Piperacillin
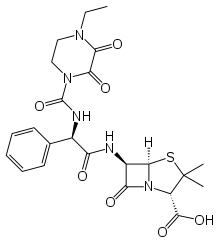
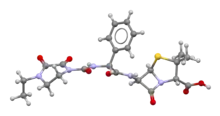
Piperacillin is a broad-spectrum β-lactam antibiotic of the ureidopenicillin class.[1] The chemical structure of piperacillin and other ureidopenicillins incorporates a polar side chain that enhances penetration into Gram-negative bacteria and reduces susceptibility to cleavage by Gram-negative beta lactamase enzymes. These properties confer activity against the important hospital pathogen Pseudomonas aeruginosa. Thus piperacillin is sometimes referred to as an "anti-pseudomonal penicillin".
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Pipracil |
| AHFS/Drugs.com | Consumer Drug Information |
| Pregnancy category |
|
| Routes of administration | Intravenous (IV), intramuscular (IM) |
| Drug class | β-lactam antibiotic |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | 0% oral |
| Protein binding | 30% |
| Metabolism | Largely not metabolized |
| Elimination half-life | 36–72 minutes |
| Excretion | 20% in bile, 80% unchanged in urine |
| Identifiers | |
IUPAC name
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.057.083 |
| Chemical and physical data | |
| Formula | C23H27N5O7S |
| Molar mass | 517.56 g·mol−1 |
| 3D model (JSmol) | |
SMILES
| |
InChI
| |
| (verify) | |
When used alone, piperacillin lacks strong activity against the Gram-positive pathogens such as Staphylococcus aureus, as the beta-lactam ring is hydrolyzed by the bacteria's beta-lactamase.[2]
It was patented in 1974 and approved for medical use in 1981.[3] Piperacillin is most commonly used in combination with the beta-lactamase inhibitor tazobactam (piperacillin/tazobactam), which enhances piperacillin's effectiveness by inhibiting many beta lactamases to which it is susceptible. However, the co-administration of tazobactam does not confer activity against MRSA, as penicillin (and most other beta lactams) do not avidly bind to the penicillin-binding proteins of this pathogen.[4] The World Health Organization classifies piperacillin as critically important for human medicine.[5]
Medical uses
Piperacillin is used almost exclusively in combination with the beta lactamase inhibitor tazobactam for the treatment of serious, hospital-acquired infections. This combination is among the most widely used drug therapies in United States non-federal hospitals, accounting for $388M in spending in spite of being a low-cost generic drug.[6]
Piperacillin-tazobactam is recommended as part of a three-drug regimen for the treatment of hospital-acquired pneumonia suspected as being due to infection by multi-drug resistant pathogens.[7] It is also one of several antibacterial drugs recommended for the treatment of infections known to be caused by anaerobic Gram-negative rods.[8]
Piperacillin-tazobactam is recommended by the National Institute for Health and Care Excellence as initial empiric treatment for people with suspected neutropenic sepsis.[9]
Piperacillin is used to treat patients diagnosed with various internal infections such as abdominal, bacteremia, gynecological, respiratory, and urinary, mainly caused by Pseudomonas aeruginosa and other infectious bacteria.[10][11][12] They are primarily used in current and former neutropenic patients, and patients with biliary tract infections. Other uses include applications in surgical infection prophylaxis; in biliary surgery, a single dose of piperacillin is administered intravenously to inhibit the development of acute cholangitis and prevent wound infections.[13] The combination of piperacillin and an aminoglycoside is commonly used to treat severe infections, but due to the incompatibilities in drug interaction, they are administered separately.[12][14]
Pneumonia
The piperacillin-tazobactam (piptaz) antibiotic commonly used with an aminoglycoside retains similar levels of drug safety and efficacy as other antibiotic combinations such as ceftazidime with the aminoglycoside tobramycin in the treatment of patients with hospital acquired pneumonia. In a clinical comparison primarily targeting patients not initially placed in intensive care units, piperacillin-tazobactam was found to produce higher clinical and microbiological rates of success.[15] By contrast, the drug efficacy of ceftazidime and piperacillin-tazobactam resulted in similar response rates (61.5% and 63.9 respectively) when tobramycin was added into both groups.[16] Identical evaluations are shown when compared to the imipenem and tobramycin combination, where the administration of piperacillin-tazobactam on patients (especially those under mechanical ventilation) was only consisted of a slightly higher response rate.[17][18]
