Spontaneous bacterial peritonitis
| Spontaneous bacterial peritonitis | |
|---|---|
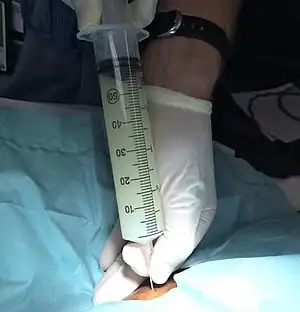 | |
| Turbid peritoneal fluid withdrawn during a diagnostic paracentesis, which is consistent with SPB.[1] | |
| Specialty | Gastroenterology |
| Symptoms | Mild to moderate diffuse abdominal pain, confusion, fever[2][3] |
| Complications | Kidney problems, further liver problems, gastrointestinal bleeding[4] |
| Risk factors | Liver cirrhosis, peritoneal carcinomatosis, heart failure, pancreatitis, nephrotic syndrome[3] |
| Diagnostic method | Paracentesis[3] |
| Treatment | Antibiotics, albumin[3] |
| Medication | Ceftriaxone, piperacillin/tazobactam, carbapenem[3] |
| Frequency | 15% of people admitted to hospital due to cirrhosis[3] |
| Deaths | 30% at one month; 60% dead at a year[3] |
Spontaneous bacterial peritonitis (SBP) is a bacterial infection of ascitic fluid in the abdomen without an obvious source.[2] Symptoms generally include diffuse, mild to moderate abdominal pain that is constant in nature.[2] Other symptoms may include fever or confusion.[3] Complications may include kidney problems, further liver problems, and gastrointestinal bleeding.[4]
Risk factors include liver cirrhosis, peritoneal carcinomatosis, heart failure, pancreatitis, and nephrotic syndrome.[3] The most common organisms involved are gram-negative bacteria, such as E. coli.[3] Diagnosis is by paracentesis, sampling of the peritoneal fluid.[3] It is confirmed if the fluid contains large numbers of white blood cells known as neutrophils (>250 cells/µL).[4]
Treatment is with antibiotics, without waiting for culture results.[5] For those who develop infection in the community, generally ceftriaxone is used; while in those who develop infection in hospital piperacillin/tazobactam of a carbapenem is used.[3] Infusions of albumin may also generally given.[3] In those with cirrhosis who have a GI bleed, the use of antibiotics may prevent SBP.[3]
SBP is present in about 15% of people admitted to hospital due to cirrhosis.[3] It has a high risk of death, with 30% dead at one month and 60% dead at a year.[3] The condition was first formally described by Harold O. Conn in 1964.[6] Those at risk of SBP may also develop spontaneous fungal peritonitis (SFP).[7]
Signs and symptoms

Symptoms of spontaneous bacterial peritonitis (SBP) include fevers, chills, nausea, vomiting, abdominal pain and tenderness, general malaise, altered mental status, and worsening ascites.[8] Thirteen percent of patients have no signs or symptoms.[9] In cases of acute or chronic liver failure SBP is one of the main triggers for hepatic encephalopathy, and where there is no other clear causal indication for this, SBP may be suspected.[10]
These symptoms can also be the same for a spontaneous fungal peritonitis (SFP) and therefore make a differentiation difficult. Delay of diagnosis can delay antifungal treatment and lead to a higher mortality rate.[7]
Causes
SBP is most commonly caused by gram-negative E. coli, followed by Klebsiella. Common gram-positive bacteria identified include species of Streptococcus, Staphylococcus, and Enterococcus.[11] The percentage of gram-positive bacteria responsible has been increasing.[5][11]
A spontaneous fungal infection can often follow a spontaneous bacterial infection that has been treated with antibiotics.[7] The use of antibiotics can result in an excessive growth of fungi in the gut flora which can then translocate into the peritoneal cavity.[12][7] Although fungi are much larger than bacteria, the increased intestinal permeability resulting from advanced cirrhosis makes their translocation easier.[7] SFP is mostly caused by species of Candida and most commonly by Candida albicans.[12]
Pathophysiology
H2 antagonists and proton-pump inhibitors are medications that decrease or suppress the secretion of acid by the stomach. Their use in treating cirrhosis is associated with the development of SBP.[13][14][15] Bacterial translocation is thought to be the key mechanism for the development of SBP.[9][16] Small intestinal bacterial overgrowth which may be implicated in this translocation, is found in a large percentage of those with cirrhosis.[17] With respect to compromised host defenses, patients with severe acute or chronic liver disease are often deficient in complement and may also have malfunctioning of the neutrophilic and reticuloendothelial systems.[18]
