Esophageal rupture
| Esophageal rupture | |
|---|---|
| Other names: Boerhaave syndrome, esophageal injury | |
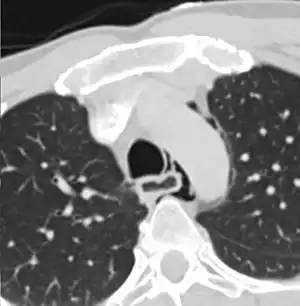 | |
| Axial CT image through the upper chest showing extraluminal air (pneumediastinum) surrounding the trachea and esophagus | |
| Specialty | Gastroenterology, general surgery |
| Symptoms | Chest pain, shortness of breath, fever, trouble swallowing[1] |
| Complications | Mediastinitis, sepsis[2][1] |
| Causes | Endoscopy, trauma, caustic ingestion, vomiting, seizures, abdominal trauma, compressed air injury, childbirth[3][4] |
| Risk factors | Esophagitis, alcoholism, eating in excess[3] |
| Diagnostic method | May be supported medical imaging or endoscopy[1] |
| Differential diagnosis | Aortic dissection, acute pancreatitis, heart attack, pneumothorax[3] |
| Treatment | Intravenous fluids, antibiotics, surgery[5] |
| Prognosis | High risk of death[3] |
| Frequency | Rare[2] |
Esophageal rupture, also known as Boerhaave syndrome, is a full thickness tear of the esophageal wall.[1] Symptoms generally include chest pain.[1] Other symptoms may include shortness of breath, fever, and trouble swallowing.[1] Complications can include mediastinitis and sepsis.[2][1]
Causes include endoscopy, trauma, caustic ingestion, vomiting, seizures, abdominal trauma, compressed air injury, and childbirth.[3][4] While in most cases the esophagus is previously normal, esophagitis and esophageal ulcers are risk factors.[3] Other risk factors include alcoholism and eating in excess.[3] Diagnosis may be supported by a chest X-ray, esophagogram, CT scan, or endoscopy.[1] A crackling sound may be heart in time with the heart beat.[5]
Treatment is with intravenous fluids, antibiotics such as piperacillin/tazobactam, and surgery when the lower esophagus is involved.[5] The risk of death is high and without treatment people may die within days.[3][5] Some injuries of the middle and upper esophagus may be managed without surgery.[4] Early diagnosis improves outcomes.[3]
Esophageal rupture is rare.[2] This condition was first documented by the 18th-century physician Herman Boerhaave, after whom it is named.[6][7] Some use the term "Boerhaave" only for those cases due to increased intra-esophageal pressure.[3] Mallory-Weiss syndrome is a much less severe condition in which only the mucosa tears.[6]
Signs and symptoms
The classic history of esophageal rupture is one of severe retching and vomiting followed by excruciating retrosternal chest and upper abdominal pain. Odynophagia, tachypnea, dyspnea, cyanosis, fever, and shock develop rapidly thereafter.
Physical examination is usually not helpful, particularly early in the course. Subcutaneous emphysema (crepitation) is an important diagnostic finding but is not very sensitive, being present in only 9 of 34 patients (27 percent) in one series. A pleural effusion may be detected.
Mackler's triad includes chest pain, vomiting, and subcutaneous emphysema, and while it is a classical presentation, it is only present in 14% of people.[8]
Pain can occasionally radiate to the left shoulder, causing physicians to confuse an esophageal perforation with a myocardial infarction.
It may also be audibly recognized as Hamman's sign.
Pathophysiology
Esophageal rupture, in Boerhaave syndrome is thought to be the result of a sudden rise in internal esophageal pressure produced during vomiting, as a result of neuromuscular incoordination causing failure of the cricopharyngeus muscle (a sphincter within the pharynx) to relax. As the intra-oesophageal pressure increases, the bolus within the oesophagus has nowhere to go superiorly (as the cricopharyngeus fails to relax) which causes the oesophagus to rupture. The syndrome is commonly associated with the consumption of excessive food and/or alcohol as well as eating disorders such as bulimia.
The most common anatomical location of the tear in Boerhaave syndrome is at left posterolateral wall of the lower third of the esophagus, 2–3 cm before the stomach.[9]
Currently, the most common cause of esophageal perforation is iatrogenic. However, iatrogenic perforations, while still constituting a serious medical condition, are easier to treat and less prone to complications, particularly mediastinitis and sepsis. This is because they usually do not involve contamination of the mediastinum with gastric contents.
Diagnosis
The diagnosis of Boerhaave's syndrome is suggested on the plain chest radiography and confirmed by chest CT scan. The initial plain chest radiograph is almost always abnormal in patients with Boerhaave's syndrome and usually reveals mediastinal or free peritoneal air as the initial radiologic manifestation. With cervical esophageal perforations, plain films of the neck show air in the soft tissues of the prevertebral space.
Hours to days later, pleural effusion(s) with or without pneumothorax, widened mediastinum, and subcutaneous emphysema are typically seen. CT scan may show esophageal wall edema and thickening, extraesophageal air, periesophageal fluid with or without gas bubbles, mediastinal widening, and air and fluid in the pleural spaces, retroperitoneum or lesser sac.
The diagnosis of esophageal perforation could also be confirmed by water-soluble contrast esophagram (Gastrografin), which reveals the location and extent of extravasation of contrast material. Although barium is superior in demonstrating small perforations, the spillage of barium sulfate into the mediastinal and pleural cavities can cause an inflammatory response and subsequent fibrosis and is therefore not used as the primary diagnostic study. If, however, the water-soluble study is negative, a barium study should be performed for better definition.
