Angiotensin II receptor blocker
| Angiotensin II receptor blocker | |
|---|---|
| Drug class | |
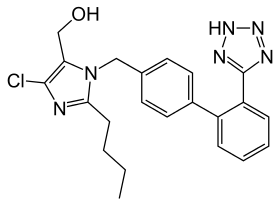 Losartan, the first ARB | |
| Names | |
| Stem | -sartan[1] |
| Other names | Angiotensin receptor blockers, angiotensin II receptor type 1 (AT1) antagonists,[2] angiotensin II receptor antagonists, AT1 receptor antagonists |
| Clinical data | |
| Uses | High blood pressure, heart failure, coronary heart disease, kidney disease[3] |
| Side effects | Low blood pressure, high potassium, kidney problems[3] |
| Interactions | NSAIDs[3] |
| Common types | Candesartan, irbesartan, losartan, olmesartan, telmisartan, valsartan[4] |
| External links | |
| Drugs.com | Drug Classes |
Angiotensin II receptor blockers (ARBs), also known as angiotensin receptor blockers, are a class of medication primarily used to treat high blood pressure, heart failure, coronary heart disease, and kidney disease.[3] They are taken by mouth.[3] Their use with ACE inhibitors is not recommended.[5]
Side effects can include low blood pressure, high potassium, and kidney problems.[3] Kidney problems are more likely in those with renal artery stenosis.[3] Compared to ACE inhibitors they are less likely to cause cough or angioedema.[3] Use during pregnancy can harm the baby.[6] They work by blocking the angiotensin II receptor type 1 (AT1) thereby preventing the effects of angiotensin II.[7] This results in dilation of blood vessels and increased release of water and sodium by the kidneys.[4]
ARBs, specifically losartan, came into medical use in 1995.[8] Some are available as generic medication and are not very expensive.[3] In the United States losartan and irbesartan were the least expensive at about 90 USD per month in 2016.[9] In the United States they are a first line treatment for high blood pressure, along with calcium channel blockers, thiazide diuretics, and ACE inhibitors.[10]
Types
ARBs include candesartan (Atacand), lisinopril, telmisartan (Micardis), and valsartan (Diovan), fimasartan (Kanarb).
A number are also available in combination with HCTZ, chlorthalidone, or amlodipine within a single pill.[9]
Medical uses
Angiotensin II receptor blockers are used primarily for the treatment of hypertension where the person is intolerant of ACE inhibitor therapy primarily because of persistent cough.[11] More recently, they have been used for the treatment of heart failure in people intolerant of ACE inhibitor therapy, in particular candesartan. Irbesartan and losartan have trial data showing benefit in hypertensive patients with type 2 diabetes, and may delay the progression of diabetic nephropathy.
Candesartan is used experimentally in preventive treatment of migraine.[12][13] Lisinopril has been found less often effective than candesartan at preventing migraine.[14]
The angiotensin II receptor blockers have differing potencies in relation to blood pressure control, with statistically differing effects at the maximal doses.[15]
Some of these drugs have a uricosuric effect.[16][17]
In 2008, they were reported to have a negative association with Alzheimer's disease (AD). Those people taking angiotensin receptor blockers (ARBs) were 35–40% less likely to develop AD than those using other antihypertensives.[18][19]
Side effects
This class of drugs is usually well tolerated. Common adverse drug reactions (ADRs) include: dizziness, headache, and/or hyperkalemia. Infrequent ADRs associated with therapy include: first dose orthostatic hypotension, rash, diarrhea, dyspepsia, abnormal liver function, muscle cramp, myalgia, back pain, insomnia, decreased hemoglobin levels, renal impairment, pharyngitis, and/or nasal congestion.[20] A 2014 Cochrane systematic review based on randomized controlled trials reported that when comparing patients taking ACE inhibitors to patients taking ARBs, fewer ARB patients withdrew from the study due to adverse events compared to ACE inhibitor patients.[21]
While one of the main rationales for the use of this class is the avoidance of a persistent dry cough and/or angioedema associated with ACE inhibitor therapy, rarely they may still occur. In addition, there is also a small risk of cross-reactivity in patients having experienced angioedema with ACE inhibitor therapy.[20]
Heart attack
The issue of whether angiotensin II receptor antagonists slightly increase the risk of myocardial infarction (MI or heart attack) is currently being investigated. Some studies suggest ARBs can increase the risk of MI.[22] However, other studies have found ARBs do not increase the risk of MI.[23] To date, with no consensus on whether ARBs have a tendency to increase the risk of myocardial infarction, further investigations are underway.