Administration
Piperacillin is not absorbed orally, and must therefore be given by intravenous or intramuscular injection. It has been shown that the bactericidal actions of the drug do not increase with concentrations of piperacillin higher than 4-6 x MIC, which means that the drug is concentration-independent in terms of its actions. Piperacillin has instead shown to offer higher bactericidal activity when its concentration remains above the MIC for longer periods of time (50% time>MIC showing the highest activity). This higher activity present in continuous dosing has not been directly linked to clinical outcomes, but however does show promise of lowering possibility of resistance and decreasing mortality.[19]
Extending the time of piperacillin-tazobactam infusion allows the drugs to maintain the necessary concentrations needed within the body to prevent bacterial growth, enhancing bactericidal activity.[20] The studies supporting this theory generally administered ~3.375g of piperacillin-tazobactam every 8 hours during a 4-hour infusion, while for organisms with higher minimum inhibitory concentrations, ~4.5g of piperacillin-tazobactam was administered every 6 hours during a 3-hour infusion.[20]
The recommended doses provided by the BNFC for infants with hospital-acquired infections are 90 mg/kg every 8 hours for infants, a maximum of 4.5g every 6 hours for children, and 4.5g every 8 hours for children aged 12 and above. A dosage of 90 mg/kg every 6 hours is suggested for infants and children diagnosed with neutropenia.[21]
Adverse effects
Common side effects associated with the administration of piperacillin-tazobactam include:[22]
- Gastrointestinal: constipation, diarrhea, nausea, vomiting
- Dermatologic: erythema, pain, phlebitis, rash
- Neurologic: headaches, insomnia
Prolonged periods of piperacillin-tazobactam therapy have been associated with the potential development of hematologic adversities such as leukopenia (16.3%), neutropenia (10%), and eosinophilia (10%) in adult patients.[23] The combination of piperacillin-tazobactam with other antibiotics was found to be a major risk factor for leukopenia as well. Additionally, the chances of developing these illnesses increases in younger patients with fewer conditions, prolonging their time to recover.[23]
Other cases of adverse effects include instances of renal dysfunction, hepatitis, hyperactivity, anemia, abnormalities in coagulation, and hypokalemia.[10] Allergic reactions can be induced from the side chains of β-lactam antibiotics such as amoxicillin, or antibodies surrounding the nucleus of penicillin.[24]
Interactions
The combination of piperacillin and tazobactam, commonly branded as Zosyn, improves their overall bactericidal activity as amino-benzylpenicillins and ureidopencillins work synergistically with β-lactamase inhibitors.[25] Concurrent use or unregulated dosages of piperacillin results in increasing levels of piperacillin within the body, prolonging neuromuscular transmission blockages created by non-depolarizing muscle relaxants, and disruptions in urine tests for glucose.[10] Some compounds that may interfere with the bactericidal activity of piperacillin include chloramphenicol, macrolides, and sulfonamides.
Following two studies conducted in 1986 and 2006,[26][27] piperacillin was found to inhibit the removal of methotrexate in animal kidneys. Furthermore, in the presence of piperacillin-tazobactam, the decay time for methotrexate triples in comparison to the normal half-life, leaving the patient exposed to cytotoxic effects produced by the chemical agent.[26] While penicillin antibiotics generally work synergistically with aminoglycosides by enhancing their penetration of bacterial membranes, they can also work adversely by inactivating them.[22] A reformulation of ethylenediaminetetraacetic acid and piperacillin-tazobactam has produced results showing an increase in their affinity with amikacin and gentamicin in vitro, enabling the process of simultaneous Y-site infusion to occur. However, tobramycin was found to be incompatible as a combination through Y-site infusion.[22]
Pharmacology
Piperacillin irreversibly binds to the enzyme penicillin-binding proteins, inhibiting the biosynthesis of bacterial cell walls.[10]
Mechanism of action
