Intermittent fasting

Intermittent fasting, also known as intermittent energy restriction, is any of various meal timing schedules that cycle between voluntary fasting (or reduced calorie intake) and non-fasting over a given period.[1][2][3] Methods of intermittent fasting include alternate-day fasting,[4] periodic fasting, and daily time-restricted feeding.[1][5]
Intermittent fasting may have similar effects to a calorie-restriction diet,[2] and has been studied in the 21st century as a practice to possibly reduce the risk of diet-related diseases, such as metabolic syndrome.[1][2][6][7][8] The American Heart Association stated in 2017 that intermittent fasting may produce weight loss, reduce insulin resistance, and lower the risk of cardiometabolic diseases, although its long-term sustainability is unknown.[2] A 2019 review concluded that intermittent fasting may help with obesity, insulin resistance, dyslipidemia, hypertension, and inflammation.[1]
Adverse effects of intermittent fasting have not been comprehensively studied, leading some academics to point out its risk as a dietary fad.[9] The US National Institute on Aging stated in 2018 that there is insufficient evidence to recommend intermittent fasting, and encourages speaking to one's healthcare provider about the benefits and risks before making any significant changes to one's eating pattern.[10]
Fasting exists in various religious practices, including Buddhism, Christianity, Hinduism, Islam, Jainism, and Judaism.[3][11][12]
History
Fasting is an ancient tradition, having been practiced by many cultures and religions over centuries.[9][13][14]
Therapeutic intermittent fasts for the treatment of obesity were investigated since at least 1915, with a renewed interest in the medical community in the 1960s after Bloom and his colleagues published an "enthusiastic report".[15] Intermittent fasts, or "short-term starvation periods", ranged from 1 to 14 days in these early studies.[16] This enthusiasm penetrated lay magazines, which prompted researchers and clinicians to caution about the use of intermittent fasts without medical monitoring.[17]
A type of periodic fasting known as the 5:2 diet was introduced by Michelle Harvie and Mark Mattson and popularized in the UK and Australia by Michael Mosley around 2012. It also became popular in Australia.[18][19][20]
Types
Three methods of intermittent fasting are time-restricted feeding, alternate-day fasting, and periodic fasting:[1][3][5][9][21][22]
- Time-restricted feeding involves eating only during a certain number of hours each day, often establishing a consistent daily pattern of caloric intake within an 8–12 hour time window. This schedule is thought to better align food intake with naturally occurring circadian rhythms relating to nutrient metabolism.[23][24][25] Some approaches further restrict the time window, such as the 16:8 diet (16 fasting hours cycled by 8 non-fasting hours), or the 20:4 diet (20 hours fasting with a 4-hour feeding window).[26]
- Alternate-day fasting involves alternating between a 24-hour "fast day" when the person eats less than 25% of usual energy needs, followed by a 24-hour non-fasting "feast day" period. It is the strictest form of intermittent fasting because there are more days of fasting per week.[2][5] There are two subtypes:[9][25]
- Complete alternate-day fasting (or total intermittent energy restriction), where no calories are consumed on fasting days.
- Modified alternate-day fasting (or partial intermittent energy restriction) which allows the consumption of up to 25% of daily calorie needs on fasting days instead of complete fasting. This is akin to alternating days with normal eating and days with a very-low-calorie diet.[27]
- Periodic fasting or whole-day fasting involves any period of consecutive fasting of more than 24 hours, such as the 5:2 diet where there are one or two fasting days per week, to the more extreme version with several days or weeks of fasting.[1] During the fasting days, consumption of approximately 500 to 700 calories, or about 25% of regular daily caloric intake, may be allowed instead of complete fasting.[1][2][5][25][28]
The science concerning intermittent fasting is preliminary and uncertain due to an absence of studies on its long term effects.[1][2][10][29][30] Preliminary evidence indicates that intermittent fasting may be effective for weight loss, may decrease insulin resistance and fasting insulin, and may improve cardiovascular and metabolic health, although the long term sustainability of these effects has not been studied.[1][2]
Research
A 2021 review found that moderate alternate-day fasting for two to six months was associated with reductions of body weight, body mass index, and cardiometabolic risk factors in overweight or obese adults.[31]
Body weight
There is limited evidence that intermittent fasting produces weight loss comparable to a calorie restricted diet.[6][7][32][33][34] Most studies on intermittent fasting in humans have observed weight loss, ranging from 2.5% to 9.9%.[35][36]
The reductions in body weight can be attributed to the loss of fat mass and some lean mass.[37][38] For time restricted eating the ratio of weight loss is 3:1 for fat mass to lean mass, respectively.[38] Alternate-day fasting does not affect lean body mass,[5][39] although one review found a small decrease.[40]
Alternate-day fasting improves cardiovascular and metabolic biomarkers similarly to a calorie restriction diet in people who are overweight, obese or have a metabolic syndrome.[6][8][22][28][41] As of 2021, it remains uncertain whether intermittent fasting could prevent cardiovascular disease.[42]
A 2021 review found that intermittent fasting may help people lose more weight than regular eating patterns, but was not different from energy restriction diets.[42]
Intermittent fasting has not been studied in children, elderly, or underweight people, and may be harmful in these populations.[6][8][10][43] Intermittent fasting is not recommended for people who are not overweight, and the long-term sustainability of intermittent fasting is unknown as of 2018.[10][44][45]
Other effects
Night-time eating is linked to impaired sleep quality.[25] Intermittent fasting is not recommended to treat cancer in France,[46][47] the United Kingdom,[48] or the United States,[49] although a few small-scale clinical studies suggest that it may reduce chemotherapy side effects.[50][51] Periodic fasting may have a minor effect on chronic pain and mood disorders.[52][53][54] In preliminary research, intermittent fasting has shown signs of reducing risk factors for certain disorders, including insulin resistance and cardiovascular disease.[31][28] Intermittent fasting does not affect bone health.[55]