Indeed, as a consequence of AT1 blockade, ARBs increase angiotensin II levels several-fold above baseline by uncoupling a negative-feedback loop. Increased levels of circulating angiotensin II result in unopposed stimulation of the AT2 receptors, which are, in addition, upregulated. However, recent data suggest AT2 receptor stimulation may be less beneficial than previously proposed, and may even be harmful under certain circumstances through mediation of growth promotion, fibrosis, and hypertrophy, as well as eliciting proatherogenic and proinflammatory effects.[24][25][26]
Cancer
A study published in 2010 determined that "...meta-analysis of randomised controlled trials suggests that ARBs are associated with a modestly increased risk of new cancer diagnosis. Given the limited data, it is not possible to draw conclusions about the exact risk of cancer associated with each particular drug. These findings warrant further investigation." [27] A later meta-analysis by the U.S. Food and Drug Administration (FDA) of 31 randomized controlled trials comparing ARBs to other treatment found no evidence of an increased risk of incident (new) cancer, cancer-related death, breast cancer, lung cancer, or prostate cancer in patients receiving ARBs.[28] In 2013, comparative effectiveness research from the United States Department of Veterans Affairs on the experience of more than a million Veterans found no increased risks for either lung cancer [29] (original article Archived 2014-12-10 at the Wayback Machine in Journal of Hypertension) or prostate cancer.[30] The researchers concluded: "In this large nationwide cohort of United States Veterans, we found no evidence to support any concern of increased risk of lung cancer among new users of ARBs compared with nonusers. Our findings were consistent with a protective effect of ARBs."[29]
In May 2013, a senior regulator at the Food & Drug Administration, Medical Team Leader Thomas A. Marciniak, revealed publicly that contrary to the FDA's official conclusion that there was no increased cancer risk, after a patient-by-patient examination of the available FDA data he had concluded that there was a lung-cancer risk increase of about 24% in ARB patients, compared with patients taking a placebo or other drugs. One of the criticisms Marciniak made was that the earlier FDA meta-analysis did not count lung carcinomas as cancers. In ten of the eleven studies he examined, Marciniak said that there were more lung cancer cases in the ARB group than the control group. Ellis Unger, chief of the drug-evaluation division that includes Dr. Marciniak, was quoted as calling the complaints a "diversion," and saying in an interview, "We have no reason to tell the public anything new." In an article about the dispute, the Wall Street Journal interviewed three other doctors to get their views; one had "no doubt" ARBs increased cancer risk, one was concerned and wanted to see more data, and the third thought there was either no relationship or a hard to detect, low-frequency relationship.[31]
A 2016 meta-analysis including 148,334 patients found no significant differences in cancer incidence associated with ARB use.[32]
Kidney failure
Although ARBs have protective effects against developing kidney diseases for patients with diabetes and previous hypertension without administration of ARBs,[33] ARBs may worsen kidney functions such as reducing glomerular filtration rate associated with a rise of serum creatinine in patients with pre-existing proteinuria, renal artery stenosis, hypertensive nephrosclerosis, heart failure, polycystic kidney disease, chronic kidney disease, interstitial fibrosis, focal segmental glomerulosclerosis, or any conditions such as ARBs-treated but still clinically present hypertension that lead to abnormal narrowing of blood vessels to the kidney that interrupts oxygen and nutrient supply to the organ.[34][35][36][37][38][39][33]
Mechanism of action
These substances are AT1-receptor antagonists; that is, they block the activation of angiotensin II AT1 receptors. AT1 receptors are found in smooth muscle cells of vessels, cortical cells of the adrenal gland, and adrenergic nerve synapses. Blockage of AT1 receptors directly causes vasodilation, reduces secretion of vasopressin, and reduces production and secretion of aldosterone, among other actions. The combined effect reduces blood pressure.
The specific efficacy of each ARB within this class depends upon a combination of three pharmacodynamic (PD) and pharmacokinetic (PK) parameters. Efficacy requires three key PD/PK areas at an effective level; the parameters of the three characteristics will need to be compiled into a table similar to one below, eliminating duplications and arriving at consensus values; the latter are at variance now.