As a β-lactam antibiotic, piperacillin inhibits penicillin-binding proteins, preventing the spread of bacteria and infections. Responsible for catalyzing the cross-linkage between peptidoglycan strands that protect the bacterial cell from osmotic rupture, penicillin-binding proteins are unique to bacterial organisms, where every known bacteria with a peptidoglycan cell wall consists of homologous sub-families.[24] By sharing a similar stereochemistry with the substrates that bind to penicillin-binding proteins, piperacillin is able to bind to serine residues found at the active site of the enzyme through the formation of a covalent complex, preventing other substrates from binding.[28] Moreover, this leads to the release of autolysins that break down the bacteria's cell wall.[29]
Some β-lactamase enzymes also consist of residue at their active site, enabling them to hydrolyze the β-lactam ring found within these antibiotics.[28] However, this hydrolytic activity is inhibited when piperacillin works in conjunction with tazobactam. Tazobactam binds to these enzymes to form a stable acyl-enzyme complex; similar to one formed during the hydrolysis of the β-lactam ring. Thus, protecting piperacillin from hydrolysis.[30]
The inclusion of a β-lactamase inhibitor does not always increase drug efficacy. Some bacteria may produce certain types of β-lactamase such as AmpC, which are intrinsically resistant to tazobactam.[31]
Mechanisms of resistance
A major mechanism of resistance against piperacillin-tazobactam is Gram-negative bacteria producing β-lactamases. Other currently known mechanisms include mutations in the active site of penicillin-binding proteins, changes in membrane efflux, or bacteria permeability.[31] Some enzymes, such as extended-spectrum β-lactamase (ESBL) have evolved from narrow-spectrum β-lactamases due to genetic mutations, increasing their capabilities to hydrolyze much broader spectrum penicillin. Due to prior conflicting reports on the drug's affinity with ESBL-producing bacteria, piperacillin-tazobactam treatment for such is not recommended.[31] Antibiotic resistance occurs sporadically, conferred by the continuous use of piperacillin-tazobactam in situations where it may prove to be ineffective, leading to cases where plasmid-mediated β-lactamases are being produced in bacteria that do not naturally produce it.[25]
Some Gram-positive bacteria penicillin-binding proteins such as Enterococcus faecium (PBP-5) or Staphylococcus aureus (PBP-2a) are intrinsically antibiotic resistant, consisting of relatively low affinity with piperacillin and therefore high resistance to piperacillin-tazobactam.[32][33] Furthermore, mutations in penicillin-binding proteins cause fluctuations in piperacillin affinity, whereas Streptococcus pneumoniae (PBP-2b) autolytic response is significantly reduced due to decreased affinity with piperacillin.[34] Although membrane permeability changes are less common as a mechanism of resistance, studies investigating Klebsiella pneumoniae have reported a correlation between decreased permeability of piperacillin and increased SHV-1 β-lactamase production.[35][36]
Pharmacokinetics
Piperacillin is generally available in their stable form as crystallized potassium or sodium salt, quickly losing bactericidal activity upon dissolution due to their short half-lives.[25] As the gastrointestinal tract does not absorb piperacillin and tazobactam, they are dissolved in a solution before being administered to a patient, through parenteral means.[31] Excreted through renal mechanisms like glomerular or tubular filtration as a component of urine, uncontrolled dosages of the drug can cause renal dysfunction and competitive inhibition of excretion, delaying piperacillin-tazobactam excretion, and endangering patients to drug exposure.[25]
Although the distribution of the drug remained the same, the half-life for elimination increased by three to five folds for patients diagnosed with renal dysfunction.[37] Measured by creatinine clearance (CrCl), patients with less than 30ml/min of clearance had significantly reduced levels of piperacillin/tazobactam excretion, measuring down to 35% of the initial dosage, while the area under the curve (AUC) for piperacillin increased by about three folds for those with less than 20ml/min.[37][38] A reduced dosage or alteration in the interval of administration is recommended for patients lying under 40ml/min of CrCl, depending on the severity of dysfunction.
