Pneumoperitoneum
| Pneumoperitoneum | |
|---|---|
| Other names: Aeroperitoneum[1] | |
 | |
| Chest X-ray with air between the right diaphragm and the liver (green and red arrows). Air also visible below the diaphragm on the persons left. Blue arrows mark a normal gas filled colon. | |
| Specialty | General surgery |
| Symptoms | None to peritonitis[2] |
| Complications | Abdominal compartment syndrome[3] |
| Causes | Gastrointestinal tract perforation, abdominal surgery, peritoneal dialysis, pneumothorax, pneumomediastinum, mechanical ventilation, entry via the vagina[1][4] |
| Diagnostic method | X-ray, CT scan[2] |
| Differential diagnosis | Chilaiditi syndrome, pneumomediastinum, atelectasis of the lower lung, bowel wall gas[5] |
| Treatment | Based on cause, often surgery[6][4] |
Pneumoperitoneum is the presence of air or other gas in the peritoneal cavity.[1] Symptoms may vary from none to peritonitis.[2] Other symptoms may include abdominal swelling or shortness of breath.[2] Complications may rarely include abdominal compartment syndrome.[3]
The most common cause (>90%) is a hole in the gastrointestinal tract.[1][4] This may occur due to a peptic ulcer, bowel obstruction, appendicitis, or abdominal trauma.[1] Other causes may include following abdominal surgery, including laparoscopic surgery; peritoneal dialysis, pneumothorax, pneumomediastinum, mechanical ventilation, and entry via the vagina.[1] Rarely cases may occur due to an unknown cause.[4] Diagnosis is generally via X-ray or CT scan.[2]
Treatment depends on the source of the air.[6] In most cases surgery is required; though certain cases may be managed conservatively.[4][7] Conservative management may include bowel rest, intravenous antibiotics, and closely watching for worsening.[2] Cases were detected via X-ray as early as 1915.[4]
Signs and symptoms
The presentation often involves:[8]
- Nausea
- Abdominal pain
- Chest pain
Causes
- Perforated duodenal ulcer – The most common cause of rupture in the abdomen. Especially of the anterior aspect of the first part of the duodenum.
- Perforated peptic ulcer[9]
- Bowel obstruction[10][11]
- Ruptured diverticulum[12]
- Penetrating trauma[13]
- Ruptured inflammatory bowel disease (e.g., megacolon)[14]
- Necrotising enterocolitis/pneumatosis coli[15]
- Bowel cancer[16]
- Ischemic bowel[17][18][19]
- Steroids
- After laparotomy
- After laparoscopy
- Breakdown of a surgical anastomosis
- Bowel injury after endoscopy
- Peritoneal dialysis (PD), although the prevalence of pneumoperitoneum is estimated to be less than 4% among people with PD in a more recent study in the United Kingdom.[20]
- Vaginal insufflation (air enters via the fallopian tubes; e.g., water-skiing,[21] oral sex[22][23])
- Colonic or peritoneal infection
- From chest (e.g., bronchopleural fistula)
- Non-invasive PAP (positive airway pressure) can force air down duodenum as well as down trachea.
Spontaneous
Spontaneous cases are rare and not caused by an abdominal organ rupture. This is called idiopathic when the cause is not known.[24] Causes of a spontaneous pneumoperitoneum, with no peritonitis include barotrauma due to mechanical ventilation, and tracheal rupture following an emergency intubation. In the ventilation case, air had passed from the chest into the abdominal cavity through the diaphragm. In the tracheal rupture air had passed along the great vessels.[25]
Diagnosis
When present, pneumoperitoneum can often be seen on projectional radiography, but small amounts are often missed, and CT scan is nowadays regarded as a criterion standard in the assessment of a pneumoperitoneum.[26] CT can visualize quantities as small as 5 cm³ of air or gas.
Signs that can be seen on projectional radiography are shown below:
The double wall sign marks the presence of air on both sides of the intestine.[27] However, a false double wall sign can result from two loops of bowel being in contact with one another.[28] The sign is named after Leo George Rigler.[29] It is not the same as Rigler's triad.