Pressor inhibition
Pressor inhibition at trough level - this relates to the degree of blockade or inhibition of the blood pressure-raising ("pressor") effect of angiotensin II. However, pressor inhibition is not a measure of blood pressure-lowering (BP) efficacy per se. The rates as listed in the U.S. Food and Drug Administration (FDA) Package Inserts (PIs) for inhibition of this effect at the 24th hour for the ARBs are as follows: (all doses listed in PI are included)
- Valsartan 80 mg 30%
- Telmisartan 80 mg 40%
- Losartan 100 mg 25–40%
- Irbesartan 150 mg 40%
- Irbesartan 300 mg 60%
- Azilsartan 32 mg 60%
- Olmesartan 20 mg 61%
- Olmesartan 40 mg 74%
AT1 affinity vs AT2
The ratios of AT1 to AT2 in binding affinities of the specific ARBs are shown as follows. Whereas, AT1 affinity vs AT2 is not a meaningful efficacy measurement of BP response.
- Losartan – 1000-fold
- Telmisartan – 3000-fold
- Irbesartan – 8500-fold
- Candesartan – greater than 10000-fold
- Olmesartan – 12500-fold
- Valsartan – 30000-fold higher than AT2 (the ratio of binding affinities of valsartan to AT1 and AT2 is 30000:1)[40][41]
- Saprisartan – ???[42]
Component
Nearly all ARBs contain biphenyltetrazole moiety except telmisartan and eprosartan.[41]
Active agent
Losartan carries a heterocycle imidazole while valsartan carries a nonplanar acylated amino acid.[41]
Biological half-life
The third area needed to complete the overall efficacy picture of an ARB is its biological half-life. The half-lives from the U.S. Food and Drug Administration (FDA) package inserts (PIs) are as follows:
- Valsartan 6 hours
- Losartan 6–9 hours
- Azilsartan 11 hours
- Irbesartan 11–15 hours
- Olmesartan 13 hours
- Telmisartan 24 hours
- Fimasartan 7–11 hours
Chemistry
Losartan, irbesartan, olmesartan, candesartan, valsartan, fimasartan and azilsartan include the tetrazole group (a ring with four nitrogen and one carbon). Losartan, irbesartan, olmesartan, candesartan, and telmisartan include one or two imidazole groups.
Comparison
| Drug | Trade name | Biological half-life [hrs] | Peak plasma concentration [Tmax] | Protein binding [%] | Bioavailability [%] | Renal/hepatic clearance [%] | Food effect | Daily dosage [mg] | Metabolism/transporter |
|---|---|---|---|---|---|---|---|---|---|
| Losartan | Cozaar | 6–9 |
|
98.7% | 33% | 10/90% | Minimal | 50–100 | Sensitive substrates: CYP2C9 and CYP3A4[43] |
| EXP 3174 | 6–9 | 99.8% | – | 50/50% | – | – | |||
| Candesartan | Atacand | 9 | 3–4 hrs[44] | >99% | 15% | 60/40% | No | 4–32 | Moderate sensitive substrate: CYP2C9[44] |
| Valsartan | Diovan | 6 | 2–4 hrs[45] | 95% | 25% | 30/70% | No | 80–320 | Substrates:MRP2 and OATP1B1/SLCO1B1[45] |
| Irbesartan | Avapro | 11–15 | 1.5–2 hrs[46] | 90–95% | 70% | 20/80% | No | 150–300 | Minor substrates of CYP2C9[46] |
| Telmisartan | Micardis | 24 | 0.5–1 hr [47] | >99% | 42–58% | 1/99% | No | 40–80 | Unknown[47] |
| Eprosartan | Teveten | 5 | 1–2 hrs [48] | 98% | 13% | 30/70% | No | 400–800 | None known [48] |
| Olmesartan | Benicar/Olmetec | 14–16 | 1–2 hrs [49] | >99% | 29% | 40/60% | No | 10–40 | Substrates of OATP1B1/SLCO1B1[49] |
| Azilsartan | Edarbi | 11 | 1.5–3 hrs [50] | >99% | 60% | 55/42% | No | 40–80 | Minor substrates of CYP2C9 [50] |
| Fimasartan | Kanarb | 7–11 | 0.5–3 hrs after dosing.[51] | >97% | 30–40% | – | – | 30–120 | No related research as of February 2019. |
| Drug | Trade name | Biological half-life [hrs] | Peak plasma concentration [Tmax] | Protein binding [%] | Bioavailability [%] | Renal/hepatic clearance [%] | Food effect | Daily dosage [mg] | Metabolism/transporter |
History
Society and culture
Impurities
In 2018 and in 2019, the U.S Food and Drug Administration (FDA) found traces of NDMA and NDEA impurities in the angiotensin II receptor blocker (ARB) drug products valsartan, losartan, and irbesartan.[57][58][59][60][61] The FDA stated "In June 2018, FDA was informed of the presence of an impurity, identified as N-Nitrosodimethylamine (NDMA), from one valsartan API producer. Since then, FDA has determined that other types of nitrosamine compounds, e.g., N-Nitrosodiethylamine (NDEA), are present at unacceptable levels in APIs from multiple API producers of valsartan and other drugs in the ARB class."[62] In 2018, the FDA issued guidance to the industry on how to assess and control the impurities.[63]
