Wellens' syndrome
| Wellens' syndrome | |
|---|---|
| Other names: Wellens syndrome, Wellens' sign, Wellens' warning, Wellens' waves, anterior descending T-wave syndrome | |
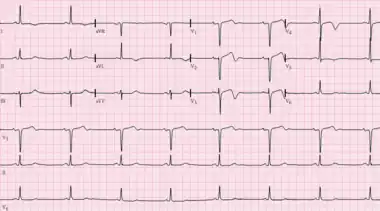 | |
| ECG of Wellens' syndrome. Note biphasic T-waves in leads V1-V4. | |
| Specialty | Cardiology |
| Symptoms | Angina that resolves[1] |
| Complications | Myocardial infarction[1] |
| Types | Type A, B[1] |
| Causes | Atherosclerosis, coronary vasospasm, Takotsubo cardiomyopathy[1] |
| Diagnostic method | ECG (deeply inverted or biphasic T waves in leads V2 and V3)[1] |
| Differential diagnosis | Brain injury, left ventricular hypertrophy (LVH), right bundle branch block (RBBB), hypertrophic cardiomyopathy (HOCM), pulmonary embolism, Brugada syndrome[1][2] |
| Treatment | Percutaneous coronary intervention (PCI)[1] |
| Medication | Aspirin, heparin[1] |
| Frequency | Relatively common[1] |
Wellens' syndrome is an electrocardiogram (ECG) pattern which often represents critical narrowing of the left anterior descending (LAD) coronary artery.[1] People often have chest pain, which resolves by the time they arrive at the hospital.[1] Complications include a 75% risk of myocardial infarction (MI) within weeks without appropriate treatment.[1]
The underlying mechanism is believed to involve rupture of an atherosclerotic plaque leading to blockage of the LAD, followed by clot breakdown before a MI occurs.[1] In about 90% of cases there is near blockage of the proximal LAD.[3] It can also occur in coronary vasospasm and Takotsubo cardiomyopathy.[1]
Diagnosis is based on an ECG showing deeply inverted or biphasic T waves in at least leads V2 and V3.[1][3] Other findings may include ST-segment elevation of less than 1 mm, no Q waves, and normal or slightly increased troponin.[1][3] When chest pain occurs, the ECG may appear normal.[1]
Treatment is by percutaneous coronary intervention (PCI).[1] Until this can be carried out, aspirin and heparin is typically used.[1] Wellens' syndrome is relatively common.[1] It was first described in 1982 by Hein Wellens.[4][5]
Diagnosis
The diagnosis is by ECG showing:
- Progressive symmetrical deep T wave inversion in leads V2 and V3
- Slope of inverted T waves generally at 60°-90°
- Little or no cardiac marker elevation
- Discrete or no ST segment elevation
- No loss of precordial R waves.
Types
Type A involves deeply inverted T waves while type B involves biphasic T waves in V2 and V3.[1] Over time, type A changes may turn into type B changes.[2]
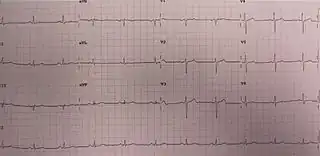 ECG in someone with Wellens' syndrome when having chest pain
ECG in someone with Wellens' syndrome when having chest pain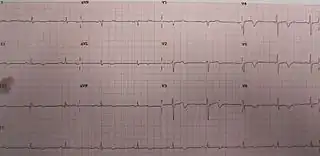 ECG of the same person when pain-free, note the biphasic T waves (type B) in leads V2 and V3
ECG of the same person when pain-free, note the biphasic T waves (type B) in leads V2 and V3 Angiogram, with video on the left showing critical (95%) stenosis of the proximal LAD in a person who had Wellens'; video on the right shows the same person after reperfusion
Angiogram, with video on the left showing critical (95%) stenosis of the proximal LAD in a person who had Wellens'; video on the right shows the same person after reperfusion
Differential diagnosis
Other conditions that may appear similarly include brain injury, left ventricular hypertrophy (LVH), right bundle branch block (RBBB), hypertrophic cardiomyopathy (HOCM), pulmonary embolism, and Brugada syndrome.[1][2] Additionally it may represent a normal ECG pattern in children.[2]
References
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 Miner, B; Grigg, WS; Hart, EH (January 2022). "Wellens Syndrome". PMID 29494097.
{{cite journal}}: Cite journal requires|journal=(help) - 1 2 3 4 Cadogan, Mike; Buttner, Robert; Buttner, Mike Cadogan and Robert (1 August 2020). "Wellens Syndrome". Life in the Fast Lane • LITFL. Archived from the original on 1 August 2021. Retrieved 28 July 2022.
- 1 2 3 Tzimas, Georgios; Antiochos, Panagiotis; Monney, Pierre; Eeckhout, Eric; Meier, David; Fournier, Stephane; Harbaoui, Brahim; Muller, Olivier; Schläpfer, Jürg (October 2019). "Atypical Electrocardiographic Presentations in Need of Primary Percutaneous Coronary Intervention". The American Journal of Cardiology. 124 (8): 1305–1314. doi:10.1016/j.amjcard.2019.07.027.
- ↑ PA-C, David Roberts, MSPAS, RN (31 December 2019). Mastering the 12-Lead EKG. Springer Publishing Company. p. 407. ISBN 978-0-8261-8194-7. Archived from the original on 28 July 2022. Retrieved 28 July 2022.
- ↑ de Zwaan, C; Bär FW; Wellens HJJ (April 1982). "Characteristic electrocardiographic pattern indicating a critical stenosis high in left anterior descending coronary artery in patients admitted because of impending myocardial infarction". American Heart Journal. 103 (4): 730–736. doi:10.1016/0002-8703(82)90480-X. PMID 6121481.
External links
- Further examples from Life in the Fastlane Archived 2021-08-01 at the Wayback Machine