Renal is the main pathway for drug elimination for both tazobactam and piperacillin in the body. While there are other non-renal means of drug elimination like Hepatobiliary excretion, they occur less frequently.[38] A substantial amount (~80%) of piperacillin found in urine when excreted through glomerular and tubular filtration is unmetabolized.[39] Tazobactam renal elimination may be significantly reduced through piperacillin interaction, dropping from 63.7% to 56.8% of the administered dose over a 24-hour period.[40] Piperacillin may be actively diffused through filtration into the biliary tract during renal clearing, indicated by a generally higher concentration of piperacillin than tazobactam in the bile.[41] The metabolites that make up the remaining percentage in the excreted urine are composed of M1 (inactive) and N-desethyl-piperacillin (active), formed from the division of β-lactam rings of both tazobactam and piperacillin respectively.[42]
Due to the hydrophilic nature of piperacillin-tazobactam, a volume distribution of ~15 L amounting to various sites (tissues) is desired, as hydrophilic compounds are not able to pass through plasma membranes as easily as hydrophobic compounds.[14][38] Concentrations often in the range of 90 MIC or above are located in specific areas including the gallbladder, lung, muscle, and skin, making up 16 - 85% of the plasma concentrations.[38] The concentration of piperacillin-tazobactam is especially lower in fatty tissue, making up less than 10% of the plasma concentrations.[43]
Pharmacodynamics
Compared to concentration dependent bactericidal antibiotics like aminoglycosides and fluoroquinolones, the antibacterial activity of β-lactam antibiotics are generally more time dependent.[44][45] Unlike the former, when piperacillin-tazobactam concentrations exceed minimum inhibitory concentrations (MIC) of a pathogen by five folds, the exponential relationship between concentration and activity begins to level off.[46] Otherwise, piperacillin-tazobactam bactericidal efficacy is shown to consist of a strong association with the duration of time the concentration exceeds minimum inhibitory concentrations (T>MIC).[45][47] When the T>MIC in the serum equates to 60 - 70% of the frequency for drug administration (dosing interval), maximal activity is achieved against Gram-negative bacteria, while for Gram-positive bacteria it occurs at around 40 - 50%.[44][46]
Within a 24-hour period in one clinical study, a T>MIC surpassing 60% was found for piperacillin-susceptible bacteria including Escherichia coli, Klebsiella pneumoniae and Staphylococcus aureus in two dosing regimes (4.5g every 8 hours and 3.375g every 8 hours).[48]
The evidence for this was obtained through Monte Carlo experiments procured by a special program (OPTAMA), where for several different scenarios (e.g. hospital acquired infections, secondary peritonitis, skin or soft tissue infections), the probability of attaining those figures were in the ranges of 85 - 95% and 90 - 89% respectively for the two regimes.[49][50][51] In addition, two similar dosing regimes (3.375g and 4.5g every 6 hours) both had lower chances of reaching the 90% T>MIC threshold compared to the 50% threshold against hospital acquired pneumonia pathogens.[52]
The optimization of piperacillin-tazobactam drug efficiency has been covered by various studies, limiting the focus down to two types of infusions; continuous and intermittent.[47][53] A comparison using the two administration methods under the same dosage regime of 13.5g per day highlighted no major differences when treating complex intra-abdominal infections.[19] Furthermore, a follow-up analyzation of this trial deduced that both methods of administration lead to higher concentrations compared to the MIC of the pathogens that were used.[54] Similar results are found in a study where a select number of β-lactam susceptible pathogens consisting of Enterococcus faecalis, Klebsiella pneumoniae and Citrobacter freundii were used to test a ~10g every 24 hour dosing interval for continuous infusion.[47][54]
Organisms with a piperacillin-tazobactam MIC values equal to 32 or less than 16ml/I lead to 50% T>MIC when extended-interval intermittent administrations under two different dosing intervals (8.1g and 6.75g every 12 hours) were used against them.[53] The pharmacodynamic target attainments corresponding to pathogens with MIC values of 16 mg/I are found to reach 92% when a more traditional 4 hour dosing regime is utilized to administer at irregular intervals.[55][56] One study using the Monte Carlo simulation produced contradicting results to the previous studies, deducing that inadequate pharmacodynamic targets were achieved (T>MIC > 50%) for similar ESBL-producing bacteria, applying to both continuous and high dosage intermittent infusion.[57]
Chemistry
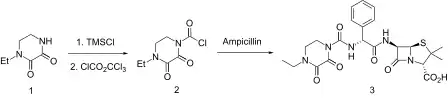
Derived from “the addition of a hydrophilic heterocyclic group to the α-amino group of ampicillin”,[22] the structure consists of a thiazolidine ring conjoined to a β-lactam ring contained within several ring compounds. The addition of this substituent increases the compound's affinity to penicillin-binding protein PBP-3, improving activity against Gram-negative bacteria, and thus broadening its spectrum of activity.[58] Susceptible β-lactamase producing bacteria such as Staphylococcus spp. or Haemophilus influenzae, the combination of tazobactam (which shares a similar structure to sulbactam, another β-lactamase inhibitor), and piperacillin significantly improves the stability of the drug against β-lactamases.[14]
References
- Tan JS, File TM (July 1995). "Antipseudomonal penicillins". The Medical Clinics of North America. 79 (4): 679–93. doi:10.1016/s0025-7125(16)30032-3. PMID 7791416.
- Hauser, AR Antibiotic Basics for Clinicians, 2nd Ed., Wolters Kluwer, 2013, pg 26-27
- Fischer J, Ganellin CR (2006). Analogue-based Drug Discovery. John Wiley & Sons. p. 491. ISBN 9783527607495.