In August 2020, the European Medicines Agency (EMA) provided guidance to marketing authorization holders on how to avoid the presence of nitrosamine impurities in human medicines and asked them to review all chemical and biological human medicines for the possible presence of nitrosamines and to test the products at risk.[64]
In November 2020, the Committee for Medicinal Products for Human Use (CHMP) of the EMA aligned recommendations for limiting nitrosamine impurities in sartan medicines with recommendations it issued for other classes of medicines.[65] The main change concerns the limits for nitrosamines, which previously applied to the active ingredients but now apply instead to the finished products (e.g. tablets).[65] These limits, based on internationally agreed standards (ICH M7(R1)), should ensure that the excess risk of cancer from nitrosamines in any sartan medicines is below 1 in 100,000 for a person taking the medicine for lifelong treatment.[65]
These sartan medicines have a specific ring structure (tetrazole) whose synthesis could potentially lead to the formation of nitrosamine impurities.[65][66] Other sartan medicines which do not have this ring, such as azilsartan, eprosartan and telmisartan, were not included in this review but are covered by the subsequent review of other medicines.[65]
Longevity
Knockout of the Agtr1a gene that encodes AT1 results in prolongation of the life-span of mice by 26% compared to controls. The likely mechanism is reduction of oxidative damage (especially to mitochondria) and overexpression of renal prosurvival genes. The ARBs seem to have the same effect.[67][68]
References
- ↑ The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances (PDF). WHO. 2011. p. 37. Archived (PDF) from the original on 2018-07-12. Retrieved 2021-04-18.
- ↑ Mirabito Colafella, Katrina M.; Uijl, Estrellita; Jan Danser, A.H. (2019). "Interference With the Renin–Angiotensin System (RAS): Classical Inhibitors and Novel Approaches". Encyclopedia of Endocrine Diseases. Elsevier. pp. 523–530. doi:10.1016/b978-0-12-801238-3.65341-2. ISBN 978-0-12-812200-6.
- 1 2 3 4 5 6 7 8 9 Hitchings, Andrew; Lonsdale, Dagan; Burrage, Daniel; Baker, Emma (2019). The Top 100 Drugs: Clinical Pharmacology and Practical Prescribing (2nd ed.). Elsevier. p. 52. ISBN 978-0-7020-7442-4. Archived from the original on 2021-05-22. Retrieved 2021-11-09.
- 1 2 "List of Angiotensin receptor blockers (angiotensin II inhibitors)". Drugs.com. 2020-02-28. Archived from the original on 2021-08-27. Retrieved 2020-03-21.
- ↑ BNF (80 ed.). BMJ Group and the Pharmaceutical Press. September 2020 – March 2021. p. 152. ISBN 978-0-85711-369-6.
{{cite book}}: CS1 maint: date format (link) - ↑ "Angiotensin receptor blockers (ARBs)". Archived from the original on 9 March 2021. Retrieved 19 April 2021.
- ↑ "ARBs", Angiotensin II Receptor Antagonists, Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases, 2012, PMID 31643954, archived from the original on 2021-08-27, retrieved 2020-03-21,
The angiotensin II receptor antagonists, also known as angiotensin receptor blockers (ARBs), are a family of agents that bind to and inhibit the angiotensin II type 1 receptor (AT1) and thus inhibit the renin-angiotensin system and its cascade of effects in causing arteriolar contraction and sodium retention. While angiotensin converting enzyme (ACE) inhibitors block the cleavage of angiotensin I to angiotensin II, the active peptide that causes a pressor response, the ARBs inhibit its peripheral action.
- ↑ Kirk, Julienne K. (1 June 1999). "Angiotensin-II Receptor Antagonists: Their Place in Therapy". American Family Physician. 59 (11): 3140. ISSN 0002-838X. Archived from the original on 12 February 2021. Retrieved 18 April 2021.
- 1 2 Massachusetts, Christina C. Andros, PharmD/MBA Candidate 2017 Western New England University College of Pharmacy Springfield, Massachusetts Jared L. Ostroff, PharmD, BCACP Clinical Assistant Professor of Ambulatory Care Western New England University College of Pharmacy Department of Pharmacy Practice Springfield, Massachusetts Marissa L. Wolff, PharmD, BCPS Clinical Assistant Professor of Ambulatory Care Western New England University College of Pharmacy Department of Pharmacy Practice Springfield. "An Overview of Generic Angiotensin Receptor Blockers". www.uspharmacist.com. Archived from the original on 9 September 2020. Retrieved 19 April 2021.