Athletic performance does not benefit from intermittent fasting.[56] Overnight fasting before exercise increases lipolysis, but reduces performance in prolonged exercise (more than 60 min).[57][58]
Adverse effects
Reviews of preliminary clinical studies found that short-term intermittent fasting may produce minor adverse effects, such as continuous feelings of hunger, irritability, dizziness, nausea, headaches, and impaired thinking, although these effects disappear within a month from the fasting practice.[59][26] However, the data remains sparse, as most of the studies did not analyze adverse effects specifically.[6][33][60][61] A 2018 systematic review found no major adverse effects.[6] Intermittent fasting is not recommended for pregnant or breastfeeding women, growing children and adolescents, the elderly, or individuals with, or vulnerable to, eating disorders.[21]
Tolerance
Tolerance of a diet is a determinant of the potential effectiveness and maintenance of benefits obtained, such as weight loss or biomarker improvement.[33] A 2019 review found that drop-out rates varied widely from 2% to 38% for intermittent fasting, and from 0% to 50% for calorie restriction diet.[6]
Possible mechanisms
Preliminary research indicates that fasting may induce a transition through four states:
- The fed state or absorptive state during satiety, when the primary fuel source is glucose and body fat storage is active, lasting for about 4 hours;[62][63]
- The postabsorptive state, lasting for up to 18 hours, when glucagon is secreted and the body uses liver glucose reserves as a fuel source;[5][22][62]
- The fasted state, transitioning progressively to other reserves, such as fat, lactic acid, and alanine, as fuel sources, when the liver glucose reserves are depleted, occurring after 12 to 36 hours of continued fast;[63][64][65]
- The shift from preferential lipid synthesis and fat storage, to the mobilization of fat (in the form of free fatty acids), metabolized into fatty acid-derived ketones to provide energy.[22][63][66][67] Some authors call this transition the "metabolic switch".[1][22][68]
A 2019 review of weight-change interventions, including alternate day fasting, time-restricted feeding, exercise and overeating, found that body weight homeostasis could not precisely correct "energetic errors" – the loss or gain of calories – in the short-term.[69]
Another pathway for effects of meal timing on metabolism lies in the influence of the circadian rhythm over the endocrine system, especially on glucose metabolism and leptin.[70] Preliminary studies found that eating when melatonin is secreted – during darkness and commonly when sleeping at night – is associated with increased glucose levels in young healthy adults, and obesity and cardiovascular disorders in less healthy individuals.[71] Reviews on obesity prevention concluded that "meal timing appears as a new potential target in weight control strategies" and suggest that "timing and content of food intake, physical activity, and sleep may be modulated to counteract" circadian and metabolic genetic predispositions to obesity.[72][73]
Intermittent feeding
Other feeding schemes, such as hypocaloric feeding[74] and intermittent feeding, also called bolus feeding were under study.[75] A 2019 meta-analysis found that intermittent feeding may be more beneficial for premature infants, although better designed studies are required to devise clinical practices.[76] In adults, reviews have not found intermittent feeding to increase glucose variability or gastrointestinal intolerance.[77][78] A meta-analysis found intermittent feeding had no influence on gastric residual volumes and aspiration, pneumonia, mortality nor morbidity in people with a trauma, but increased the risk of diarrhea.[75][78]
Food production
Intermittent fasting, or "skip-a-day" feeding, is supposedly the most common feeding strategy for poultry in broiler breeder farms worldwide, as an alternative to adding bulky fibers to the diet to reduce growth. It is perceived as welfare-reducing and thus illegal in several European countries including Sweden. Intermittent fasting in poultry appears to increase food consumption but reduce appetitive behaviors such as foraging.[79]
Religious fasting
Intermittent fasting exists in some religious practices.[3][11] These include the Black Fast of Christianity (commonly practiced during Lent), Vrata (Hinduism), Ramadan (Islam), Fast Sunday (The Church of Jesus Christ of Latter-day Saints), Jain fasting, and Buddhist fasting.[3][11][12] Religious fasting practices may only require abstinence from certain foods or last for a short period of time and cause negligible effects.[11]
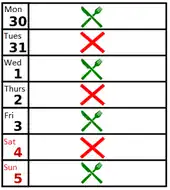
In Christianity, many adherents of Christian denominations including Catholics, Lutherans, Methodists, Anglicans, and the Orthodox, often observe the Friday Fast throughout the year, which commonly includes abstinence from meat.[80] Throughout the liturgical season of Lent (and especially on Ash Wednesday and Good Friday) in the Christian calendar, many Christians practice a form of intermittent fasting in which one can consume two collations and one full meal; others partake of the Black Fast, in which no food is consumed until sundown.[81][82]
In Buddhism, fasting is undertaken as part of the monastic training of Theravada Buddhist monks, who fast daily from noon to sunrise of the next day.[83] This daily fasting pattern may be undertaken by laypeople following the eight precepts.[84][83]
During Ramadan, Islamic practices are similar to intermittent fasting by not eating or drinking from dawn until sunset, while permitting food intake in the morning before dawn and in the evening after dusk for 30 days.[11][85][86] A meta-analysis on the health of Muslims during Ramadan shows significant weight loss during the fasting period of up to 1.51 kilograms (3.3 lb), but this weight was regained within about two weeks thereafter.[87] The analysis concluded that "Ramadan provides an opportunity to lose weight, but structured and consistent lifestyle modifications are necessary to achieve lasting weight loss."[87] One review found similarities between Ramadan and time-restricted feeding, with the main dissimilarity being the disallowance of water drinking with Islamic fasting.[88] In a 2020 review, Ramadan fasting caused a significant decrease in LDL cholesterol levels, and a slight decline in total cholesterol.[86]
