Achondroplasia
| Achondroplasia | |
|---|---|
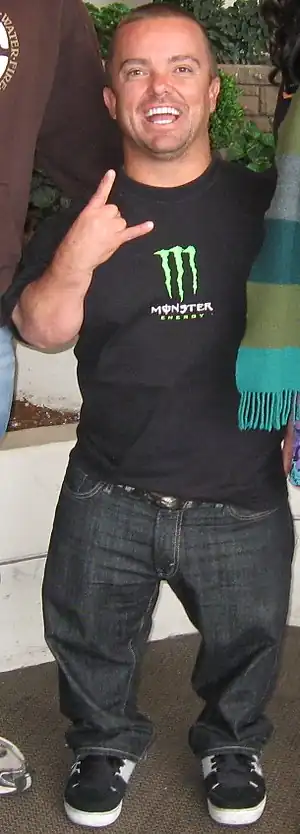 | |
| Jason "Wee Man" Acuña, an American actor and stunt performer with achondroplasia | |
| Pronunciation | |
| Specialty | Medical genetics |
| Symptoms | Short arms and legs, enlarged head, prominent forehead[3] |
| Complications | Ear infections, hyperlordosis, back pain, spinal stenosis, hydrocephalus[3] |
| Causes | Genetic (autosomal dominant mutation in the FGFR3 gene)[3] |
| Risk factors | Paternal age[4][3] |
| Diagnostic method | Based on symptoms, genetic testing if uncertain[5] |
| Differential diagnosis | Hypochondroplasia, thanatophoric dysplasia, cartilage-hair hypoplasia, pseudoachondroplasia[5] |
| Treatment | Support groups, growth hormone therapy, treatment of complications[5] |
| Prognosis | 10 year shorter life expectancy[5] |
| Frequency | 1 in 27,500 people[3] |
Achondroplasia is a genetic disorder whose primary feature is dwarfism.[3] In those with the condition, the arms and legs are short, while the torso is typically of normal length.[3] Those affected have an average adult height of 131 centimetres (4 ft 4 in) for males and 123 centimetres (4 ft) for females.[3] Other features include an enlarged head and prominent forehead.[3] Complications can include sleep apnea or recurrent ear infections.[3] The disorder does not generally affect intelligence.[3]
Achondroplasia is caused by a mutation in the fibroblast growth factor receptor 3 (FGFR3) gene that results in its protein being overactive.[3] The disorder has an autosomal dominant mode of inheritance, meaning only one mutated copy of the gene is required for the condition to occur.[6] About 80% of cases result from a new mutation, which originates in the father's sperm.[5] The rest are inherited from a parent with the condition.[3] The risk of a new mutation increases with the age of the father.[4] In families with two affected parents, children who inherit both affected genes typically die before birth or in early infancy from breathing difficulties.[3] The condition is generally diagnosed based on the symptoms but may be confirmed by genetic testing.[5]
Treatments may include support groups and growth hormone therapy.[5] Efforts to treat or prevent complications such as obesity, hydrocephalus, obstructive sleep apnea, middle ear infections or spinal stenosis may be required.[5] Life expectancy of those affected is about 10 years less than average.[5] Achondroplasia is the most common cause of dwarfism[4] and affects about 1 in 27,500 people.[3] The shortest known adult with the condition is Jyoti Amge, at 62.8 centimetres (2 ft 0.7 in).[7]
Signs and symptoms
- Disproportionate dwarfism
- Shortening of the proximal limbs (called rhizomelic shortening)
- Short fingers and toes with trident hands
- Large head with prominent forehead frontal bossing
- Small midface with a flattened nasal bridge
- Spinal kyphosis (convex curvature) or lordosis (concave curvature)
- Varus (bowleg) or valgus (knock knee) deformities
- Frequent ear infections (due to Eustachian tube blockages), sleep apnea (which can be central or obstructive), and hydrocephalus
Causes
Achondroplasia is caused by a mutation in fibroblast growth factor receptor 3 (FGFR3) gene.[8] This gene is mainly responsible for making the protein, fibroblast growth factor receptor 3. This protein contributes to the production of collagen and other structural components in tissues and bones.[9] When the FGFR3 gene is mutated it interferes with how this protein interacts with growth factors leading to complications with bone production. Cartilage is not able to fully develop into bone, causing the individual to be disproportionately shorter in height.
