-Amiri, H; Zibari, G; Boktor, M; Alexander, JS (6 July 2019). "Cholestatic liver diseases: An era of emerging therapies". World journal of clinical cases. 7 (13): 1571–1581. doi:10.12998/wjcc.v7.i13.1571. PMID 31367616.
- ↑ Burtis, Carl A.; Ashwood, Edward R.; Bruns, David E. (2012). Tietz Textbook of Clinical Chemistry and Molecular Diagnostics - E-Book. Elsevier Health Sciences. p. 1676. ISBN 978-1-4557-5942-2. Archived from the original on 2021-08-28. Retrieved 2021-02-20.
- ↑ Clinic, Cleveland (2010). Current Clinical Medicine E-Book: Expert Consult - Online. Elsevier Health Sciences. p. 552. ISBN 978-1-4377-3571-0. Archived from the original on 2021-08-28. Retrieved 2021-02-20.
- ↑ Kumar (2015). Robbins and Cotran Pathologic Basis of Disease (9 ed.). Elsevier. pp. 821–881.
External links
| Classification | |
|---|---|
| External resources |