A review of the metabolic effects of fasting showed that religious fasting proved to be beneficial in terms of "body weight and glycemia, cardiometabolic risk markers, and oxidative stress parameters", where animals, in the study, that followed a diet regimen consistent with that of religious fasting, were observed to have weight loss in addition to "lowered plasma levels of glucose, triacylglycerols, and insulin growth factor-1".[11] Negative effects of Ramadan fasting include increased risk of hypoglycemia in diabetics, as well as inadequate levels of certain nutrients.[11] Ramadan disallows fluids during the fasting period. This type of fasting would be hazardous for pregnant women, as it is associated with risks of inducing labor and causing gestational diabetes, although it does not appear to affect the child's weight.[89][90][91] For these reasons, pregnant women, as well as children who have not reached puberty, the elderly, those who are physically or mentally incapable of fasting, travelers, and breast-feeding mothers are often exempt from religious fasting — Ramadan being one example.[85]
Recommendations
United States
The American Heart Association (AHA) recommends intermittent fasting as an option for weight loss and calorie control as part of an "intentional approach to eating that focuses on the timing and frequency of meals and snacks as the basis of a healthier lifestyle and improved risk factor management".[2] For overweight people, fasting may be integrated into a wider dietary change, such as "placing snacks strategically before meals that might be associated with overeating", planning meals and snacks throughout the day to help manage hunger and control meal portions, and "promote consistent overnight fast periods".[2] The AHA noted that eating some food on a fast day (instead of a complete fast) produced the greatest weight loss when at least 4% weight loss was achieved by obese individuals.[2]
The American Diabetes Association "found limited evidence about the safety and/or effects of intermittent fasting on type 1 diabetes" and preliminary results of weight loss for type 2 diabetes, and so does not recommend any specific dietary pattern for the management of diabetes until more research is done, recommending instead that "health care providers should focus on the key factors that are common among the patterns".[29]
The National Institute on Aging stated that although intermittent fasting showed weight loss success in several studies on obese or overweight individuals, it does not recommend intermittent fasting for non-overweight individuals because of uncertainties about its effectiveness and safety, especially for older adults.[10]
New Zealand
The New Zealand's Ministry of Health considers that intermittent fasting can be advised by doctors to some people, except diabetics, stating that these "diets can be as effective as other energy-restricted diets, and some people may find them easier to stick to" but there are possible side effects during fasting days such as "hunger, low energy levels, light-headedness and poor mental functioning" and note that healthy food must be chosen on non-fasting days.[30][92]
United Kingdom
According to NHS Choices, people considering the 5:2 diet should first consult a physician, as fasting can sometimes be unsafe.[93][94] A news item in the Canadian Medical Association Journal expressed concern that promotional material for the 5:2 diet showed people eating high-calorie food, such as hamburgers and chips, and that this could encourage binge eating since the implication was that "if you fast two days a week, you can devour as much junk as your gullet can swallow during the remaining five days".[95] Binge eating following dietary restrictions has been observed in a post-war famine study, where nineteen prisoners of war were observed during their rehabilitation with unlimited access to food, and found they tended to engage in binge eating.[27]
Europe
Given the lack of advantage and the increased incidence of diarrhea, European guidelines do not recommend intermittent feeding for patients in Intensive Care Units.[75][78]
Usage trends
As of 2019, intermittent fasting was a common fad diet, attracting celebrity endorsements and public interest.[96]
UK and Australia
Intermittent fasting (specifically the 5:2 diet) was popularized by Michael Mosley) in the UK and Australia in 2012[97][98] after the BBC2 television Horizon documentary Eat, Fast and Live Longer.[99][93][100][20]
North America
In the United States, intermittent fasting became a fad in Silicon Valley, California.[101] It was the most popular diet in 2018, according to a survey by the International Food Information Council.[102][103]
Commercial activity
As of 2019, interest in intermittent fasting led some companies to commercialize diet coaching, dietary supplements, and full meal packages.[101][104] These companies were criticized for offering expensive products or services that were not backed by science.[104][105]
See also
- 2010s in food
- Healthy diet
- List of diets
- Sustainable diet
- Very-low-calorie diet or starvation diet
- Weight loss
References
- 1 2 3 4 5 6 7 8 9 10 de Cabo R, Mattson MP (December 2019). "Effects of Intermittent Fasting on Health, Aging, and Disease". The New England Journal of Medicine. 381 (26): 2541–2551. doi:10.1056/NEJMra1905136. PMID 31881139. S2CID 209498984.
- 1 2 3 4 5 6 7 8 9 10 11 St-Onge MP, Ard J, Baskin ML, Chiuve SE, Johnson HM, Kris-Etherton P, Varady K, et al. (American Heart Association Obesity Committee of the Council on Lifestyle and Cardiometabolic Health; Council on Cardiovascular Disease in the Young; Council on Clinical Cardiology; and Stroke) (February 2017). "Meal Timing and Frequency: Implications for Cardiovascular Disease Prevention: A Scientific Statement From the American Heart Association". Circulation. 135 (9): e96–e121. doi:10.1161/CIR.0000000000000476. PMC 8532518. PMID 28137935.
- 1 2 3 4 5 Patterson RE, Laughlin GA, LaCroix AZ, Hartman SJ, Natarajan L, Senger CM, et al. (August 2015). "Intermittent Fasting and Human Metabolic Health". Journal of the Academy of Nutrition and Dietetics. 115 (8): 1203–12. doi:10.1016/j.jand.2015.02.018. PMC 4516560. PMID 25857868.
- ↑ Trepanowski JF, Kroeger CM, Barnosky A, Klempel MC, Bhutani S, Hoddy KK, et al. (July 2017). "Effect of Alternate-Day Fasting on Weight Loss, Weight Maintenance, and Cardioprotection Among Metabolically Healthy Obese Adults: A Randomized Clinical Trial". JAMA Internal Medicine. 177 (7): 930–938. doi:10.1001/jamainternmed.2017.0936. PMC 5680777. PMID 28459931.
- 1 2 3 4 5 6 Tinsley GM, La Bounty PM (October 2015). "Effects of intermittent fasting on body composition and clinical health markers in humans". Nutrition Reviews. 73 (10): 661–74. doi:10.1093/nutrit/nuv041. PMID 26374764.
- 1 2 3 4 5 6 7 Cioffi I, Evangelista A, Ponzo V, Ciccone G, Soldati L, Santarpia L, et al. (December 2018). "Intermittent versus continuous energy restriction on weight loss and cardiometabolic outcomes: a systematic review and meta-analysis of randomized controlled trials". Journal of Translational Medicine (Systematic review). 16 (1): 371. doi:10.1186/s12967-018-1748-4. PMC 6304782. PMID 30583725.