In normal development FGFR3 has a negative regulatory effect on bone growth. In achondroplasia, the mutated form of the receptor is constitutively active and this leads to severely shortened bones. The effect is genetically dominant, with one mutant copy of the FGFR3 gene being sufficient to cause achondroplasia, while two copies of the mutant gene are invariably fatal (recessive lethal) before or shortly after birth (known as a lethal allele). This occurs due to respiratory failure from an underdeveloped ribcage.[3] A person with achondroplasia thus has a 50% chance of passing dwarfism to each of their offspring. People with achondroplasia can be born to parents that do not have the condition due to spontaneous mutation.[10]
Achondroplasia can be inherited through autosomal dominance. In couples where one partner has achondroplasia there is a 50% chance of passing the disorder onto their child every pregnancy. In situations where both parents have achondroplasia there is a 50% chance the child will have achondroplasia, 25% chance the child will not, and a 25% chance that the child will inherit the gene from both parents resulting in double dominance and leading to severe or lethal bone dysplasia.[11]
Studies have demonstrated that new gene mutations for achondroplasia are exclusively inherited from the father and occur during spermatogenesis; it has been theorized that sperm carrying the mutation in FGFR3 have a selective advantage over sperm with normal FGFR3.[4] The frequency of mutations in sperm leading to achondroplasia increase in proportion to paternal age, as well as in proportion to exposure to ionizing radiation.[12] The occurrence rate of achondroplasia in the children of fathers over 50 years of age is 1 in 1,875, compared to 1 in 15,000 in the general population.[13]
There are two other syndromes with a genetic basis similar to achondroplasia: hypochondroplasia and thanatophoric dysplasia.
Diagnosis

Achondroplasia can be detected before birth by prenatal ultrasound. A DNA test can be performed before birth to detect homozygosity, wherein two copies of the mutant gene are inherited, a lethal condition leading to stillbirths. Clinical features include megalocephaly, short limbs, prominent forehead, thoracolumbar kyphosis and mid-face hypoplasia.[14] Complications like dental malocclusion, hydrocephalus and repeated otitis media can be observed.[14] The risk of death in infancy is increased due to the likelihood of compression of the spinal cord with or without upper airway obstruction.
Radiologic findings
A skeletal survey is useful to confirm the diagnosis of achondroplasia. The skull is large, with a narrow foramen magnum, and relatively small skull base. The vertebral bodies are short and flattened with relatively large intervertebral disk height, and there is congenitally narrowed spinal canal. The iliac wings are small and squared, with a narrow sciatic notch and horizontal acetabular roof.[15][16] The tubular bones are short and thick with metaphyseal cupping and flaring and irregular growth plates.[15] Fibular overgrowth is present. The hand is broad with short metacarpals and phalanges, and a trident configuration. The ribs are short with cupped anterior ends.[15] If the radiographic features are not classic, a search for a different diagnosis should be entertained. Because of the extremely deformed bone structure, people with achondroplasia are often "double jointed". The diagnosis can be made by fetal ultrasound by progressive discordance between the femur length and biparietal diameter by age. The trident hand configuration can be seen if the fingers are fully extended.
Another distinct characteristic of the syndrome is thoracolumbar gibbus in infancy.