- Zhanel GG, DeCorby M, Laing N, Weshnoweski B, Vashisht R, Tailor F, et al. (April 2008). "Antimicrobial-resistant pathogens in intensive care units in Canada: results of the Canadian National Intensive Care Unit (CAN-ICU) study, 2005-2006". Antimicrobial Agents and Chemotherapy. 52 (4): 1430–7. doi:10.1128/AAC.01538-07. PMC 2292546. PMID 18285482.
- World Health Organization (2019). Critically important antimicrobials for human medicine (6th revision ed.). Geneva: World Health Organization. hdl:10665/312266. ISBN 9789241515528.
- Schumock GT, Li EC, Suda KJ, Wiest MD, Stubbings J, Matusiak LM, et al. (May 2015). "National trends in prescription drug expenditures and projections for 2015". American Journal of Health-System Pharmacy. 72 (9): 717–36. doi:10.2146/ajhp140849. PMID 25873620.
- Mandell LA, Wunderink R, in Harrison's Principles of Internal Medicine 18th Ed., Chapter 257, pp. 2139-2141.
- Kasper DL, Cohen-Poradosu R, in Harrison's Principles of Internal Medicine 18th Ed., Chapter 164, pp. 1331-1339.
- National Collaborating Centre for Cancer (2012). "Neutropenic Sepsis: Prevention and Management of Neutropenic Sepsis in Cancer Patients". PMID 26065059.
{{cite journal}}: Cite journal requires|journal=(help) - Schlossberg D, Samuel R (2017-10-04). Antibiotics Manual. doi:10.1002/9781119220787. ISBN 9781119220787.
- Klastersky JA, ed. (1997). Febrile Neutropenia. Berlin, Heidelberg: Springer Berlin Heidelberg. doi:10.1007/978-3-642-60443-0. ISBN 978-3-540-61230-8. S2CID 34848917.
- "Antibiotics". Kucers' The Use of Antibiotics (Sixth ed.). CRC Press. 2010-10-29. p. 1. ISBN 978-0-340-92767-0.
- Westphal JF, Brogard JM (January 1999). "Biliary tract infections: a guide to drug treatment". Drugs. 57 (1): 81–91. doi:10.2165/00003495-199957010-00007. PMID 9951953. S2CID 46953299.
- Perry CM, Markham A (May 1999). "Piperacillin/tazobactam: an updated review of its use in the treatment of bacterial infections". Drugs. 57 (5): 805–43. doi:10.2165/00003495-199957050-00017. PMID 10353303. S2CID 209143536.
- Joshi M, Bernstein J, Solomkin J, Wester BA, Kuye O (March 1999). "Piperacillin/tazobactam plus tobramycin versus ceftazidime plus tobramycin for the treatment of patients with nosocomial lower respiratory tract infection. Piperacillin/tazobactam Nosocomial Pneumonia Study Group". The Journal of Antimicrobial Chemotherapy. 43 (3): 389–97. doi:10.1093/jac/43.3.389. PMID 10223595.
- Alvarez-Lerma F, Insausti-Ordeñana J, Jordá-Marcos R, Maraví-Poma E, Torres-Martí A, Nava J, et al. (March 2001). "Efficacy and tolerability of piperacillin/tazobactam versus ceftazidime in association with amikacin for treating nosocomial pneumonia in intensive care patients: a prospective randomized multicenter trial". Intensive Care Medicine. 27 (3): 493–502. doi:10.1007/s001340000846. PMID 11355117. S2CID 587826.
- Joshi M, Metzler M, McCarthy M, Olvey S, Kassira W, Cooper A (September 2006). "Comparison of piperacillin/tazobactam and imipenem/cilastatin, both in combination with tobramycin, administered every 6 h for treatment of nosocomial pneumonia". Respiratory Medicine. 100 (9): 1554–65. doi:10.1016/j.rmed.2006.01.004. PMID 16487695.
- Schmitt DV, Leitner E, Welte T, Lode H (June 2006). "Piperacillin/tazobactam vs imipenem/cilastatin in the treatment of nosocomial pneumonia--a double blind prospective multicentre study". Infection. 34 (3): 127–34. doi:10.1007/s15010-006-5020-0. PMID 16804655. S2CID 43485365.