- 1 2 Sainsbury A, Wood RE, Seimon RV, Hills AP, King NA, Gibson AA, Byrne NM (December 2018). "Rationale for novel intermittent dieting strategies to attenuate adaptive responses to energy restriction". Obesity Reviews. 19 (Suppl 1): 47–60. doi:10.1111/obr.12787. PMID 30511512. S2CID 54552826.
- 1 2 3 Harris L, Hamilton S, Azevedo LB, Olajide J, De Brún C, Waller G, et al. (February 2018). "Intermittent fasting interventions for treatment of overweight and obesity in adults: a systematic review and meta-analysis" (PDF). JBI Database of Systematic Reviews and Implementation Reports. 16 (2): 507–547. doi:10.11124/JBISRIR-2016-003248. PMID 29419624. S2CID 46780578. Archived (PDF) from the original on 2019-10-30. Retrieved 2019-10-23.
- 1 2 3 4 Hart K (2018). "Chapter 4.6 Fad diets and fasting for weight loss in obesity.". In Hankey C (ed.). Advanced nutrition and dietetics in obesity. Wiley. pp. 177–182. ISBN 9780470670767.
- 1 2 3 4 5 "Calorie restriction and fasting diets: What do we know?". National Institute on Aging, US National Institutes of Health. 2018-08-14. Archived from the original on 5 October 2019. Retrieved 29 September 2019.
- 1 2 3 4 5 6 7 Persynaki A, Karras S, Pichard C (March 2017). "Unraveling the metabolic health benefits of fasting related to religious beliefs: A narrative review". Nutrition. 35: 14–20. doi:10.1016/j.nut.2016.10.005. PMID 28241983.
- 1 2 Kannan S, Mahadevan S, Seshadri K, Sadacharan D, Velayutham K (2016). "Fasting practices in Tamil Nadu and their importance for patients with diabetes". Indian Journal of Endocrinology and Metabolism. 20 (6): 858–862. doi:10.4103/2230-8210.192921. PMC 5105573. PMID 27867892.
- ↑ Fung J (11 April 2015). "Fasting - A History". Intensive Dietary Management. Archived from the original on 5 November 2019. Retrieved 4 October 2019.
- ↑ Hicks C (13 April 2015). "Why fasting is now back in fashion". The Telegraph. Archived from the original on 16 January 2019. Retrieved 14 January 2019.
- ↑ Howard AN (1975). "Dietary Treatment of Obesity". Obesity: Its Pathogenesis And Management (Monograph). Springer Netherlands. pp. 123–153. doi:10.1007/978-94-011-7155-7_5. ISBN 978-94-011-7155-7.: 125
- ↑ Duncan GG (September 1964). "The Control of Obesity by Intermittent Fasts". Transactions of the American Clinical and Climatological Association (Review). 74 (5): 121–9. doi:10.1016/S0025-7125(16)33406-X. PMC 2249073. PMID 14047310.
- ↑ Dinning JS (October 1963). "Correction of Obesity by Fasting". Nutrition Reviews (Mini-review). 21 (10): 304–6. doi:10.1111/j.1753-4887.1963.tb07474.x. PMID 14069065.
- ↑ Mosley M (5 August 2012). "The power of intermittent fasting". BBC Health. Archived from the original on 16 February 2019. Retrieved 14 January 2019.
- ↑ "Horizon - Eat, Fast and Live Longer". BBC iPlayer. 6 August 2012. Archived from the original on 5 January 2019. Retrieved 14 January 2019.
- 1 2 Wilson P (10 February 2020). "What the science says about the 5:2 intermittent fasting diet". ABC Everyday. Australian Broadcasting Corporation. Retrieved 11 February 2021.
This story, which was originally written by Pamela Wilson and published by ABC Health and Wellbeing, has been reviewed by Dr Rosemary Stanton OAM, nutritionist and visiting fellow, School of Medical Sciences, University of NSW, and was updated in 2019. Posted 5 Feb 2020, updated 10 Feb 2020
- 1 2 "Diet Review: Intermittent Fasting for Weight Loss". The Nutrition Source. Harvard School of Public Health. 16 January 2018. Archived from the original on 11 October 2019. Retrieved 4 October 2019.
- 1 2 3 4 5 Anton SD, Moehl K, Donahoo WT, Marosi K, Lee SA, Mainous AG, et al. (February 2018). "Flipping the Metabolic Switch: Understanding and Applying the Health Benefits of Fasting". Obesity (Review). 26 (2): 254–268. doi:10.1002/oby.22065. PMC 5783752. PMID 29086496.
- ↑ Chaix, Amandine; Manoogian, Emily N.C.; Melkani, Girish C.; Panda, Satchidananda (21 August 2019). "Time-Restricted Eating to Prevent and Manage Chronic Metabolic Diseases". Annual Review of Nutrition. 39 (1): 291–315. doi:10.1146/annurev-nutr-082018-124320. PMC 6703924. PMID 31180809.
- ↑ von Bubnoff, Andreas (29 January 2021). "The when of eating: The science behind intermittent fasting". Knowable Magazine. doi:10.1146/knowable-012821-1. Retrieved 29 November 2021.
- 1 2 3 4 Patterson RE, Sears DD (August 2017). "Metabolic Effects of Intermittent Fasting". Annual Review of Nutrition. 37 (1): 371–393. doi:10.1146/annurev-nutr-071816-064634. PMID 28715993.
- 1 2 Cienfuegos, Sofia; Gabel, Kelsey; Kalam, Faiza; Ezpeleta, Mark; Wiseman, Eric; Pavlou, Vasiliki; Lin, Shuhao; Oliveira, Manoela Lima; Varady, Krista A. (September 2020). "Effects of 4- and 6-h Time-Restricted Feeding on Weight and Cardiometabolic Health: A Randomized Controlled Trial in Adults with Obesity". Cell Metabolism. 32 (3): 366–378.e3. doi:10.1016/j.cmet.2020.06.018. ISSN 1550-4131. PMID 32673591. S2CID 220609271.