- ↑ Herman, LL; Padala, SA; Annamaraju, P; Bashir, K (January 2021). "Angiotensin Converting Enzyme Inhibitors (ACEI)". PMID 28613705.
{{cite journal}}: Cite journal requires|journal=(help) - ↑ "Choice of drug therapy in primary (essential) hypertension". UpToDate. Archived from the original on 2016-01-31. Retrieved 2019-02-03.
- ↑ Tronvik E, Stovner LJ, Helde G, Sand T, Bovim G (January 2003). "Prophylactic treatment of migraine with an angiotensin II receptor blocker: a randomized controlled trial". JAMA. 289 (1): 65–9. doi:10.1001/jama.289.1.65. PMID 12503978. S2CID 35939042.
- ↑ Cernes R, Mashavi M, Zimlichman R (2011). "Differential clinical profile of candesartan compared to other angiotensin receptor blockers". Vascular Health and Risk Management. 7: 749–59. doi:10.2147/VHRM.S22591. PMC 3253768. PMID 22241949.
- ↑ Gales BJ, Bailey EK, Reed AN, Gales MA (February 2010). "Angiotensin-converting enzyme inhibitors and angiotensin receptor blockers for the prevention of migraines". The Annals of Pharmacotherapy. 44 (2): 360–6. doi:10.1345/aph.1M312. PMID 20086184. S2CID 207263658.
- ↑ Kassler-Taub K, Littlejohn T, Elliott W, Ruddy T, Adler E (April 1998). "Comparative efficacy of two angiotensin II receptor antagonists, irbesartan and losartan in mild-to-moderate hypertension. Irbesartan/Losartan Study Investigators". American Journal of Hypertension. 11 (4 Pt 1): 445–53. doi:10.1016/S0895-7061(97)00491-3. PMID 9607383.
- ↑ Dang A, Zhang Y, Liu G, Chen G, Song W, Wang B (January 2006). "Effects of losartan and irbesartan on serum uric acid in hypertensive patients with hyperuricaemia in Chinese population". Journal of Human Hypertension. 20 (1): 45–50. doi:10.1038/sj.jhh.1001941. PMID 16281062.
- ↑ Daskalopoulou SS, Tzovaras V, Mikhailidis DP, Elisaf M (2005). "Effect on serum uric acid levels of drugs prescribed for indications other than treating hyperuricaemia". Current Pharmaceutical Design. 11 (32): 4161–75. doi:10.2174/138161205774913309. PMID 16375738.
- ↑ Li NC, Lee A, Whitmer RA, Kivipelto M, Lawler E, Kazis LE, Wolozin B (January 2010). "Use of angiotensin receptor blockers and risk of dementia in a predominantly male population: prospective cohort analysis". BMJ. 340 (9): b5465. doi:10.1136/bmj.b5465. PMC 2806632. PMID 20068258.
- ↑ "Potential of antihypertensive drugs for the prevention and treatment of Alzheimer's disease". Expert Review of Neurotherapeutics. 8 (9): 1285–1287. September 2008. doi:10.1586/14737175.8.9.1285.
- 1 2 Rossi S, editor. Australian Medicines Handbook 2006. Adelaide: Australian Medicines Handbook; 2006.
- ↑ Li EC, Heran BS, Wright JM (August 2014). "Angiotensin converting enzyme (ACE) inhibitors versus angiotensin receptor blockers for primary hypertension". The Cochrane Database of Systematic Reviews (8): CD009096. doi:10.1002/14651858.CD009096.pub2. PMC 6486121. PMID 25148386.
- ↑ Strauss MH, Hall AS (August 2006). "Angiotensin receptor blockers may increase risk of myocardial infarction: unraveling the ARB-MI paradox". Circulation. 114 (8): 838–54. doi:10.1161/CIRCULATIONAHA.105.594986. PMID 16923768.
- ↑ Tsuyuki RT, McDonald MA (August 2006). "Angiotensin receptor blockers do not increase risk of myocardial infarction". Circulation. 114 (8): 855–60. doi:10.1161/CIRCULATIONAHA.105.594978. PMID 16923769.
- ↑ Levy BI (September 2005). "How to explain the differences between renin angiotensin system modulators". American Journal of Hypertension. 18 (9 Pt 2): 134S–141S. doi:10.1016/j.amjhyper.2005.05.005. PMID 16125050.