.jpg.webp) Achondroplasia
Achondroplasia.jpg.webp) Achondroplasia
Achondroplasia.JPG.webp) Achondroplasia
Achondroplasia
Treatment
There is no known cure for achondroplasia even though the cause of the mutation in the growth factor receptor has been found. Although used by those without achondroplasia to aid in growth, human growth hormone does not help people with achondroplasia, which involve a different hormonal pathway. Usually, the best results appear within the first and second year of therapy.[17] After the second year of growth hormone therapy, beneficial bone growth decreases,[18] so the therapy is not a satisfactory long-term treatment.[17]
The controversial surgery of limb-lengthening will increase the length of the legs and arms of someone with achondroplasia.[19]
Complications
Children
Children with achondroplasia often have less muscle tone; because of this it is common for them to have delayed walking and motor skills. It is also common for children to have bowed legs, scoliosis, lordosis, arthritis, issues with joint flexibility, breathing problems, ear infections, and crowded teeth.[20] These issues can be treated with surgery, braces, or physical therapy.
Hydrocephalus is a severe effect associated with achondroplasia in children. This condition occurs when cerebrospinal fluid is not able to flow in and out of the skull because of how the spine narrows.[21] This fluid build up is associated with an enlarged head, vomiting, lethargy, headaches, and irritability.[22] A shunt surgery is commonly performed to treat this condition, but an endoscopic third ventriculostomy can also be done.[23]
Adults
Adults with achondroplasia often face issues with obesity and sleep apnea. It is also typical for adults to suffer from numbness or tingling in their legs because of nerve compression.
Pregnancy in women with achondroplasia is considered higher risk. Women with achondroplasia generally have their babies delivered through C-sections to prevent complications that could occur with a natural birth.[24]
Epidemiology
Achondroplasia is one of several congenital conditions with similar presentations, such as osteogenesis imperfecta, multiple epiphyseal dysplasia tarda, achondrogenesis, osteopetrosis, and thanatophoric dysplasia. This makes estimates of prevalence difficult, with changing and subjective diagnostic criteria over time. One detailed and long-running study in the Netherlands found that the prevalence determined at birth was only 1.3 per 100,000 live births.[25] Another study at the same time found a rate of 1 per 10,000.[25]
Other animals
Based on their disproportionate dwarfism, some dog breeds traditionally have been classified as "achondroplastic". This is the case for the dachshund, basset hound, corgi and bulldog breeds.[26][27][28] Data from whole genome association studies in short-limbed dogs reveal a strong association of this trait with a retro-gene coding for fibroblast growth factor 4 (FGF4).[29] Therefore, it seems unlikely that dogs and humans are achondroplastic for the same reasons. However, histological studies in some achondroplastic dog breeds have shown altered cell patterns in cartilage that are very similar to those observed in humans exhibiting achondroplasia.[30]
A similar form of achondroplasia was found in a litter of piglets from a phenotypically normal Danish sow. The dwarfism was inherited dominant in the offspring from this litter. The piglets were born phenotypically normal, but became more and more symptomatic as they reached maturity.[31] This involved a mutation of the protein collagen, type X, alpha 1, encoded by the COL10A1 gene. In humans a similar mutation (G595E) has been associated with Schmid metaphyseal chondrodysplasia (SMCD), a relatively mild skeletal disorder that is also associated with dwarfism.
The now-extinct Ancon sheep was created by humans through the selective breeding of common domestic sheep with achondroplasia. The average-sized torso combined with the relatively smaller legs produced by achondroplasia was valued for making affected sheep less likely to escape without affecting the amount of wool or meat each sheep produced.[32]
Research
As of 2019, tentative evidence has found that the experimental peptide drug vosoritide increases growth velocity in those with achondroplasia. The drug inhibits the activity of FGFR3.[33]
See also
References
- ↑ "Achondroplasia". Oxford Dictionaries UK Dictionary. Oxford University Press. Retrieved 2016-01-20.
- ↑ "Achondroplasia". Merriam-Webster Dictionary.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 "Achondroplasia". Genetics Home Reference. May 2012. Archived from the original on 11 December 2019. Retrieved 12 December 2017.
- 1 2 3 4 Horton, William A; Hall, Judith G; Hecht, Jacqueline T (July 2007). "Achondroplasia". The Lancet. 370 (9582): 162–172. doi:10.1016/S0140-6736(07)61090-3. PMID 17630040.