- 1 2 Johnstone A (May 2015). "Fasting for weight loss: an effective strategy or latest dieting trend?". International Journal of Obesity (Review). 39 (5): 727–33. doi:10.1038/ijo.2014.214. PMID 25540982. S2CID 24033290.
- 1 2 3 Mattson MP, Longo VD, Harvie M (October 2017). "Impact of intermittent fasting on health and disease processes". Ageing Research Reviews. 39: 46–58. doi:10.1016/j.arr.2016.10.005. PMC 5411330. PMID 27810402.
- 1 2 Evert AB, Dennison M, Gardner CD, Garvey WT, Lau KH, MacLeod J, et al. (May 2019). "Nutrition Therapy for Adults With Diabetes or Prediabetes: A Consensus Report". Diabetes Care (Professional society guidelines). 42 (5): 731–754. doi:10.2337/dci19-0014. PMC 7011201. PMID 31000505.
- 1 2 Minister of Health NZ (2017). Clinical guidelines for weight management in New Zealand adults (National guidelines). ISBN 978-1-98-853916-4. Archived from the original on 2019-11-01. Retrieved 2019-11-01.
- 1 2 Patikorn, Chanthawat; Roubal, Kiera; Veettil, Sajesh K.; Chandran, Viji; Pham, Tuan; Lee, Yeong Yeh; Giovannucci, Edward L.; Varady, Krista A.; Chaiyakunapruk, Nathorn (2021-12-17). "Intermittent fasting and obesity-related health outcomes: An umbrella review of meta-analyses of randomized clinical trials". JAMA Network Open. 4 (12): e2139558. doi:10.1001/jamanetworkopen.2021.39558. ISSN 2574-3805. PMC 8683964. PMID 34919135.
- ↑ Davis CS, Clarke RE, Coulter SN, Rounsefell KN, Walker RE, Rauch CE, et al. (March 2016). "Intermittent energy restriction and weight loss: a systematic review". European Journal of Clinical Nutrition. 70 (3): 292–9. doi:10.1038/ejcn.2015.195. PMID 26603882. S2CID 24189275.
- 1 2 3 Freire R (January 2020). "Scientific evidence of diets for weight loss: Different macronutrient composition, intermittent fasting, and popular diets". Nutrition. 69: 110549. doi:10.1016/j.nut.2019.07.001. PMID 31525701. S2CID 198280773.
- ↑ Rynders, Corey A.; Thomas, Elizabeth A.; Zaman, Adnin; Pan, Zhaoxing; Catenacci, Victoria A.; Melanson, Edward L. (2019-10-14). "Effectiveness of Intermittent Fasting and Time-Restricted Feeding Compared to Continuous Energy Restriction for Weight Loss". Nutrients. 11 (10): 2442. doi:10.3390/nu11102442. ISSN 2072-6643. PMC 6836017. PMID 31614992.
- ↑ Ekmekcioglu C (21 October 2019). "Nutrition and longevity - From mechanisms to uncertainties". Critical Reviews in Food Science and Nutrition (Review). 60 (18): 3063–3082. doi:10.1080/10408398.2019.1676698. PMID 31631676. S2CID 204815279.
- ↑ Stockman MC, Thomas D, Burke J, Apovian CM (June 2018). "Intermittent Fasting: Is the Wait Worth the Weight?". Current Obesity Reports (Review). 7 (2): 172–185. doi:10.1007/s13679-018-0308-9. PMC 5959807. PMID 29700718.
Nearly all IF studies have resulted in some degree of weight loss, ranging from 2.5–9.9%, and associated fat mass loss.
- ↑ Fanti, Maura; Mishra, Amrendra; Longo, Valter D.; Brandhorst, Sebastian (2021-01-29). "Time-Restricted Eating, Intermittent Fasting, and Fasting-Mimicking Diets in Weight Loss". Current Obesity Reports. 10 (2): 70–80. doi:10.1007/s13679-021-00424-2. ISSN 2162-4968. PMID 33512641. S2CID 231747084.
- 1 2 Gabel, Kelsey; Cienfuegos, Sofia; Kalam, Faiza; Ezpeleta, Mark; Varady, Krista A. (2021-03-26). "Time-Restricted Eating to Improve Cardiovascular Health". Current Atherosclerosis Reports. 23 (5): 22. doi:10.1007/s11883-021-00922-7. ISSN 1523-3804. PMC 8218778. PMID 33772388.
- ↑ Alhamdan BA, Garcia-Alvarez A, Alzahrnai AH, Karanxha J, Stretchberry DR, Contrera KJ, et al. (September 2016). "Alternate-day versus daily energy restriction diets: which is more effective for weight loss? A systematic review and meta-analysis". Obesity Science & Practice. 2 (3): 293–302. doi:10.1002/osp4.52. PMC 5043510. PMID 27708846.
- ↑ Roman YM, Dominguez MC, Easow TM, Pasupuleti V, White CM, Hernandez AV (October 2019). "Effects of intermittent versus continuous dieting on weight and body composition in obese and overweight people: a systematic review and meta-analysis of randomized controlled trials". International Journal of Obesity. 43 (10): 2017–2027. doi:10.1038/s41366-018-0204-0. hdl:10757/624649. PMID 30206335. S2CID 52188900.
- ↑ Papamichou D, Panagiotakos DB, Itsiopoulos C (June 2019). "Dietary patterns and management of type 2 diabetes: A systematic review of randomised clinical trials". Nutrition, Metabolism, and Cardiovascular Diseases (Systematic review). 29 (6): 531–543. doi:10.1016/j.numecd.2019.02.004. PMID 30952576. S2CID 86497236.
- 1 2 Allaf M, Elghazaly H, Mohamed OG, Fareen MF, Zaman S, Salmasi AM, et al. (Cochrane Heart Group) (January 2021). "Intermittent fasting for the prevention of cardiovascular disease". The Cochrane Database of Systematic Reviews. 1 (3): CD013496. doi:10.1002/14651858.CD013496.pub2. PMC 8092432. PMID 33512717.
- ↑ Longo VD, Mattson MP (February 2014). "Fasting: molecular mechanisms and clinical applications". Cell Metabolism. 19 (2): 181–92. doi:10.1016/j.cmet.2013.12.008. PMC 3946160. PMID 24440038.