- Lau WK, Mercer D, Itani KM, Nicolau DP, Kuti JL, Mansfield D, Dana A (November 2006). "Randomized, open-label, comparative study of piperacillin-tazobactam administered by continuous infusion versus intermittent infusion for treatment of hospitalized patients with complicated intra-abdominal infection". Antimicrobial Agents and Chemotherapy. 50 (11): 3556–61. doi:10.1128/AAC.00329-06. PMC 1635208. PMID 16940077.
- Kaufman SE, Donnell RW, Hickey WS (August 2011). "Rationale and evidence for extended infusion of piperacillin-tazobactam". American Journal of Health-System Pharmacy. 68 (16): 1521–6. doi:10.2146/ajhp100694. PMID 21817083.
- Wolf MF, Simon A (January 2009). "The use of piperacillin-tazobactam in neonatal and paediatric patients". Expert Opinion on Drug Metabolism & Toxicology. 5 (1): 57–69. doi:10.1517/17425250802614688. PMID 19236229. S2CID 72928444.
- Gin A, Dilay L, Karlowsky JA, Walkty A, Rubinstein E, Zhanel GG (June 2007). "Piperacillin-tazobactam: a beta-lactam/beta-lactamase inhibitor combination". Expert Review of Anti-Infective Therapy. 5 (3): 365–83. doi:10.1586/14787210.5.3.365. PMID 17547502. S2CID 68837323.
- Benli A, Şimşek-Yavuz S, Başaran S, Çağatay A, Özsüt H, Eraksoy H (November 2018). "Hematologic Adverse Effects of Prolonged Piperacillin-Tazobactam Use in Adults". Turkish Journal of Haematology. 35 (4): 290–295. doi:10.4274/tjh.2018.0127. PMC 6256823. PMID 29856362.
- Page MG (2012). "Beta-Lactam Antibiotics". In Dougherty TJ, Pucci MJ (eds.). Antibiotic Discovery and Development. Boston, MA: Springer US. pp. 79–117. doi:10.1007/978-1-4614-1400-1_3. ISBN 978-1-4614-1399-8.
- Dowling PM (July 2013). "Peptide antibiotics: polymyxins, glycopeptides, bacitracin, and fosfomycin.". In Giguère S, Prescott JF, Dowling PM (eds.). Antimicrobial Therapy in Veterinary Medicine. Wiley Blackwell. pp. 189–192. doi:10.1002/9781118675014. ISBN 9780470963029.
- Zarychanski R, Wlodarczyk K, Ariano R, Bow E (July 2006). "Pharmacokinetic interaction between methotrexate and piperacillin/tazobactam resulting in prolonged toxic concentrations of methotrexate". The Journal of Antimicrobial Chemotherapy. 58 (1): 228–30. doi:10.1093/jac/dkl196. PMID 16717053.
- Iven H, Brasch H (1986). "Influence of the antibiotics piperacillin, doxycycline, and tobramycin on the pharmacokinetics of methotrexate in rabbits". Cancer Chemotherapy and Pharmacology. 17 (3): 218–22. doi:10.1007/BF00256687. PMID 3742705. S2CID 25441195.
- Wilke MS, Lovering AL, Strynadka NC (October 2005). "Beta-lactam antibiotic resistance: a current structural perspective". Current Opinion in Microbiology. 8 (5): 525–33. doi:10.1016/j.mib.2005.08.016. PMID 16129657.
- Samaha-Kfoury JN, Araj GF (November 2003). "Recent developments in beta lactamases and extended spectrum beta lactamases". BMJ. 327 (7425): 1209–13. doi:10.1136/bmj.327.7425.1209. PMC 274061. PMID 14630759.
- Yang Y, Rasmussen BA, Shlaes DM (August 1999). "Class A beta-lactamases--enzyme-inhibitor interactions and resistance". Pharmacology & Therapeutics. 83 (2): 141–51. doi:10.1016/S0163-7258(99)00027-3. PMID 10511459.
- Hayashi Y, Roberts JA, Paterson DL, Lipman J (August 2010). "Pharmacokinetic evaluation of piperacillin-tazobactam". Expert Opinion on Drug Metabolism & Toxicology. 6 (8): 1017–31. doi:10.1517/17425255.2010.506187. PMID 20636224. S2CID 38067522.
- Rybkine T, Mainardi JL, Sougakoff W, Collatz E, Gutmann L (July 1998). "Penicillin-binding protein 5 sequence alterations in clinical isolates of Enterococcus faecium with different levels of beta-lactam resistance". The Journal of Infectious Diseases. 178 (1): 159–63. doi:10.1086/515605. PMID 9652435.