Endoscopy has no role in the diagnosis of spontaneous esophageal perforation. Both the endoscope and insufflation of air can extend the perforation and introduce air into the mediastinum.
Patients may also have a pleural effusion high in amylase (from saliva), low pH, and may contain particles of food.
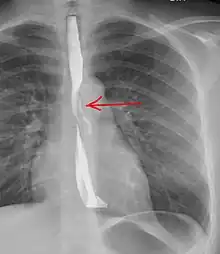
 Upright chest radiography showing mediastinal air adjacent to the aorta and tracking cephalad adjacent to the left common carotid artery. This patient presented to the Emergency department with severe chest pain after eating.
Upright chest radiography showing mediastinal air adjacent to the aorta and tracking cephalad adjacent to the left common carotid artery. This patient presented to the Emergency department with severe chest pain after eating. Sagittal remormatted CT image showing discontinutity in the wall of the posterolateral aspect of the distal esophagus
Sagittal remormatted CT image showing discontinutity in the wall of the posterolateral aspect of the distal esophagus
Differential diagnosis
Common misdiagnoses include myocardial infarction, pancreatitis, lung abscess, pericarditis, and spontaneous pneumothorax. If esophageal perforation is suspected, even in the absence of physical findings, chest xray, water soluble contrast radiographic studies of the esophagus and a CT scan should be promptly obtained. In most cases, non-operative management is administered based on radiological evidence contained in mediastinal collection.[10]
Treatment
With the exception of a few case reports describing survival without surgery,[11] the mortality of untreated Boerhaave syndrome is nearly 100%.[12] Its treatment includes immediate antibiotic therapy to prevent mediastinitis and sepsis, surgical repair of the perforation,[13] and if there is significant fluid loss it should be replaced with IV fluid therapy since oral rehydration is not possible. Even with early surgical intervention (within 24 hours) the risk of death is 25%.[14]
References
- 1 2 3 4 5 6 7 8 Bautz, B; Schneider, JI (May 2020). "High-Risk Chief Complaints I: Chest Pain-The Big Three (an Update)". Emergency medicine clinics of North America. 38 (2): 453–498. doi:10.1016/j.emc.2020.01.009. PMID 32336336.
- 1 2 3 4 Oguma, J; Ozawa, S (July 2015). "[Idiopathic and Iatrogenic Esophageal Rupture]". Kyobu geka. The Japanese journal of thoracic surgery. 68 (8): 701–5. PMID 26197919.
- 1 2 3 4 5 6 7 8 9 10 Turner, AR; Turner, SD (January 2021). "Boerhaave Syndrome". PMID 28613559.
{{cite journal}}: Cite journal requires|journal=(help) - 1 2 3 Mubang, RN; Sigmon, DF; Stawicki, SP (January 2021). "Esophageal Trauma". PMID 29261892.
{{cite journal}}: Cite journal requires|journal=(help) - 1 2 3 4 "Esophageal Rupture - Gastrointestinal Disorders". Merck Manuals Professional Edition. Archived from the original on 3 May 2021. Retrieved 2 May 2021.
- 1 2 "Boerhaave's syndrome". www.whonamedit.com. Archived from the original on 16 January 2020. Retrieved 2 May 2021.
- ↑ Boerhaave, Herman (1724). Atrocis, nec descripti prius, morbis historia: Secundum medicae artis leges conscripta [Bitter or the results were registered before the history of the disease. According to the written laws of medicine] (in Latin). Lugduni Batavorum; Ex officine Boutesteniana. OCLC 952706276.
{{cite book}}: CS1 maint: unrecognized language (link) - ↑ Bautz, B; Schneider, JI (May 2020). "High-Risk Chief Complaints I: Chest Pain-The Big Three (an Update)". Emergency medicine clinics of North America. 38 (2): 453–498. doi:10.1016/j.emc.2020.01.009. PMID 32336336.
- ↑ Korn, Owen; Oñate, Juan C.; López, René (2007). "Anatomy of the Boerhaave syndrome". Surgery. 141 (2): 222–8. doi:10.1016/j.surg.2006.06.034. PMID 17263979.
- ↑ Wong, Kenneth; Roy, Gerard (2006). "Oesophageal rupture arising as a complication of acute appendicitis in a child". The Medical Journal of Australia. 184 (11): 588. PMID 16768671. Archived from the original on 2011-04-11. Retrieved 2016-10-19.
- ↑ Boerhaave syndrome at eMedicine
- ↑ Curci, Joseph J.; Horman, Marc J. (1976). "Boerhaaveʼs Syndrome. The Importance of Early Diagnosis and Treatment". Annals of Surgery. 183 (4): 401–8. doi:10.1097/00000658-197604000-00013. PMC 1344212. PMID 1267496.
- ↑ Matsuda, Akihisa; Miyashita, Masao; Sasajima, Koji; Nomura, Tsutomu; Makino, Hiroshi; Matsutani, Takeshi; Katsuno, Akira; Sasaki, Junpei; Tajiri, Takashi (2006). "Boerhaave Syndrome Treated Conservatively Following Early Endoscopic Diagnosis: A Case Report". Journal of Nippon Medical School. 73 (6): 341–5. doi:10.1272/jnms.73.341. PMID 17220586.
- ↑ Jougon, J; Mcbride, T; Delcambre, F; Minniti, A; Velly, J (2004). "Primary esophageal repair for Boerhaave's syndrome whatever the free interval between perforation and treatment". European Journal of Cardio-Thoracic Surgery. 25 (4): 475–9. doi:10.1016/j.ejcts.2003.12.029. PMID 15037257.
External links
| Classification | |
|---|---|
| External resources |