- ↑ Lévy BI (January 2004). "Can angiotensin II type 2 receptors have deleterious effects in cardiovascular disease? Implications for therapeutic blockade of the renin-angiotensin system". Circulation. 109 (1): 8–13. doi:10.1161/01.CIR.0000096609.73772.C5. PMID 14707017.
- ↑ Reudelhuber TL (December 2005). "The continuing saga of the AT2 receptor: a case of the good, the bad, and the innocuous". Hypertension. 46 (6): 1261–2. doi:10.1161/01.HYP.0000193498.07087.83. PMID 16286568.
- ↑ Sipahi I, Debanne SM, Rowland DY, Simon DI, Fang JC (July 2010). "Angiotensin-receptor blockade and risk of cancer: meta-analysis of randomised controlled trials". The Lancet. Oncology. 11 (7): 627–36. doi:10.1016/S1470-2045(10)70106-6. PMC 4070221. PMID 20542468.
- ↑ "Angiotensin FDA Drug Safety Communication: No increase in risk of cancer with certain blood pressure drugs – Angiotensin Receptor Blockers (ARBs)". Food and Drug Administration (FDA). 2 June 2011. Archived from the original on 8 December 2011.
- 1 2 Rao GA, Mann JR, Shoaibi A, Pai SG, Bottai M, Sutton SS, et al. (August 2013). "Angiotensin receptor blockers: are they related to lung cancer?". Journal of Hypertension. 31 (8): 1669–75. doi:10.1097/HJH.0b013e3283621ea3. PMC 3879726. PMID 23822929.
- ↑ Rao GA, Mann JR, Bottai M, Uemura H, Burch JB, Bennett CL, et al. (July 2013). "Angiotensin receptor blockers and risk of prostate cancer among United States veterans". Journal of Clinical Pharmacology. 53 (7): 773–8. doi:10.1002/jcph.98. PMC 3768141. PMID 23686462.
- ↑ Burton, Thomas M. (31 May 2013). "Dispute Flares Inside FDA Over Safety of Popular Blood-Pressure Drugs". The Wall Street Journal. Archived from the original on 15 February 2018. Retrieved 1 May 2018.
- ↑ Zhao YT, Li PY, Zhang JQ, Wang L, Yi Z (May 2016). "Angiotensin II Receptor Blockers and Cancer Risk: A Meta-Analysis of Randomized Controlled Trials". Medicine. 95 (18): e3600. doi:10.1097/MD.0000000000003600. PMC 4863811. PMID 27149494.
- 1 2 Tucker, Bryan M.; Perazella, Mark A. (2019). "Medications: 3. What are the major adverse effects on the kidney of ACE inhibitors and ARBs?". Nephrology Secrets. Elsevier. pp. 78–83. doi:10.1016/b978-0-323-47871-7.00019-8. ISBN 978-0-323-47871-7.
due to inhibition of angiotensin II production by ACE inhibitors or competitive antagonism of the angiotensin II receptor by ARBs... results in loss of angiotensin II–induced efferent arteriolar tone, leading to a drop in glomerular filtration fraction and GFR. The efferent arteriolal vasodilation reduces intraglomerular hypertension (and pressure-related injury) and maintains perfusion (and oxygenation) of the peritubular capillaries.
- ↑ Toto RD, Mitchell HC, Lee HC, Milam C, Pettinger WA (October 1991). "Reversible renal insufficiency due to angiotensin converting enzyme inhibitors in hypertensive nephrosclerosis". Annals of Internal Medicine. 115 (7): 513–9. doi:10.7326/0003-4819-115-7-513. PMID 1883120.
- ↑ Bakris GL, Weir MR (March 2000). "Angiotensin-converting enzyme inhibitor-associated elevations in serum creatinine: is this a cause for concern?". Archives of Internal Medicine. 160 (5): 685–93. doi:10.1001/archinte.160.5.685. PMID 10724055.
- ↑ Remuzzi G, Ruggenenti P, Perico N (April 2002). "Chronic renal diseases: renoprotective benefits of renin-angiotensin system inhibition". Annals of Internal Medicine. 136 (8): 604–15. doi:10.7326/0003-4819-136-8-200204160-00010. PMID 11955029. S2CID 24795760.
- ↑ Sarafidis PA, Khosla N, Bakris GL (January 2007). "Antihypertensive therapy in the presence of proteinuria". American Journal of Kidney Diseases. 49 (1): 12–26. doi:10.1053/j.ajkd.2006.10.014. PMID 17185142. S2CID 18337587.