- Palmer SM, Rybak MJ (April 1997). "An evaluation of the bactericidal activity of ampicillin/sulbactam, piperacillin/tazobactam, imipenem or nafcillin alone and in combination with vancomycin against methicillin-resistant Staphylococcus aureus (MRSA) in time-kill curves with infected fibrin clots". The Journal of Antimicrobial Chemotherapy. 39 (4): 515–8. doi:10.1093/jac/39.4.515. PMID 9145825.
- Grebe T, Hakenbeck R (April 1996). "Penicillin-binding proteins 2b and 2x of Streptococcus pneumoniae are primary resistance determinants for different classes of beta-lactam antibiotics". Antimicrobial Agents and Chemotherapy. 40 (4): 829–34. doi:10.1128/AAC.40.4.829. PMC 163214. PMID 8849235.
- Rice LB, Carias LL, Hujer AM, Bonafede M, Hutton R, Hoyen C, Bonomo RA (February 2000). "High-level expression of chromosomally encoded SHV-1 beta-lactamase and an outer membrane protein change confer resistance to ceftazidime and piperacillin-tazobactam in a clinical isolate of Klebsiella pneumoniae". Antimicrobial Agents and Chemotherapy. 44 (2): 362–7. doi:10.1128/AAC.44.2.362-367.2000. PMC 89684. PMID 10639363.
- Poole K (September 2004). "Resistance to beta-lactam antibiotics". Cellular and Molecular Life Sciences. 61 (17): 2200–23. doi:10.1007/s00018-004-4060-9. PMID 15338052. S2CID 25289147.
- Aronoff GR, Sloan RS, Brier ME, Luft FC (1983). "The effect of piperacillin dose on elimination kinetics in renal impairment". European Journal of Clinical Pharmacology. 24 (4): 543–7. doi:10.1007/BF00609901. PMID 6222908. S2CID 262219.
- Sörgel F, Kinzig M (July 1994). "Pharmacokinetic characteristics of piperacillin/tazobactam". Intensive Care Medicine. 20 Suppl 3 (S3): S14-20. doi:10.1007/bf01745246. PMID 7962984. S2CID 27422742.
- Welling PG, Craig WA, Bundtzen RW, Kwok FW, Gerber AU, Madsen PO (June 1983). "Pharmacokinetics of piperacillin in subjects with various degrees of renal function". Antimicrobial Agents and Chemotherapy. 23 (6): 881–7. doi:10.1128/aac.23.6.881. PMC 184992. PMID 6225390.
- Wise R, Logan M, Cooper M, Andrews JM (June 1991). "Pharmacokinetics and tissue penetration of tazobactam administered alone and with piperacillin". Antimicrobial Agents and Chemotherapy. 35 (6): 1081–4. doi:10.1128/AAC.35.6.1081. PMC 284290. PMID 1656853.
- Westphal JF, Brogard JM, Caro-Sampara F, Adloff M, Blicklé JF, Monteil H, Jehl F (August 1997). "Assessment of biliary excretion of piperacillin-tazobactam in humans". Antimicrobial Agents and Chemotherapy. 41 (8): 1636–40. doi:10.1128/aac.41.8.1636. PMC 163977. PMID 9257733.
- Bryson HM, Brogden RN (March 1994). "Piperacillin/tazobactam. A review of its antibacterial activity, pharmacokinetic properties and therapeutic potential". Drugs. 47 (3): 506–35. doi:10.2165/00003495-199447030-00008. PMID 7514977. S2CID 209144038.
- Kinzig M, Sörgel F, Brismar B, Nord CE (September 1992). "Pharmacokinetics and tissue penetration of tazobactam and piperacillin in patients undergoing colorectal surgery". Antimicrobial Agents and Chemotherapy. 36 (9): 1997–2004. doi:10.1128/aac.36.9.1997. PMC 192425. PMID 1329637.
- Craig WA (January 1998). "Pharmacokinetic/pharmacodynamic parameters: rationale for antibacterial dosing of mice and men". Clinical Infectious Diseases. 26 (1): 1–10, quiz 11–2. doi:10.1086/516284. PMID 9455502.
- Turnidge JD (July 1998). "The pharmacodynamics of beta-lactams". Clinical Infectious Diseases. 27 (1): 10–22. doi:10.1086/514622. PMID 9675443.
- Burgess DS, Waldrep T (July 2002). "Pharmacokinetics and pharmacodynamics of piperacillin/tazobactam when administered by continuous infusion and intermittent dosing". Clinical Therapeutics. 24 (7): 1090–104. doi:10.1016/s0149-2918(02)80021-2. PMID 12182254.