The football sign is when the abdomen appears as a large oval radiolucency reminiscent of an American football on a supine projectional radiograph.[30] The football sign is most frequently seen in infants with spontaneous or iatrogenic gastric perforation causing pneumoperitoneum. It is also seen in bowel obstruction with secondary perforation, as in Hirschprung disease, midgut volvulus, meconium ileus and intestinal atresia. Iatrogenic causes like endoscopic perforation may also give football sign.
The Cupola sign is seen when air is accumulated under the central tendon of the diaphragm.[31]
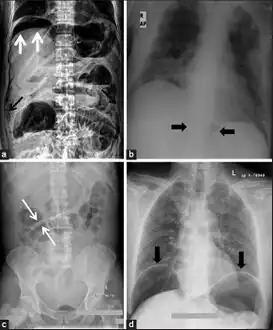 a) X-ray of abdomen, showing subdiaphragmatic free air, air outlining the properitoneal fat stripe black arrows b) Cupola sign arrowheads c) Rigler's sign d) chest radiograph showing free air under the diaphragms
a) X-ray of abdomen, showing subdiaphragmatic free air, air outlining the properitoneal fat stripe black arrows b) Cupola sign arrowheads c) Rigler's sign d) chest radiograph showing free air under the diaphragms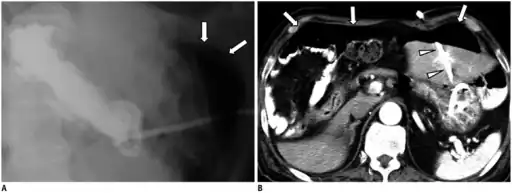 a.b)Pneumoperitoneum developed three days following percutaneous radiologic gastrostomy
a.b)Pneumoperitoneum developed three days following percutaneous radiologic gastrostomy Another pneumoperitoneum on chest X-ray.
Another pneumoperitoneum on chest X-ray.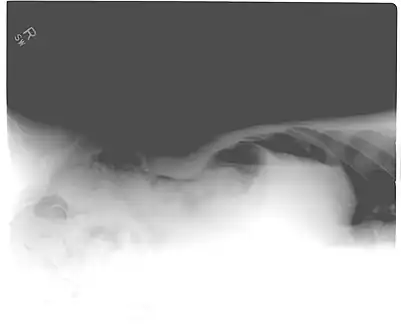 Pneumoperitoneum seen on X-ray with the patient lying on his left side.
Pneumoperitoneum seen on X-ray with the patient lying on his left side. Double wall sign. This is a secondary sign of pneumoperitoneum. Patient is supine, and air within the abdomen and lumen of the bowel accentuate both sides of the bowel wall.
Double wall sign. This is a secondary sign of pneumoperitoneum. Patient is supine, and air within the abdomen and lumen of the bowel accentuate both sides of the bowel wall.- Ultrasound finding of pneumoperitoneum known as "peritoneal stripe sign"[32]
Differential diagnosis

As differential diagnoses, a subphrenic abscess, bowel interposed between diaphragm and liver (Chilaiditi syndrome), and linear atelectasis at the base of the lungs can simulate free air under the diaphragm on a chest X-ray.
Treatment
Treatment depends on the cause.
Terminology
Pneumoperitoneum can be described as peritoneal emphysema,[33] just as pneumomediastinum can be called mediastinal emphysema, but pneumoperitoneum is the usual name.
See also
References
- 1 2 3 4 5 6 Jones, Jeremy. "Pneumoperitoneum | Radiology Reference Article | Radiopaedia.org". Radiopaedia. Archived from the original on 2 February 2023. Retrieved 31 January 2023.
- 1 2 3 4 5 6 Ramponi, DR (2018). "Pneumoperitoneum". Advanced emergency nursing journal. 40 (2): 87–93. doi:10.1097/TME.0000000000000189. PMID 29715250.