- ↑ Harris L, McGarty A, Hutchison L, Ells L, Hankey C (January 2018). "Short-term intermittent energy restriction interventions for weight management: a systematic review and meta-analysis". Obesity Reviews. 19 (1): 1–13. doi:10.1111/obr.12593. PMID 28975722. S2CID 23760594.
- ↑ Headland M, Clifton PM, Carter S, Keogh JB (June 2016). "Weight-Loss Outcomes: A Systematic Review and Meta-Analysis of Intermittent Energy Restriction Trials Lasting a Minimum of 6 Months". Nutrients. 8 (6): 354. doi:10.3390/nu8060354. PMC 4924195. PMID 27338458.
- ↑ "Réseau NACRe - Réseau National Alimentation Cancer Recherche - Rapport NACRe jeûne regimes restrictifs cancer 2017". www6.inra.fr (in French). November 2017. Archived from the original on 20 September 2018. Retrieved 19 September 2018.
- ↑ Régime et évolution d'un cancer. Rev Prescrire. 1 October 2018. p. 773. Archived from the original on 6 October 2019. Retrieved 6 October 2019.
- ↑ "No proof 5:2 diet prevents cancer". nhs.uk. 3 October 2018. Archived from the original on 17 October 2019. Retrieved 17 October 2019.
- ↑ Russell J, Rovere A, eds. (2009). "Fasting". American Cancer Society Complete Guide to Complementary and Alternative Cancer Therapies (2nd ed.). American Cancer Society. ISBN 9780944235713.
- ↑ Smith LA, O'Flanagan CH, Bowers LW, Allott EH, Hursting SD (April 2018). "Translating Mechanism-Based Strategies to Break the Obesity-Cancer Link: A Narrative Review". Journal of the Academy of Nutrition and Dietetics (Narrative review). 118 (4): 652–667. doi:10.1016/j.jand.2017.08.112. PMC 5869082. PMID 29102513.
- ↑ O'Flanagan CH, Smith LA, McDonell SB, Hursting SD (May 2017). "When less may be more: calorie restriction and response to cancer therapy". BMC Medicine (Mini-review). 15 (1): 106. doi:10.1186/s12916-017-0873-x. PMC 5442682. PMID 28539118.
- ↑ Brain K, Burrows TL, Rollo ME, Chai LK, Clarke ED, Hayes C, et al. (April 2019). "A systematic review and meta-analysis of nutrition interventions for chronic noncancer pain". Journal of Human Nutrition and Dietetics. 32 (2): 198–225. doi:10.1111/jhn.12601. PMID 30294938. S2CID 52933736.
- ↑ Fond G, Macgregor A, Leboyer M, Michalsen A (October 2013). "Fasting in mood disorders: neurobiology and effectiveness. A review of the literature" (PDF). Psychiatry Research. 209 (3): 253–8. doi:10.1016/j.psychres.2012.12.018. PMID 23332541. S2CID 39700065. Archived (PDF) from the original on 2019-04-30. Retrieved 2019-10-23.
- ↑ Michalsen A (April 2010). "Prolonged fasting as a method of mood enhancement in chronic pain syndromes: a review of clinical evidence and mechanisms". Current Pain and Headache Reports. 14 (2): 80–7. doi:10.1007/s11916-010-0104-z. PMID 20425196. S2CID 23707195.
- ↑ Veronese N, Reginster JY (June 2019). "The effects of calorie restriction, intermittent fasting and vegetarian diets on bone health". Aging Clinical and Experimental Research. 31 (6): 753–758. doi:10.1007/s40520-019-01174-x. PMID 30903600. S2CID 85456777.
- ↑ Levy E, Chu T (July 2019). "Intermittent Fasting and Its Effects on Athletic Performance: A Review". Current Sports Medicine Reports. 18 (7): 266–269. doi:10.1249/JSR.0000000000000614. PMID 31283627. S2CID 195828287.
- ↑ Vieira AF, Costa RR, Macedo RC, Coconcelli L, Kruel LF (October 2016). "Effects of aerobic exercise performed in fasted v. fed state on fat and carbohydrate metabolism in adults: a systematic review and meta-analysis". The British Journal of Nutrition (Meta-analysis). 116 (7): 1153–1164. doi:10.1017/S0007114516003160. PMID 27609363. S2CID 25607885. Lay summary.
{{cite journal}}: Cite uses deprecated parameter|lay-url=(help) - ↑ Aird TP, Davies RW, Carson BP (May 2018). "Effects of fasted vs fed-state exercise on performance and post-exercise metabolism: A systematic review and meta-analysis". Scandinavian Journal of Medicine & Science in Sports (Meta-analysis). 28 (5): 1476–1493. doi:10.1111/sms.13054. hdl:10344/6776. PMID 29315892. S2CID 4962378.
- ↑ de Cabo R, Mattson MP (December 2019). "Effects of Intermittent Fasting on Health, Aging, and Disease". The New England Journal of Medicine. 381 (26): 2541–2551. doi:10.1056/NEJMra1905136. PMID 31881139. S2CID 209498984.
- ↑ Horne BD, Muhlestein JB, Anderson JL (August 2015). "Health effects of intermittent fasting: hormesis or harm? A systematic review". The American Journal of Clinical Nutrition. 102 (2): 464–70. doi:10.3945/ajcn.115.109553. PMID 26135345.
- ↑ "Top diets review". nhs.uk. 26 April 2018. Archived from the original on 5 August 2019. Retrieved 6 October 2019.
- 1 2 Monnier L, Colette C, Lapinski H, Boniface H (April 2004). "Self-monitoring of blood glucose in diabetic patients: from the least common denominator to the greatest common multiple". Diabetes & Metabolism (Mini-review). Elsevier Masson. 30 (2): 113–9. doi:10.1016/S1262-3636(07)70097-6. PMID 15223983. Archived from the original on 8 November 2019. Retrieved 8 November 2019.