- 1 2 3 4 5 6 7 8 9 Pauli, RM; Adam, MP; Ardinger, HH; Pagon, RA; Wallace, SE; Bean, LJH; Mefford, HC; Stephens, K; Amemiya, A; Ledbetter, N (2012). "Achondroplasia". GeneReviews. PMID 20301331.
- ↑ "Achondroplasia". Genetic and Rare Diseases Information Center (GARD) – an NCATS Program. 2016. Archived from the original on 29 February 2020. Retrieved 12 December 2017.
- ↑ "New world's shortest woman: It's official – Jyoti Amge from India is new record holder". Guinness World Records. 13 December 2011. Archived from the original on 29 June 2017. Retrieved 12 December 2017.
- ↑ "Learning About Achondroplasia". National Human Genome Research Institute (NHGRI). Archived from the original on 2018-09-16. Retrieved 2018-09-26.
- ↑ Reference, Genetics Home. "FGFR3 gene". Genetics Home Reference. Archived from the original on 2018-10-02. Retrieved 2018-09-26.
- ↑ Richette P, Bardin T, Stheneur C (2007). "Achondroplasia: From genotype to phenotype". Joint Bone Spine. 75 (2): 125–30. doi:10.1016/j.jbspin.2007.06.007. PMID 17950653.
- ↑ "Achondroplasia". Archived from the original on 2018-09-26. Retrieved 2018-09-26.
- ↑ Wyrobek AJ, Eskenazi B, Young S, Arnheim N, Tiemann-Boege I, Jabs EW, Glaser RL, Pearson FS, Evenson D (2006). "Advancing age has differential effects on DNA damage, chromatin integrity, gene mutations, and aneuploidies in sperm". Proceedings of the National Academy of Sciences of the United States of America. 103 (25): 9601–9606. doi:10.1073/pnas.0506468103. PMC 1480453. PMID 16766665.
- ↑ Kovac JR, Addai J, Smith RP, Coward RM, Lamb DJ, Lipshultz LI (2013). "The effects of advanced paternal age on fertility" (PDF). Asian Journal of Andrology. 15 (6): 723–728. doi:10.1038/aja.2013.92. PMC 3854059. PMID 23912310. Archived (PDF) from the original on 2020-11-24. Retrieved 2019-05-07.
- 1 2 Beattie, R.M.; Champion, M.P., eds. (2004). Essential questions in paediatrics for MRCPCH (1st ed.). Knutsford, Cheshire: PasTest. ISBN 978-1-901198-99-7.
- 1 2 3 EL-Sobky, TA; Shawky, RM; Sakr, HM; Elsayed, SM; Elsayed, NS; Ragheb, SG; Gamal, R (15 November 2017). "A systematized approach to radiographic assessment of commonly seen genetic bone diseases in children: A pictorial review". J Musculoskelet Surg Res. 1 (2): 25. doi:10.4103/jmsr.jmsr_28_17.
- ↑ "Achondroplasia Pelvis". Archived from the original on 2007-10-22. Retrieved 2007-11-28.
- 1 2 Vajo, Z; Francomano, CA; Wilkin, DJ (2000). "The molecular and genetic basis of fibroblast growth factor receptor 3 disorders: the achondroplasia family of skeletal dysplasias, Muenke craniosynostosis, and Crouzon syndrome with acanthosis nigricans". Endocrine Reviews. 21 (1): 23–39. doi:10.1210/er.21.1.23. PMID 10696568. Archived from the original on 2020-12-05. Retrieved 2019-07-04.
- ↑ Aviezer, D; Golembo, M; Yayon, A (2003). "Fibroblast growth factor receptor-3 as a therapeutic target for Achondroplasia—genetic short limbed dwarfism". Current Drug Targets. 4 (5): 353–65. doi:10.2174/1389450033490993. PMID 12816345.
