Helicobacter pylori
| Helicobacter pylori infection | |
|---|---|
| Other names: H. pylori infection, Campylobacter pylori | |
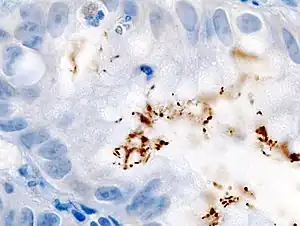 | |
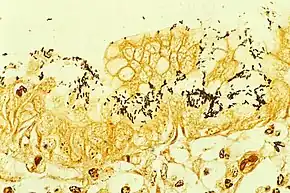
| Immunohistochemical staining of H. pylori (brown) from a gastric biopsy | |
| Pronunciation | |
| Specialty | Infectious disease, gastroenterology |
| Symptoms | Abdominal pain, nausea, heart burn[3] |
| Complications | Gastritis, stomach ulcers, stomach cancer[4] |
| Causes | Helicobacter pylori, spread by fecal-oral or oral–oral route[4] |
| Diagnostic method | Urea breath test, fecal antigen assay, rapid urease test, tissue biopsy[4] |
| Differential diagnosis | Celiac disease, Crohn disease, NSAID use, lactose intolerance[3] |
| Medication | Proton pump inhibitor, clarithromycin, amoxicillin, bismuth subsalicylate, metronidazole[5][4] |
| Frequency | 60% (2015)[6] |
Helicobacter pylori infection is an infection, typically of the stomach, by the bacterium Helicobacter pylori.[3] Usually there are no symptoms; but it may result in gastritis (stomach inflammation) in 25% or stomach ulcers in 10%.[4][5] Symptoms may include abdominal pain, nausea, and heart burn.[3] Infection is also associated with atrophic gastritis, gastric cancer, and mucosal associated-lymphoid-type (MALT) lymphoma.[4][3]
It is believed to spread mostly by the fecal-oral and possibly oral-oral route.[4] Risk factors include living in an area were the disease is common and poverty.[4][3] Helicobacter pylori is a gram-negative, microaerophilic, curved rod-shaped bacterium.[4] Diagnosis is by urea breath test, fecal antigen assay, rapid urease test, or tissue biopsy.[4] Serology may indicate a current or past infection.[4]
Cases without symptoms do not require specific treatment.[4] Otherwise the combination of a proton pump inhibitor (PPI), amoxicillin, metronidazole, and clarithromycin may be used.[5] Other options include a PPI, bismuth subsalicylate, metronidazole, and tetracycline.[4] Treatment is generally for 14 days.[4] An H. pylori vaccine is in development as of 2015.[3]
It is estimated that 60% of the world's population were infected in 2015, with this being more common in developing countries.[6][4] Onset is often in childhood.[3] About 5% of children under 10 in the United States are affected.[3] In recent decades, rates have declined in many countries.[7] The bacterium was first identified in 1982 by Australian doctors Barry Marshall and Robin Warren.[8][9]
Signs and symptoms
Up to 90% of people infected with H. pylori never experience symptoms or complications.[10] About 10% to 20% develop peptic ulcers at some point in time.[11][12] Acute infection may appear as gastritis with abdominal pain (stomach ache) or nausea.[13] Where this develops into chronic gastritis, the symptoms, are often those of non-ulcer dyspepsia: stomach pains, nausea, bloating, belching, and sometimes vomiting.[14][15] Pain typically occurs when the stomach is empty, between meals, and in the early morning hours, but it can also occur at other times.