- 1 2 3 Drăgoi CM (10 July 2019). "Insights into Chrononutrition: The Innermost Interplay Amongst Nutrition, Metabolism and the Circadian Clock, in the Context of Epigenetic Reprogramming". Farmacia. 67 (4): 557–571. doi:10.31925/farmacia.2019.4.2. S2CID 199075075.
- ↑ Cahill GF (August 2006). "Fuel metabolism in starvation". Annual Review of Nutrition (Narrative Review). 26 (1): 1–22. doi:10.1146/annurev.nutr.26.061505.111258. PMID 16848698.
- ↑ Renold AE (1965). "Section 5: Adipose Tissue". Handbook of Physiology: a Critical, Comprehensive Presentation of Physiological Knowledge and Concepts. American Physiological Society.
- ↑ Lechner K, von Schacky C, McKenzie AL, Worm N, Nixdorff U, Lechner B, et al. (March 2020). "Lifestyle factors and high-risk atherosclerosis: Pathways and mechanisms beyond traditional risk factors". European Journal of Preventive Cardiology. 27 (4): 394–406. doi:10.1177/2047487319869400. PMC 7065445. PMID 31408370.
- ↑ Zubrzycki A, Cierpka-Kmiec K, Kmiec Z, Wronska A (October 2018). "The role of low-calorie diets and intermittent fasting in the treatment of obesity and type-2 diabetes". Journal of Physiology and Pharmacology (Review). 69 (5). doi:10.26402/jpp.2018.5.02. PMID 30683819.
- ↑ Mattson MP, Moehl K, Ghena N, Schmaedick M, Cheng A (February 2018). "Intermittent metabolic switching, neuroplasticity and brain health". Nature Reviews. Neuroscience (Review). 19 (2): 63–80. doi:10.1038/nrn.2017.156. PMC 5913738. PMID 29321682.
- ↑ Levitsky DA, Sewall A, Zhong Y, Barre L, Shoen S, Agaronnik N, et al. (February 2019). "Quantifying the imprecision of energy intake of humans to compensate for imposed energetic errors: A challenge to the physiological control of human food intake". Appetite. 133: 337–343. doi:10.1016/j.appet.2018.11.017. PMID 30476522. S2CID 53712116.
- ↑ Rüger, M; Scheer, FA (December 2009). "Effects of circadian disruption on the cardiometabolic system". Reviews in Endocrine and Metabolic Disorders. 10 (4): 245–60. doi:10.1007/s11154-009-9122-8. PMID 19784781.
- ↑ Manoogian, ENC; Chaix, A; Panda, S (December 2019). "When to Eat: The Importance of Eating Patterns in Health and Disease". Journal of Biological Rhythms. 34 (6): 579–581. doi:10.1177/0748730419892105. PMID 31813351.
- ↑ Beccuti, G; Monagheddu, C; Evangelista, A; Ciccone, G; Broglio, F; Soldati, L; Bo, S (November 2017). "Timing of food intake: Sounding the alarm about metabolic impairments? A systematic review". Pharmacological Research. 125 (Pt B): 132–141. doi:10.1016/j.phrs.2017.09.005. PMID 28928073.
- ↑ Covassin, N; Singh, P; Somers, VK (November 2016). "Keeping Up With the Clock: Circadian Disruption and Obesity Risk". Hypertension. 68 (5): 1081–1090. doi:10.1161/HYPERTENSIONAHA.116.06588. PMID 27620394.
- ↑ Marik PE, Hooper MH (March 2016). "Normocaloric versus hypocaloric feeding on the outcomes of ICU patients: a systematic review and meta-analysis". Intensive Care Medicine. 42 (3): 316–323. doi:10.1007/s00134-015-4131-4. PMID 26556615. S2CID 37653149.
- 1 2 3 Singer P, Blaser AR, Berger MM, Alhazzani W, Calder PC, Casaer MP, et al. (February 2019). "ESPEN guideline on clinical nutrition in the intensive care unit" (PDF). Clinical Nutrition. 38 (1): 48–79. doi:10.1016/j.clnu.2018.08.037. PMID 30348463. S2CID 53036546. Archived (PDF) from the original on 2020-05-08. Retrieved 2020-02-17.
- ↑ Wang Y, Zhu W, Luo BR (May 2020). "Continuous feeding versus intermittent bolus feeding for premature infants with low birth weight: a meta-analysis of randomized controlled trials". European Journal of Clinical Nutrition (Meta-analysis). 74 (5): 775–783. doi:10.1038/s41430-019-0522-x. PMC 7222868. PMID 31659243. S2CID 204948008.
- ↑ Bear DE, Hart N, Puthucheary Z (August 2018). "Continuous or intermittent feeding: pros and cons". Current Opinion in Critical Care (Review). 24 (4): 256–261. doi:10.1097/MCC.0000000000000513. PMID 29877877. S2CID 46984630.
- 1 2 3 Van Dyck L, Casaer MP (August 2019). "Intermittent or continuous feeding: any difference during the first week?". Current Opinion in Critical Care (Meta-analysis). 25 (4): 356–362. doi:10.1097/MCC.0000000000000617. PMID 31107308. S2CID 159039594.
- ↑ Lindholm C (2019). Intermittent fasting in chickens: Physiological mechanisms and welfare implications for broiler breeders. Linköping University Electronic Press. ISBN 978-91-7685-018-3.
- ↑ Boyers L (2019). Intermittent Fasting Basics: Your Guide to the Essentials of Intermittent Fasting—and How It Can Work for You!. Simon and Schuster. p. 19. ISBN 978-1-5072-1056-7.
- ↑ "Fasting Guidelines" (PDF). Lutheran Church–Missouri Synod. 2016. Archived (PDF) from the original on 17 March 2018. Retrieved 17 March 2018.
- ↑ Stravinskas PM, Shaw RB (1 September 1998). Our Sunday Visitor's Catholic Encyclopedia. Our Sunday Visitor. ISBN 9780879736699.
The so-called black fast refers to a day or days of penance on which only one meal is allowed, and that in the evening. The prescription of this type of fast not only forbids the partaking of meats but also of all dairy products, such as eggs, butter, cheese, and milk. Wine and other alcoholic beverages are forbidden as well. In short, only bread, water, and vegetables form part of the diet for one following such a fast.