As for the significance of ascitic fluid proteins, it was demonstrated that cirrhotic patients with ascitic protein concentrations below 1 g/dL were 10 times more likely to develop SBP than individuals with higher concentrations.[19] It is thought that the antibacterial, or opsonic, activity of ascitic fluid is closely correlated with the protein concentration.[20] Additional studies have confirmed the validity of the ascitic fluid protein concentration as the best predictor of the first episode of SBP.[18]
In nephrotic syndrome, SBP can frequently affect children but only very rarely can it affect adults.[21]
Diagnosis
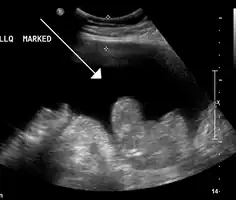
Infection of the peritoneum causes an inflammatory reaction with a subsequent increase in the number of neutrophils in the fluid.[3] Diagnosis is made by paracentesis (needle aspiration of the ascitic fluid); SBP is diagnosed if the fluid contains neutrophils at greater than 250 cells per mm3 (equals a cell count of 250 x106/L) fluid in the absence of another reason for this (such as inflammation of one of the internal organs or a perforation).[8][10] Often the number is greater than 500 cells/uL.[3]
The fluid is also cultured to identify bacteria. If the sample is sent in a plain sterile container, 40% of samples will identify an organism, while if the sample is sent in a bottle with culture medium, the sensitivity increases to 72–90%.[10]
Prevention
All people with cirrhosis might benefit from antibiotics (oral fluoroquinolone norfloxacin) if:
- Ascitic fluid protein <1.0 g/dL.[19] Patients with fluid protein <15 g/L and either Child-Pugh score of at least 9 or impaired renal function may also benefit.[22]
- Previous SBP[23]
People with cirrhosis admitted to the hospital should receive prophylactic antibiotics if:
- They have bleeding esophageal varices[24]
Studies on the use of rifaximin in cirrhotic, have suggested that its use may be effective in preventing spontaneous bacterial peritonitis.[25] [26]
Treatment
Antibiotics
Although there is no high-quality evidence, the third-generation cephalosporins are considered the standard empirical treatment for spontaneous bacterial peritonitis in people with cirrhosis.[27]
In practice, cefotaxime is often the agent of choice for treatment of SBP. After confirmation of SBP, hospital admission is usually advised for observation and intravenous antibiotic therapy.
Where there is a risk of kidney malfunction developing in a syndrome called hepatorenal syndrome, intravenous albumin is usually administered too. Paracentesis may be repeated after 48 hours to ensure control of infection. After recovery from a single episode of SBP, indefinite prophylactic antibiotics are recommended.[10]
Albumin
Intravenous albumin reduces the risk of kidney impairment and death.[28]
Prokinetics
The addition of a prokinetic drug to an antibiotic regimen reduces the incidence of spontaneous bacterial peritonitis possibly via decreasing small intestinal bacterial overgrowth.[29]
Epidemiology
Patients with ascites underwent routine paracentesis, the incidence of active SBP ranged from 10% to 27% at the time of hospital admission.[30]
History
Descriptions of SBP were first published in 1964 by Harold O. Conn.[31]
References
- ↑ Burleson, Samuel; Wang, Henry (8 March 2016). "Turbid Peritoneal Fluid". Western Journal of Emergency Medicine. 17 (2): 189–190. doi:10.5811/westjem.2016.1.29444. PMID 26973749.
- 1 2 3 "Spontaneous Bacterial Peritonitis (SBP) - Hepatic and Biliary Disorders". Merck Manuals Professional Edition. Archived from the original on 21 November 2021. Retrieved 22 January 2022.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 MacIntosh, T (1 March 2018). "Emergency Management of Spontaneous Bacterial Peritonitis - A Clinical Review". Cureus. 10 (3): e2253. doi:10.7759/cureus.2253. PMC 5929973. PMID 29721399.
- 1 2 3 Fernández, J; Bauer, TM; Navasa, M; Rodés, J (December 2000). "Diagnosis, treatment and prevention of spontaneous bacterial peritonitis". Baillière's Best Practice & Research. Clinical Gastroenterology. 14 (6): 975–990. doi:10.1053/bega.2000.0142. PMID 11139350.