Bleeding in the stomach can also occur, sometimes with the passage of black stools; prolonged bleeding may cause anemia leading to weakness and fatigue. If bleeding is heavy, vomiting blood or burgendy stool may occur. Inflammation of the pyloric antrum, which connects the stomach to the duodenum, is more likely to lead to duodenal ulcers, while inflammation of the body of stomach is more likely to lead to gastric ulcers.[16][17]
Complications
Individuals infected with H. pylori may also develop colorectal[18][19] or stomach[20] polyps, i.e. non-cancerous growths of tissue projecting from the mucous membranes of these organs. Usually, these polyps are asymptomatic but stomach polyps may be the cause of dyspepsia, heartburn, bleeding from the upper gastrointestinal tract, and, rarely, gastric outlet obstruction[20] while colorectal polyps may be the cause of rectal bleeding, anemia, constipation, diarrhea, weight loss, and abdominal pain.[21]
Individuals with chronic infections have an increased risk of cancer (less than 1 in 1,000) that is directly related to this infection.[22][23][11][12][5] These cancers are stomach adenocarcinoma, less commonly diffuse large B-cell lymphoma of the stomach,[24] or extranodal marginal zone B-cell lymphomas of the stomach,[25][26] or, more rarely, of the colon,[23][26] rectum,[27] esophagus,[28] or ocular adenexa (i.e. orbit, conjunctiva, or eyelids).[29][30]
Transmission
Helicobacter pylori is contagious, although the exact route of transmission is not known.[31][32] Person-to-person transmission by either the oral–oral (kissing, mouth feeding) or fecal–oral route is most likely. Consistent with these transmission routes, the bacteria have been isolated from feces, saliva, and dental plaque of some infected people. Findings suggest H. pylori is more easily transmitted by gastric mucus than saliva.[33] Transmission occurs mainly within families in developed nations, yet can also be acquired from the community in developing countries.[34] H. pylori may also be transmitted orally by means of fecal matter through the ingestion of waste-tainted water, so a hygienic environment could help decrease the risk of H. pylori infection.[33]
Microbiology
| Helicobacter pylori | |
|---|---|
 | |
| Electron micrograph of H. pylori possessing multiple flagella (negative staining) | |
| Scientific classification | |
| Domain: | Bacteria |
| Phylum: | Campylobacterota |
| Class: | "Campylobacteria" |
| Order: | Campylobacterales |
| Family: | Helicobacteraceae |
| Genus: | Helicobacter |
| Species: | H. pylori |
| Binomial name | |
| Helicobacter pylori (Marshall et al. 1985) Goodwin et al., 1989 | |
| Synonyms | |
| |
Morphology
Helicobacter pylori is a helix-shaped (classified as a curved rod, not spirochaete) Gram-negative bacterium about 3 μm long with a diameter of about 0.5 μm . H. pylori can be demonstrated in tissue by Gram stain, Giemsa stain, haematoxylin–eosin stain, Warthin–Starry silver stain, acridine orange stain, and phase-contrast microscopy. It is capable of forming biofilms[35] and can convert from spiral to a possibly viable but nonculturable coccoid form.[36]
Helicobacter pylori has four to six flagella at the same location; all gastric and enterohepatic Helicobacter species are highly motile owing to flagella.[37] The characteristic sheathed flagellar filaments of Helicobacter are composed of two copolymerized flagellins, FlaA and FlaB.[38]
Physiology
Helicobacter pylori is microaerophilic – that is, it requires oxygen, but at lower concentration than in the atmosphere. It contains a hydrogenase that can produce energy by oxidizing molecular hydrogen (H2) made by intestinal bacteria.[39] It produces oxidase, catalase, and urease.
H. pylori possesses five major outer membrane protein families.[12] The largest family includes known and putative adhesins. The other four families are porins, iron transporters, flagellum-associated proteins, and proteins of unknown function. Like other typical Gram-negative bacteria, the outer membrane of H. pylori consists of phospholipids and lipopolysaccharide (LPS). The O antigen of LPS may be fucosylated and mimic Lewis blood group antigens found on the gastric epithelium.[12] The outer membrane also contains cholesterol glucosides, which are present in few other bacteria.[12]
Genome
Helicobacter pylori consists of a large diversity of strains, and hundreds of genomes have been completely sequenced.[40][41][42][43][44][45] The genome of the strain "26695" consists of about 1.7 million base pairs, with some 1,576 genes. The pan-genome, that is a combined set of 30 sequenced strains, encodes 2,239 protein families (orthologous groups, OGs). Among them, 1,248 OGs are conserved in all the 30 strains, and represent the universal core. The remaining 991 OGs correspond to the accessory genome in which 277 OGs are unique (i.e., OGs present in only one strain).[46]
Transcriptome