- 1 2 Johnston WM (2013-12-04). Encyclopedia of Monasticism. Routledge. p. 467. ISBN 9781136787164. Archived from the original on 2019-12-22. Retrieved 2019-06-26.
- ↑ Cottrell T, Zigmond D (2016-09-06). Buddha's Diet: The Ancient Art of Losing Weight Without Losing Your Mind. Running Press. pp. 26–27. ISBN 9780762460465.
- 1 2 Elnakib, Sara (12 April 2021). "Ramadan The Practice of Fasting". Eat Right: Academy of Nutrition and Dietetics. Retrieved 21 September 2021.
{{cite web}}: CS1 maint: url-status (link) - 1 2 Hoddy, Kristin K.; Marlatt, Kara L.; Çetinkaya, Hatice; Ravussin, Eric (July 2020). "Intermittent Fasting and Metabolic Health: From Religious Fast to Time‐Restricted Feeding". Obesity. 28 (S1): S29–S37. doi:10.1002/oby.22829. ISSN 1930-7381. PMC 7419159. PMID 32700827.
- 1 2 Sadeghirad B, Motaghipisheh S, Kolahdooz F, Zahedi MJ, Haghdoost AA (February 2014). "Islamic fasting and weight loss: a systematic review and meta-analysis". Public Health Nutrition. 17 (2): 396–406. doi:10.1017/S1368980012005046. PMID 23182306. S2CID 6162935.
- ↑ Ismail S, Manaf RA, Mahmud A (June 2019). "Comparison of time-restricted feeding and Islamic fasting: a scoping review". Eastern Mediterranean Health Journal (Review). World Health Organization Regional Office for the Eastern Mediterranean. 25 (4): 239–245. doi:10.26719/emhj.19.011. PMID 31210344. S2CID 96438878. Archived from the original on 2019-10-16. Retrieved 2019-10-16.
- ↑ Glazier JD, Hayes DJ, Hussain S, D'Souza SW, Whitcombe J, Heazell AE, Ashton N (October 2018). "The effect of Ramadan fasting during pregnancy on perinatal outcomes: a systematic review and meta-analysis". BMC Pregnancy and Childbirth. 18 (1): 421. doi:10.1186/s12884-018-2048-y. PMC 6202808. PMID 30359228.
- ↑ Balani J, Hyer S, Wagner M, Shehata H (2019). "Chapter 22: Obesity, Polycystic Ovaries and Impaired Reproductive Outcome". In Mahmood T, Arulkumaran S (eds.). Obesity. Journal of the American Association of Nurse Practitioners. Vol. 31. Elsevier. pp. 289–298. doi:10.1016/B978-0-12-416045-3.00022-4. ISBN 978-0-12-416045-3. PMID 30829975.
- ↑ Mirghani HM, Hamud OA (January 2006). "The effect of maternal diet restriction on pregnancy outcome". American Journal of Perinatology. 23 (1): 21–4. doi:10.1055/s-2005-923435. PMID 16450268.
- ↑ "Popular diets review". Ministry of Health NZ (National guidelines). February 2018. Archived from the original on 1 November 2019. Retrieved 1 November 2019.
- 1 2 Fleming M (27 January 2015). "Fasting facts: is the 5:2 diet too good to be true?". The Guardian. Archived from the original on 19 January 2018. Retrieved 18 January 2018.
- ↑ "News analysis: Does the 5:2 intermittent fasting diet work?". Health News. UK National Health Service - NHS Choices. May 2013. Archived from the original on 9 November 2016. Retrieved 23 November 2016.
- ↑ Collier R (June 2013). "Intermittent fasting: the science of going without". CMAJ. 185 (9): E363-4. doi:10.1503/cmaj.109-4451. PMC 3680567. PMID 23569168.
- ↑ Arbolario K (26 August 2019). "Intermittent Fasting: Exposing The Dangers Of This Fad Diet". Medical Daily. Archived from the original on 29 September 2019. Retrieved 30 September 2019.
- ↑ "How to diet". Live Well - NHS Choices. UK National Health Service. 9 December 2011. Archived from the original on 22 February 2014. Retrieved 10 February 2014.
- ↑ Trueland J (December 2013). "Fast and effective?". Nursing Standard. 28 (16–18): 26–7. doi:10.7748/ns2013.12.28.16.26.s28. PMID 24345130.
- ↑ Mosley M (5 September 2012). "Eat, Fast & Live Longer". Horizon. Episode 49x03. BBC. 2. Archived from the original on 28 February 2014. Retrieved 10 February 2014.
- ↑ "The UK's Hot New 5:2 Diet Craze Hits The U.S. - Weight Loss Miracle?". Forbes. 17 May 2013. Archived from the original on 13 February 2014. Retrieved 10 February 2014.
- 1 2 Solon O (2017-09-04). "The Silicon Valley execs who don't eat for days: 'It's not dieting, it's biohacking'". The Guardian. Archived from the original on 2018-11-05. Retrieved 2018-11-05.
- ↑ Kohok S (3 June 2019). "Why is intermittent fasting so popular?". Archived from the original on 2 July 2019. Retrieved 28 October 2019.
- ↑ "2018 Food & Health Survey" (PDF). foodinsight.org. International Food Information Council. 2018. Archived (PDF) from the original on 2020-01-03. Retrieved 2019-10-28.
- 1 2 Giles T (24 April 2018). "Silicon Valley wants to cash in on fasting". Bloomberg News. Archived from the original on 25 April 2020. Retrieved 8 November 2018.
- ↑ "Not so fast: Pros and cons of the newest diet trend". Harvard Health Publishing, Harvard University Medical School. 31 July 2019. Archived from the original on 24 August 2019. Retrieved 28 August 2019.
Further reading
- Brody JE (17 February 2020). "The benefits of intermittent fasting". The New York Times.
- Hall H (15 December 2015). "Intermittent fasting". Science-Based Medicine.
- "Cancer and Fasting / Calorie Restriction". UCSF Osher Center for Integrative Medicine.
- "A guide to 16:8 intermittent fasting". Medical News Today. 17 January 2020.