Marburg acute multiple sclerosis
| Marburg acute multiple sclerosis | |
|---|---|
| Other names: Acute multiple sclerosis, Marburg type | |
Marburg acute multiple sclerosis, also known as Marburg multiple sclerosis or acute fulminant multiple sclerosis, is considered one of the multiple sclerosis borderline diseases, which is a collection of diseases classified by some as MS variants and by others as different diseases. Other diseases in this group are neuromyelitis optica (NMO), Balo concentric sclerosis, and Schilder's disease.[1] The graver course is one form of malignant multiple sclerosis, with patients reaching a significant level of disability in less than five years from their first symptoms, often in a matter of months.[2]
Sometimes Marburg MS is considered a synonym for tumefactive MS,[3] but not for all authors.
Signs and symptoms
The clinical presentation of this condition is consistent with:[4]
- Headaches
- Vomiting
- Gait abnormality
- Hyperreflexia
Pathogenesis
Marburg MS has been reported to be closer to anti-MOG associated ADEM than to standard MS[5] It has been reported to appear sometimes post-partum[6]
MOG antibody‐associated demyelinating pseudotumor
Some anti-MOG cases satisfy the MS requirements (lesions disseminated in time and space) and are therefore traditionally considered MS cases. After the discovery of the anti-MOG disease this classification is into revision.[7]
Diagnosis
It took its name from Otto Marburg. It can be diagnosed in vivo with an MRI scan.[8] If Marburg disease occurs in the form of a single large lesion, it can be radiologically indistinguishable from a brain tumor or abscess. It is usually lethal, but it has been found to be responsive to Mitoxantrone[9] and Alemtuzumab,[10] and it has also been responsive to autologous stem cell transplantation.[11] Recent evidence shows that Marburg's presents a heterogeneous response to medication, as does standard MS.[12]
Treatment
Historically, acute MS was a fatal disease, with death occurring within a year of onset, often secondary to extensive brain stem demyelination. Treatment recommendations, based on anecdotes, include plasma exchange in conjunction with high-dose glucocorticoids(e.g., 1 to 2 g/day of methylprednisolone for 10 days followed by a slow taper). For patients who survive the acute attack, follow-up treatments include immunosuppression (monthly mitoxantrone or cyclophosphamide) either alone or in combination with IFN beta or GA.
Prognosis
Marburg variant of MS is an acute fulminant demyelinating process which in most cases progresses inexorably to death within 1–2 years.[13] However, there are some reports of Marburg MS reaching stability by three years.[14]
See also
References
- ↑ Fontaine, B. (2001). "Les formes frontières de sclérose en plaques" [Borderline forms of multiple sclerosis]. Revue Neurologique (in français). 157 (8–9 Pt 2): 929–34. PMID 11787357. Archived from the original on 2022-06-19. Retrieved 2021-01-13.
- ↑ Lublin, F. D.; Reingold, S. C. (1996). "Defining the clinical course of multiple sclerosis: Results of an international survey". Neurology. 46 (4): 907–11. doi:10.1212/WNL.46.4.907. PMID 8780061.
- ↑ "See explanation at". Archived from the original on 2013-07-19. Retrieved 2021-01-13.
- ↑ Rovira, Álex; Auger, Cristina; Rovira, Antoni (1 January 2016). "Chapter 21 - Other noninfectious inflammatory disorders". Handbook of Clinical Neurology. Elsevier. 135: 425–446. Archived from the original on 23 October 2021. Retrieved 17 June 2022.
- ↑ Todd A Hardy, Reddel, Barnett, Palace, Lucchinetti, Weinshenker, Atypical CNS inflammatory demyelinating disease, The lancet neurology, August, 2016, DOI:https://doi.org/10.1016/S1474-4422(16)30043-6 Archived 2022-06-19 at the Wayback Machine, Manuscript Number: THELANCETNEUROLOGY-D-16-00113R1 available at Archived 2021-09-21 at the Wayback Machine
- ↑ Eduardo Labat et al., An extremely aggressive case of Marburg's disease treated with high dose cyclophosphamide. A case report, Multiple Sclerosis and Related Disorders, Volume 31, June 2019, Pages 51-53, https://doi.org/10.1016/j.msard.2019.03.014
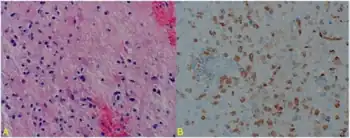
- ↑ Yaqing Shu Youming Long Shisi Wang Wanming Hu Jian Zhou Huiming Xu Chen Chen Yangmei Ou Zhengqi Lu Alexander Y. Lau Xinhua Yu Allan G. Kermode Wei Qiu, Brain histopathological study and prognosis in MOG antibody‐associated demyelinating pseudotumor, 08 January 2019, https://doi.org/10.1002/acn3.712
- ↑ Capello E, Mancardi GL (November 2004). "Marburg type and Balò's concentric sclerosis: rare and acute variants of multiple sclerosis". Neurol. Sci. 25 (Suppl): S361–3. doi:10.1007/s10072-004-0341-1. PMID 15727234. S2CID 12897512.
- ↑ Jeffery, Douglas R.; Lefkowitz, David S.; Crittenden, Jeffrey P. (2004). "Treatment of Marburg Variant Multiple Sclerosis with Mitoxantrone". Journal of Neuroimaging. 14 (1): 58–62. doi:10.1111/j.1552-6569.2004.tb00217.x. PMID 14748210. S2CID 30709186.
- ↑ Gormley KM, Zajicek JP (2006). "Alemtuzumab and craniotomy for severe acute demyelinating illness". 16th Meeting of the European Neurological Society. Archived from the original on 2007-10-07.
- ↑ Kimiskidis, VK; Sakellari, I.; Tsimourtou, V.; Kapina, V.; Papagiannopoulos, S.; Kazis, D.; Vlaikidis, N.; Anagnostopoulos, A.; Fassas, A. (2008). "Autologous stem-cell transplantation in malignant multiple sclerosis: A case with a favorable long-term outcome". Multiple Sclerosis Journal. 14 (2): 278–283. doi:10.1177/1352458507082604. PMID 17942513. S2CID 42334384.
- ↑ Leussink, V. I.; Lehmann, H. C.; Meyer Zu Hörste, G.; Hartung, H.-P.; Stüve, O.; Kieseier, B. C. (2008). "Rituximab induces clinical stabilization in a patient with fulminant multiple sclerosis not responding to natalizumab". Journal of Neurology. 255 (9): 1436–1438. doi:10.1007/s00415-008-0956-x. PMID 18685916. S2CID 38328163.
- ↑ Dan L. Longo; et al., eds. (2012). Harrison's principles of internal medicine (18th ed.). New York: McGraw-Hill. p. 3407. ISBN 9780071748896.
- ↑ Turatti, Marco; Gajofatto, Alberto; Rossi, Francesca; Vedovello, Marcella; Benedetti, Maria Donata (2010). "Long survival and clinical stability in Marburg's variant multiple sclerosis". Neurological Sciences. 31 (6): 807–811. doi:10.1007/s10072-010-0287-4. PMID 20461429. S2CID 37354295.
External links
| External resources |
|
|---|