- 1 2 Dever, JB; Sheikh, MY (June 2015). "Review article: spontaneous bacterial peritonitis--bacteriology, diagnosis, treatment, risk factors and prevention". Alimentary Pharmacology & Therapeutics (Review). 41 (11): 1116–31. doi:10.1111/apt.13172. PMID 25819304. S2CID 25620132.
- ↑ Conn, Harold O.; Rodes, Juan; Navasa, Miguel (24 March 2000). Spontaneous Bacterial Peritonitis: The Disease, Pathogenesis and Treatment. CRC Press. ISBN 978-0-8247-4654-4. Archived from the original on 23 January 2022. Retrieved 22 January 2022.
- 1 2 3 4 5 Shizuma, T (27 February 2018). "Spontaneous bacterial and fungal peritonitis in patients with liver cirrhosis: A literature review". World Journal of Hepatology. 10 (2): 254–266. doi:10.4254/wjh.v10.i2.254. PMC 5838444. PMID 29527261.
- 1 2 Lata J, Stiburek O, Kopacova M (November 2009). "Spontaneous bacterial peritonitis: a severe complication of liver cirrhosis". World J. Gastroenterol. 15 (44): 5505–10. doi:10.3748/wjg.15.5505. PMC 2785051. PMID 19938187. Archived from the original on 2016-03-15. Retrieved 2021-09-01.
- 1 2 Koulaouzidis, A; Bhat, S; Saeed, AA (7 March 2009). "Spontaneous bacterial peritonitis". World Journal of Gastroenterology. 15 (9): 1042–9. doi:10.3748/wjg.15.1042. PMC 2655193. PMID 19266595.
- 1 2 3 4 Moore KP, Aithal GP (October 2006). "Guidelines on the management of ascites in cirrhosis". Gut. 55 (Suppl 6): vi1–12. doi:10.1136/gut.2006.099580. PMC 1860002. PMID 16966752.
- 1 2 Fiore, Marco; Maraolo, Alberto Enrico; Gentile, Ivan; Borgia, Guglielmo; Leone, Sebastiano; Sansone, Pasquale; Passavanti, Maria Beatrice; Aurilio, Caterina; Pace, Maria Caterina (2017-10-28). "Current concepts and future strategies in the antimicrobial therapy of emerging Gram-positive spontaneous bacterial peritonitis". World Journal of Hepatology. 9 (30): 1166–1175. doi:10.4254/wjh.v9.i30.1166. ISSN 1948-5182. PMC 5666303. PMID 29109849.
- 1 2 Fiore, M; Leone, S (14 September 2016). "Spontaneous fungal peritonitis: Epidemiology, current evidence and future prospective". World Journal of Gastroenterology. 22 (34): 7742–7. doi:10.3748/wjg.v22.i34.7742. PMC 5016373. PMID 27678356.
- ↑ Gati GA, Deshpande A (2012). "Increased rate of spontaneous bacterial peritonitis among cirrhotic patients receiving pharmacologic acid suppression". Clinical Gastroenterology and Hepatology. 10 (4): 422–27. doi:10.1016/j.cgh.2011.11.019. PMID 22155557.
- ↑ Deshpande A, Pasupuleti V (2012). "Acid suppressive therapy is associated with spontaneous bacterial peritonitis in cirrhotic patients: a meta-analysis". Journal of Gastroenterology and Hepatology. 28 (2): 235–42. doi:10.1111/jgh.12065. PMID 23190338. S2CID 25099491.
- ↑ Bajaj JS, Zadvornova Y (2009). "Association of Proton Pump Inhibitor Therapy With Spontaneous Bacterial Peritonitis in Cirrhotic Patients With Ascites". American Journal of Gastroenterology. 104 (5): 1130–34. doi:10.1038/ajg.2009.80. PMID 19337238. S2CID 21179465.
- ↑ Căruntu, FA; Benea, L (March 2006). "Spontaneous bacterial peritonitis: pathogenesis, diagnosis, treatment". Journal of Gastrointestinal and Liver Diseases. 15 (1): 51–6. PMID 16680233.
- ↑ Maslennikov, R; Pavlov, C; Ivashkin, V (4 October 2018). "Small intestinal bacterial overgrowth in cirrhosis: systematic review and meta-analysis". Hepatology International. 12 (6): 567–576. doi:10.1007/s12072-018-9898-2. PMID 30284684. S2CID 52917740.
- 1 2 Alaniz C, Regal RE (April 2009). "Spontaneous Bacterial Peritonitis: A Review of Treatment Options". P T. 34 (4): 204–210. PMC 2697093. PMID 19561863.