- 1 2 Eltorai, Adam E. M.; Hyman, Charles H.; Healey, Terrance T. (18 December 2019). Essential Radiology Review: A Question and Answer Guide. Springer Nature. p. 306. ISBN 978-3-030-26044-6. Archived from the original on 2 February 2023. Retrieved 31 January 2023.
- 1 2 3 4 5 6 Williams, NM; Watkin, DF (September 1997). "Spontaneous pneumoperitoneum and other nonsurgical causes of intraperitoneal free gas". Postgraduate medical journal. 73 (863): 531–7. doi:10.1136/pgmj.73.863.531. PMID 9373590.
- 1 2 Jones, Jeremy. "Pseudopneumoperitoneum | Radiology Reference Article | Radiopaedia.org". Radiopaedia. Archived from the original on 2 February 2023. Retrieved 31 January 2023.
- 1 2 Tanner, TN; Hall, BR; Oran, J (October 2018). "Pneumoperitoneum". The Surgical clinics of North America. 98 (5): 915–932. doi:10.1016/j.suc.2018.06.004. PMID 30243453.
- ↑ Mularski, RA; Sippel, JM; Osborne, ML (July 2000). "Pneumoperitoneum: a review of nonsurgical causes". Critical care medicine. 28 (7): 2638–44. doi:10.1097/00003246-200007000-00078. PMID 10921609.
- ↑ Martin, Ronald F.; Schenarts, Paul J. (24 September 2018). Emergency General Surgery, An Issue of Surgical Clinics. Elsevier Health Sciences. ISBN 978-0-323-64100-5. Archived from the original on 4 August 2022. Retrieved 28 July 2022.
- ↑ "Peptic Ulcer Disease". The Lecturio Medical Concept Library. Archived from the original on 10 August 2021. Retrieved 10 August 2021.
- ↑ "Large Bowel Obstruction". The Lecturio Medical Concept Library. Archived from the original on 11 July 2021. Retrieved 10 August 2021.
- ↑ "Small Bowel Obstruction". The Lecturio Medical Concept Library. Archived from the original on 11 July 2021. Retrieved 10 August 2021.
- ↑ "diverticulum | Definition of diverticulum in English by Lexico Dictionaries". Lexico Dictionaries | English. Archived from the original on 2021-11-02. Retrieved 2019-07-17.
- ↑ Stewart MG (2005). "Principles of ballistics and penetrating trauma". In Stewart MG (ed.). Head, Face, and Neck Trauma: Comprehensive Management. Thieme. pp. 188–94. ISBN 3-13-140331-4. Archived from the original on 2021-08-10. Retrieved 2008-06-12.
- ↑ "Megacolon". The Lecturio Medical Concept Library. Archived from the original on 27 July 2021. Retrieved 10 August 2021.
- ↑ Necrotizing Enterocolitis Archived 2020-08-29 at the Wayback Machine Bugs, Drugs and Things That Go Bump in the Night
- ↑ "Colon Cancer Treatment (PDQ®)". NCI. May 12, 2014. Archived from the original on July 5, 2014. Retrieved June 29, 2014.
- ↑ Higgins PD, Davis KJ, Laine L (April 2004). "Systematic review: the epidemiology of ischaemic colitis". Alimentary Pharmacology & Therapeutics. 19 (7): 729–38. doi:10.1111/j.1365-2036.2004.01903.x. hdl:2027.42/74164. PMID 15043513. S2CID 9575677.
- ↑ Brandt LJ, Boley SJ (May 2000). "AGA technical review on intestinal ischemia. American Gastrointestinal Association". Gastroenterology. 118 (5): 954–68. doi:10.1016/S0016-5085(00)70183-1. PMID 10784596.
- ↑ American Gastroenterological Association (May 2000). "American Gastroenterological Association Medical Position Statement: guidelines on intestinal ischemia". Gastroenterology. 118 (5): 951–3. doi:10.1016/S0016-5085(00)70182-X. PMID 10784595. Archived from the original on 2007-09-27.