- Buck C, Bertram N, Ackermann T, Sauerbruch T, Derendorf H, Paar WD (January 2005). "Pharmacokinetics of piperacillin-tazobactam: intermittent dosing versus continuous infusion". International Journal of Antimicrobial Agents. 25 (1): 62–7. doi:10.1016/j.ijantimicag.2004.08.012. PMID 15620828.
- Occhipinti DJ, Pendland SL, Schoonover LL, Rypins EB, Danziger LH, Rodvold KA (November 1997). "Pharmacokinetics and pharmacodynamics of two multiple-dose piperacillin-tazobactam regimens". Antimicrobial Agents and Chemotherapy. 41 (11): 2511–7. doi:10.1128/AAC.41.11.2511. PMC 164153. PMID 9371358.
- Ong CT, Kuti JL, Nicolau DP (2005). "Pharmacodynamic modeling of imipenem-cilastatin, meropenem, and piperacillin-tazobactam for empiric therapy of skin and soft tissue infections: a report from the OPTAMA Program". Surgical Infections. 6 (4): 419–26. doi:10.1089/sur.2005.6.419. PMID 16433606.
- Kotapati S, Kuti JL, Nicolau DP (2005). "Pharmacodynamic modeling of beta-lactam antibiotics for the empiric treatment of secondary peritonitis: a report from the OPTAMA program". Surgical Infections. 6 (3): 297–304. doi:10.1089/sur.2005.6.297. PMID 16201939.
- Maglio D, Kuti JL, Nicolau DP (July 2005). "Simulation of antibiotic pharmacodynamic exposure for the empiric treatment of nosocomial bloodstream infections: a report from the OPTAMA program". Clinical Therapeutics. 27 (7): 1032–42. doi:10.1016/j.clinthera.2005.07.004. PMID 16154482.
- Sun HK, Kuti JL, Nicolau DP (October 2005). "Pharmacodynamics of antimicrobials for the empirical treatment of nosocomial pneumonia: a report from the OPTAMA Program". Critical Care Medicine. 33 (10): 2222–7. doi:10.1097/01.CCM.0000181528.88571.9B. PMID 16215374. S2CID 27349260.
- Mattoes HM, Capitano B, Kim MK, Xuan D, Quintiliani R, Nightingale CH, Nicolau DP (May 2002). "Comparative pharmacokinetic and pharmacodynamic profile of piperacillin/tazobactam 3.375G Q4H and 4.5G Q6H". Chemotherapy. 48 (2): 59–63. doi:10.1159/000057663. PMID 12011536. S2CID 25721950.
- Li C, Kuti JL, Nightingale CH, Mansfield DL, Dana A, Nicolau DP (August 2005). "Population pharmacokinetics and pharmacodynamics of piperacillin/tazobactam in patients with complicated intra-abdominal infection". The Journal of Antimicrobial Chemotherapy. 56 (2): 388–95. doi:10.1093/jac/dki243. PMID 16002420.
- Lodise TP, Lomaestro BM, Drusano GL (September 2006). "Application of antimicrobial pharmacodynamic concepts into clinical practice: focus on beta-lactam antibiotics: insights from the Society of Infectious Diseases Pharmacists". Pharmacotherapy. 26 (9): 1320–32. doi:10.1592/phco.26.9.1320. PMID 16945055. S2CID 196393077.
- Lodise TP, Lomaestro B, Rodvold KA, Danziger LH, Drusano GL (December 2004). "Pharmacodynamic profiling of piperacillin in the presence of tazobactam in patients through the use of population pharmacokinetic models and Monte Carlo simulation". Antimicrobial Agents and Chemotherapy. 48 (12): 4718–24. doi:10.1128/AAC.48.12.4718-4724.2004. PMC 529233. PMID 15561849.
- Reese AM, Frei CR, Burgess DS (August 2005). "Pharmacodynamics of intermittent and continuous infusion piperacillin/tazobactam and cefepime against extended-spectrum beta-lactamase-producing organisms". International Journal of Antimicrobial Agents. 26 (2): 114–9. doi:10.1016/j.ijantimicag.2005.06.004. PMID 16029947.
- Essack SY (2001). "The Development of β-Lactam Antibiotics in Response to the Evolution of β-Lactamases 6". Pharmaceutical Research. 18 (10): 1391–1399. doi:10.1023/A:1012272403776. PMID 11697463. S2CID 34318096.