- ↑ Weir MR (October 2002). "Progressive renal and cardiovascular disease: optimal treatment strategies". Kidney International. 62 (4): 1482–92. doi:10.1111/j.1523-1755.2002.kid591.x. PMID 12234333.
- ↑ "ACE Inhibitors and ARBs in Patients with Kidney Disease". Pharmacy Times. Archived from the original on 2015-12-30. Retrieved 2019-02-05.
- ↑ Kjeldsen, Sverre E; Brunner, Hans R; McInnes, Gordon T; Stolt, Pelle (2005). "Valsartan in the treatment of hypertension". Aging Health. Future Medicine Ltd. 1 (1): 27–36. doi:10.2217/1745509x.1.1.27.
- 1 2 3 Siragy HM (November 2002). "Angiotensin receptor blockers: how important is selectivity?". American Journal of Hypertension. 15 (11): 1006–14. doi:10.1016/s0895-7061(02)02280-x. PMID 12441224.
- ↑ "Saprisartan". drugbank.ca. Archived from the original on 28 September 2016. Retrieved 1 May 2018.
- 1 2 "LOSARTAN- losartan potassium tablet, film coated". DailyMed. 2018-12-26. Archived from the original on 2019-02-07. Retrieved 2019-02-06.
12.3 Pharmacokinetics/ Absorption: Following oral administration, the systemic bioavailability of losartan is approximately 33%. Mean peak concentrations of losartan and its active metabolite are reached in 1 hour and in 3 to 4 hours, respectively. While maximum plasma concentrations of losartan and its active metabolite are approximately equal, the AUC (area under the curve) of the metabolite is about 4 times as great as that of losartan. A meal slows absorption of losartan and decreases its Cmax but has only minor effects on losartan AUC or on the AUC of the metabolite (≈10% decrease). The pharmacokinetics of losartan and its active metabolite are linear with oral losartan doses up to 200 mg and do not change over time.
- 1 2 "CANDESARTAN - candesartan tablet". DailyMed. 2017-06-27. Archived from the original on 2019-02-07. Retrieved 2019-02-06.
- 1 2 "VALSARTAN - valsartan tablet". DailyMed. 2017-12-07. Archived from the original on 2019-02-07. Retrieved 2019-02-06.
- 1 2 "IRBESARTAN - irbesartan tablet". DailyMed. 2018-09-04. Archived from the original on 2019-02-07. Retrieved 2019-02-06.
- 1 2 "TELMISARTAN - telmisartan tablet". DailyMed. 2018-11-01. Archived from the original on 2019-02-07. Retrieved 2019-02-06.
- 1 2 "EPROSARTAN MESYLATE- eprosartan mesylate tablet, film coated". DailyMed. 2014-12-05. Archived from the original on 2019-02-07. Retrieved 2019-02-06.
- 1 2 "OLMESARTAN MEDOXOMIL - olmesartan medoxomil tablet, film coated". DailyMed. 2017-05-04. Archived from the original on 2019-02-07. Retrieved 2019-02-06.
- 1 2 "EDARBI- azilsartan kamedoxomil tablet". DailyMed. 2018-01-25. Archived from the original on 2019-02-07. Retrieved 2019-02-06.
- ↑ Gu, N., Kim, B., Kyoung, S.L., Kim, S.E., Nam, W.S., Yoon, S.H., Cho, J., Shin, S., Jang, I., Yu, K. The Effect of Fimasartan, an Angiotensin Receptor Type 1 Blocker, on the Pharmacokinetics and Pharmacodynamics of Warfarin in Healthy Korean Male Volunteers: A One- Sequence, Two-Period Crossover Clinical Trial. (2012). Clinical Therapeutics. 34(7): 1592–1600.