- ↑ Kitoh H, Kitakoji T, Tsuchiya H, Katoh M, Ishiguro N (2007). "Distraction osteogenesis of the lower extremity in patients that have achondroplasia/hypochondroplasia treated with transplantation of culture-expanded bone marrow cells and platelet-rich plasma". J Pediatr Orthop. 27 (6): 629–34. doi:10.1097/BPO.0b013e318093f523. PMID 17717461.
- ↑ "Dwarfism". kidshealth.org. Archived from the original on 2016-01-21. Retrieved 2018-09-26.
- ↑ "Achondroplasia | Genetic and Rare Diseases Information Center (GARD) – an NCATS Program". rarediseases.info.nih.gov. Archived from the original on 2020-02-29. Retrieved 2018-09-26.
- ↑ Kieffer, Sara. "Achondroplasia | Johns Hopkins Pediatric Neurosurgery". Archived from the original on 2018-09-26. Retrieved 2018-09-26.
- ↑ "Hydrocephalus - Diagnosis and treatment - Mayo Clinic". www.mayoclinic.org. Archived from the original on 2019-08-30. Retrieved 2018-09-26.
- ↑ Services, Department of Health & Human. "Dwarfism". Archived from the original on 2018-09-26. Retrieved 2018-09-26.
- 1 2 Online Mendelian Inheritance in Man (OMIM): ACHONDROPLASIA; ACH - 100800
- ↑ "WebMD". Archived from the original on 2013-11-04. Retrieved 2013-11-09.
- ↑ Jones, T.C.; Hunt, R.D. (1979). "The musculoskeletal system". In Jones, T.C.; Hunt, R.D.; Smith, H.A. (eds.). Veterinary Pathology (5th ed.). Philadelphia: Lea & Febiger. pp. 1175–6. ISBN 978-0812107890.
- ↑ Willis M.B. (1989). "Inheritance of specific skeletal and structural defects". In Willis M.B. (ed.). Genetics of the Dog. Great Britain: Howell Book House. pp. 119–120. ISBN 978-0876055519.
- ↑ Parker HG, VonHoldt BM, Quignon P, et al. (August 2009). "An expressed fgf4 retrogene is associated with breed-defining chondrodysplasia in domestic dogs". Science. 325 (5943): 995–8. Bibcode:2009Sci...325..995P. doi:10.1126/science.1173275. PMC 2748762. PMID 19608863.
- ↑ Braund KG, Ghosh P, Taylor TK, Larsen LH (September 1975). "Morphological studies of the canine intervertebral disc. The assignment of the beagle to the achondroplastic classification". Res. Vet. Sci. 19 (2): 167–72. doi:10.1016/S0034-5288(18)33527-6. PMID 1166121.
- ↑ Nielsen VH, Bendixen C, Arnbjerg J, et al. (December 2000). "Abnormal growth plate function in pigs carrying a dominant mutation in type X collagen". Mamm. Genome. 11 (12): 1087–92. doi:10.1007/s003350010212. PMID 11130976.
- ↑ Gidney, Louisa (May–June 1019). "Earliest Archaeological Evidence of the Ancon Mutation in Sheep from Leicester, UK". International Journal of Osteoarchaeology. 15 (27): 318–321. doi:10.1002/oa.872. ISSN 1099-1212.
- ↑ Savarirayan, Ravi (July 4, 2019). "C-Type Natriuretic Peptide Analogue Therapy in Children with Achondroplasia". New England Journal of Medicine. 381 (1): 25–35. doi:10.1056/NEJMoa1813446. PMID 31269546.
External links
| Classification | |
|---|---|
| External resources |
|
| Look up achondroplasia in Wiktionary, the free dictionary. |
- Achondroplasia at Curlie
- Pauli RM (1998). "Achondroplasia". In Pagon RA, Bird TD, Dolan CR, et al. (eds.). GeneReviews. Seattle WA: University of Washington, Seattle. PMID 20301331. NBK1152. Archived from the original on 2017-01-28. Retrieved 2017-08-29.