- ↑ Imran M, Bhat R, Anijeet H (April 2011). "Pneumoperitoneum in peritoneal dialysis patients; one centre's experience". NDT Plus. 4 (2): 120–3. doi:10.1093/ndtplus/sfq208. PMC 4421564. PMID 25984130.
- ↑ Kizer KW (May 1980). "Medical hazards of the water skiing douche". Annals of Emergency Medicine. 9 (5): 268–9. doi:10.1016/s0196-0644(80)80387-8. PMID 7369581.
Many injuries can result from water skiing accidents, but the water skiing "douche" is unique to this sport. Although generally causing only discomfort, significant trauma can result from the forceful entry of water into the various body orifices.
- ↑ Jacobs VR, Mundhenke C, Maass N, Hilpert F, Jonat W (Oct 2000). "Sexual activity as cause for non-surgical pneumoperitoneum". JSLS. 4 (4): 297–300. PMC 3113190. PMID 11051188.
- ↑ Cawich SO, Johnson PB, Williams E, Naraynsingh V (25 Sep 2013). "Non-surgical pneumoperitoneum after oro-genital intercourse". International Journal of Surgery Case Reports. 4 (11): 1048–51. doi:10.1016/j.ijscr.2013.08.022. PMC 3825970. PMID 24121052.
- ↑ Pfister J, Riedtmann-Klee HJ (September 1993). "[Idiopathic spontaneous pneumoperitoneum. Case discussion based on two cases, assessment procedure and therapy and review of the literature]". Helvetica Chirurgica Acta. 60 (1–2): 49–56. PMID 8226082.
- ↑ Gutkin Z, Iellin A, Meged S, Sorkine P, Geller E (July 1992). "Spontaneous pneumoperitoneum without peritonitis". International Surgery. 77 (3): 219–23. PMID 1399374.
- ↑ Khan AN, Chandramohan M (2017-12-06). Coombs BD, Gay SD (eds.). "Pneumoperitoneum Imaging". Emedicine, Medscape. WebMD LLC. Archived from the original on 2016-02-23. Retrieved 2022-05-17.
- ↑ Harkin DW, Blake G (March 1999). "Small bowel obstruction in a young adult". Postgraduate Medical Journal. 75 (881): 173–5. doi:10.1136/pgmj.75.881.173. PMC 1741173. PMID 10448501.
- ↑ de Lacey G, Bloomberg T, Wignall BK (July 1977). "Pneumoperitoneum: the misleading double wall sign". Clinical Radiology. 28 (4): 445–8. doi:10.1016/s0009-9260(77)80161-x. PMID 872511.
- ↑ Hirsch M, Cortés C (2009). "El signo de Leo Rigler: doble pared en neumoperitoneo" [The sign of Leo Rigler: double pared in neumoperitoneo.]. Revista chilena de radiología (in Spanish). 15 (3): 152–4. doi:10.4067/S0717-93082009000300008.
{{cite journal}}: CS1 maint: unrecognized language (link) - ↑ Rampton JW (April 2004). "The football sign". Radiology. 231 (1): 81–2. doi:10.1148/radiol.2311011290. PMID 14990817.
- ↑ Sureka B, Bansal K, Arora A (2015). "Pneumoperitoneum: What to look for in a radiograph?". Journal of Family Medicine and Primary Care. 4 (3): 477–8. doi:10.4103/2249-4863.161369. PMC 4535122. PMID 26288798.
- ↑ "UOTW #68 - Ultrasound of the Week". Ultrasound of the Week. 22 March 2016. Archived from the original on 7 July 2016. Retrieved 27 May 2017.
- ↑ Marian K, Monika K, Bartosz K (March 2015). "Spontaneous pneumoperitoneum in a patient after ventilation therapy". Polski Przeglad Chirurgiczny. 86 (12): 601–3. doi:10.1515/pjs-2015-0008. PMID 25803061.
External links
| Classification | |
|---|---|
| External resources |