- ↑ Burnier, M.; Brunner, H. R. (2000), "Angiotensin II receptor antagonists", Lancet, 355 (9204): 637–645, doi:10.1016/S0140-6736(99)10365-9, PMID 10696996, S2CID 18835715
- ↑ Analogue-based Drug Discovery (Optimizing Antihypertensive Therapy by Angiotensin Receptor Blockers; Farsang, C., Fisher, J., p.157–167) Editors; Fischer, J., Ganellin, R. Wiley-VCH 2006. ISBN 978-3-527-31257-3
- ↑ Brousil, J. A.; Burke, J. M. (2003), "Olmesartan Medoxomil: An Angiotensin II-Receptor Blocker", Clinical Therapeutics, 25 (4): 1041–1055, doi:10.1016/S0149-2918(03)80066-8, PMID 12809956
- ↑ Brunner, H. R. (2002), "The new oral angiotensin II antagonist olmesartan medoxomil: a concise overview", Journal of Human Hypertension, 16 (2): 13–16, doi:10.1038/sj.jhh.1001391, PMID 11967728, ProQuest 219966061
- ↑ Zusman, R. M.; Jullien, V.; Lemetayer, P.; Jarnier, P.; Clementy, J. (1999), "Are There Differences Among Angiotensin Receptor Blockers?", American Journal of Hypertension, 12 (2 Pt 1): 231–235, doi:10.1016/S0895-7061(99)00116-8, PMID 10090354
- ↑ "FDA Updates and Press Announcements on Angiotensin II Receptor Blocker (ARB) Recalls (Valsartan, Losartan, and Irbesartan)". Food and Drug Administration (FDA). 20 August 2018. Archived from the original on 3 October 2019. Retrieved 17 September 2019.
- ↑ "Statement on the agency's ongoing efforts to resolve safety issue with ARB medications". Food and Drug Administration (FDA). 28 August 2019. Archived from the original on 17 September 2019. Retrieved 17 September 2019.
- ↑ "FDA's Assessment of Currently Marketed ARB Drug Products". Food and Drug Administration (FDA). 4 April 2019. Archived from the original on 16 September 2019. Retrieved 17 September 2019.
- ↑ "Search List of Recalled Angiotensin II Receptor Blockers (ARBs) including Valsartan, Losartan and Irbesartan". Food and Drug Administration (FDA). 28 June 2019. Archived from the original on 16 September 2019. Retrieved 17 September 2019.
- ↑ "Updated: Torrent Pharmaceuticals Limited Expands Voluntary Nationwide Recall of Losartan Potassium Tablets, USP and Losartan Potassium / Hydrochlorothiazide Tablets, USP". U.S. Food and Drug Administration. 23 September 2019. Archived from the original on 6 October 2019. Retrieved 24 September 2019.
- ↑ "General Advice ARB" (PDF). Food and Drug Administration (FDA). Archived from the original on 12 November 2019. Retrieved 17 September 2019.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - ↑ "M7(R1) Assessment and Control of DNA Reactive (Mutagenic) Impurities in Pharmaceuticals To Limit Potential Carcinogenic Risk" (PDF). Food and Drug Administration (FDA). 30 August 2018. Archived from the original on 28 August 2019. Retrieved 17 September 2019.
- Lay summary in: (Press release) https://www.fda.gov/regulatory-information/search-fda-guidance-documents/m7r1-assessment-and-control-dna-reactive-mutagenic-impurities-pharmaceuticals-limit-potential.
{{cite press release}}: Missing or empty|title=(help)
- Lay summary in: (Press release) https://www.fda.gov/regulatory-information/search-fda-guidance-documents/m7r1-assessment-and-control-dna-reactive-mutagenic-impurities-pharmaceuticals-limit-potential.
- ↑ "Nitrosamine impurities". European Medicines Agency. 23 October 2019. Archived from the original on 4 August 2020. Retrieved 6 August 2020. Text was copied from this source which is © European Medicines Agency. Reproduction is authorized provided the source is acknowledged.
- 1 2 3 4 5 "Nitrosamines: EMA aligns recommendations for sartans with those other medicines". European Medicines Agency (EMA) (Press release). 12 November 2020. Archived from the original on 13 November 2020. Retrieved 13 November 2020. Text was copied from this source which is © European Medicines Agency. Reproduction is authorized provided the source is acknowledged.
- ↑ "Angiotensin-II-receptor antagonists (sartans) containing a tetrazole group". European Medicines Agency (EMA). Archived from the original on 11 November 2020. Retrieved 13 November 2020.
- ↑ Benigni A, Corna D, Zoja C, Sonzogni A, Latini R, Salio M, et al. (March 2009). "Disruption of the Ang II type 1 receptor promotes longevity in mice". The Journal of Clinical Investigation. 119 (3): 524–30. doi:10.1172/JCI36703. PMC 2648681. PMID 19197138.
- ↑ Cassis P, Conti S, Remuzzi G, Benigni A (January 2010). "Angiotensin receptors as determinants of life span". Pflugers Archiv. 459 (2): 325–32. doi:10.1007/s00424-009-0725-4. PMID 19763608. S2CID 24404339.
External links
- Angiotensin II Type 1 Receptor Blockers at the US National Library of Medicine Medical Subject Headings (MeSH)