- 1 2 Runyon BA (December 1986). "Low-protein-concentration ascitic fluid is predisposed to spontaneous bacterial peritonitis". Gastroenterology. 91 (6): 1343–6. doi:10.1016/0016-5085(86)90185-x. PMID 3770358.
- ↑ Runyon BA, Morrissey RL, Hoefs JC, Wyle FA (1985). "Opsonic activity of human ascitic fluid: a potentially important protective mechanism against spontaneous bacterial peritonitis". Hepatology. 5 (4): 634–7. doi:10.1002/hep.1840050419. PMID 4018735. S2CID 9665518.
- ↑ Ruiz, S; Soto, S; Rodado, R; Alcaraz, F; López Guillén, E (September 2007). "[Spontaneous bacterial peritonitis as form of presentation of idiophatic nephrotic syndrome in a black adult]". Anales de Medicina Interna. 24 (9): 442–4. doi:10.4321/s0212-71992007000900008. PMID 18198954.
- ↑ Fernández J, Navasa M, Planas R, et al. (2007). "Primary prophylaxis of spontaneous bacterial peritonitis delays hepatorenal syndrome and improves survival in cirrhosis". Gastroenterology. 133 (3): 818–24. doi:10.1053/j.gastro.2007.06.065. PMID 17854593.
- ↑ Grangé JD, Roulot D, Pelletier G, et al. (1998). "Norfloxacin primary prophylaxis of bacterial infections in cirrhotic patients with ascites: a double-blind randomized trial". J. Hepatol. 29 (3): 430–6. doi:10.1016/S0168-8278(98)80061-5. PMID 9764990.
- ↑ Chavez-Tapia, Norberto C.; Barrientos-Gutierrez, Tonatiuh; Tellez-Avila, Felix I.; Soares-Weiser, Karla; Uribe, Misael (2010-09-08). "Antibiotic prophylaxis for cirrhotic patients with upper gastrointestinal bleeding". The Cochrane Database of Systematic Reviews (9): CD002907. doi:10.1002/14651858.CD002907.pub2. ISSN 1469-493X. PMC 7138054. PMID 20824832.
- ↑ Fukui, H; Kawaratani, H; Kaji, K; Takaya, H; Yoshiji, H (2018). "Management of refractory cirrhotic ascites: challenges and solutions". Hepatic Medicine: Evidence and Research. 10: 55–71. doi:10.2147/HMER.S136578. PMC 6039068. PMID 30013405.
- ↑ Goel, A; Rahim, U; Nguyen, LH; Stave, C; Nguyen, MH (December 2017). "Systematic review with meta-analysis: rifaximin for the prophylaxis of spontaneous bacterial peritonitis". Alimentary Pharmacology & Therapeutics. 46 (11–12): 1029–1036. doi:10.1111/apt.14361. PMID 28994123.
- ↑ Chavez-Tapia, NC; Soares-Weiser, K; Brezis, M; Leibovici, L (21 January 2009). "Antibiotics for spontaneous bacterial peritonitis in cirrhotic patients". The Cochrane Database of Systematic Reviews (1): CD002232. doi:10.1002/14651858.CD002232.pub2. PMC 7100568. PMID 19160207.
- ↑ Salerno, F; Navickis, RJ; Wilkes, MM (February 2013). "Albumin infusion improves outcomes of patients with spontaneous bacterial peritonitis: a meta-analysis of randomized trials". Clinical gastroenterology and hepatology : the official clinical practice journal of the American Gastroenterological Association. 11 (2): 123-30.e1. doi:10.1016/j.cgh.2012.11.007. PMID 23178229.
- ↑ Hiyama, T.; Yoshihara, M.; Tanaka, S.; Haruma, K.; Chayama, K. (Apr 2009). "Effectiveness of prokinetic agents against diseases external to the gastrointestinal tract". J Gastroenterol Hepatol. 24 (4): 537–46. doi:10.1111/j.1440-1746.2009.05780.x. PMID 19220673.
- ↑ Runyon BA (1988). "Spontaneous bacterial peritonitis: an explosion of information". Hepatology. 8 (1): 171–5. doi:10.1002/hep.1840080131. PMID 3338704. S2CID 46406014.
- ↑ CONN HO (April 1964). "Spontaneous peritonitis and bacteremia in Laennec's cirrhosis caused by enteric organisms. A relatively common but rarely recognized syndrome". Ann. Intern. Med. 60 (4): 568–80. doi:10.7326/0003-4819-60-4-568. PMID 14138877.
External links
| Classification | |
|---|---|
| External resources |