In 2010, Sharma et al. presented a comprehensive analysis of transcription at single-nucleotide resolution by differential RNA-seq that confirmed the known acid induction of major virulence loci, such as the urease (ure) operon or the cag pathogenicity island (see below).[47] More importantly, this study identified a total of 1,907 transcriptional start sites, 337 primary operons, and 126 additional suboperons, and 66 monocistrons. Until 2010, only about 55 transcriptional start sites (TSSs) were known in this species. Notably, 27% of the primary TSSs are also antisense TSSs, indicating that – similar to E. coli – antisense transcription occurs across the entire H. pylori genome. At least one antisense TSS is associated with about 46% of all open reading frames, including many housekeeping genes.[47] Most (about 50%) of the 5′ UTRs are 20–40 nucleotides (nt) in length and support the AAGGag motif located about 6 nt (median distance) upstream of start codons as the consensus Shine–Dalgarno sequence in H. pylori.[47]
Genes involved in virulence and pathogenesis
Study of the H. pylori genome is centered on attempts to understand pathogenesis, the ability of this organism to cause disease. About 29% of the loci have a colonization defect when mutated. Two of sequenced strains have an around 40 kb-long Cag pathogenicity island (a common gene sequence believed responsible for pathogenesis) that contains over 40 genes. This pathogenicity island is usually absent from H. pylori strains isolated from humans who are carriers of H. pylori, but remain asymptomatic.[48]
The cagA gene codes for one of the major H. pylori virulence proteins. Bacterial strains with the cagA gene are associated with an ability to cause ulcers.[49] The cagA gene codes for a relatively long (1186-amino acid) protein. The cag pathogenicity island (PAI) has about 30 genes, part of which code for a complex type IV secretion system. The low GC-content of the cag PAI relative to the rest of the Helicobacter genome suggests the island was acquired by horizontal transfer from another bacterial species.[40] The serine protease HtrA also plays a major role in the pathogenesis of H. pylori. The HtrA protein enables the bacterium to transmigrate across the host cells' epithelium, and is also needed for the translocation of CagA.[50]
The vacA (Q48245) gene codes for another major H. pylori virulence protein. There are four main subtypes of vacA: s1/m1, s1/m2, s2/m1, and s2/m2. s1/m1 and s1/m2 subtypes are known to cause increased risk of gastric cancer.[51] This has been linked to the ability for toxigenic vacA to promote the generation of intracellular reservoirs of H. pylori via disruption of calcium channel TRPML1.[52]
Proteome
The proteins of H. pylori have been systematically analyzed by multiple studies. As a consequence, more than 70% of its proteome have been detected by mass spectrometry and other biochemical methods. In fact, about 50% of the proteome have been quantified, that is, we know how many copies of each protein are present in a typical cell.[53] Furthermore, the interactome of H. pylori has been systematically studied and more than 3000 protein-protein interactions have been identified. The latter provide information of how proteins interact with each other, e.g. in stable protein complexes or in more dynamic, transient interactions. This in turn helps researchers to find out what the function of uncharacterized proteins is, e.g. when an uncharacterized protein interacts with several proteins of the ribosome (that is, it is likely also involved in ribosome function). Nevertheless, about a third of all ~1,500 proteins in H. pylori remain uncharacterized and their function is largely unknown.[54]
Pathophysiology
Adaptation to the stomach
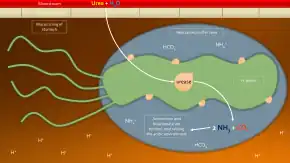
_Crossing_Mucus_Layer_of_Stomach.jpg.webp)
To avoid the acidic environment of the interior of the stomach (lumen), H. pylori uses its flagella to burrow into the mucus lining of the stomach to reach the epithelial cells underneath, where it is less acidic.[55] H. pylori is able to sense the pH gradient in the mucus and move towards the less acidic region (chemotaxis). This also keeps the bacteria from being swept away into the lumen with the bacteria's mucus environment, which is constantly moving from its site of creation at the epithelium to its dissolution at the lumen interface.[56]
H. pylori is found in the mucus, on the inner surface of the epithelium, and occasionally inside the epithelial cells themselves.[57] It adheres to the epithelial cells by producing adhesins, which bind to lipids and carbohydrates in the epithelial cell membrane. One such adhesin, BabA, binds to the Lewis b antigen displayed on the surface of stomach epithelial cells.[58] H. pylori adherence via BabA is acid sensitive and can be fully reversed by decreased pH. It has been proposed that BabA's acid responsiveness enables adherence while also allowing an effective escape from unfavorable environment at pH that is harmful to the organism.[59] Another such adhesin, SabA, binds to increased levels of sialyl-Lewis x antigen expressed on gastric mucosa.[60]
In addition to using chemotaxis to avoid areas of low pH, H. pylori also neutralizes the acid in its environment by producing large amounts of urease, which breaks down the urea present in the stomach to carbon dioxide and ammonia. These react with the strong acids in the environment to produce a neutralized area around H. pylori.[61] Urease knockout mutants are incapable of colonization. In fact, urease expression is not only required for establishing initial colonization but also for maintaining chronic infection.[62]
Adaptation of H. pylori to high acidity of stomach
As mentioned above, H. pylori produce large amounts of urease to produce ammonia as one of its adaptation methods to overcome stomach acidity. Helicobacter pylori arginase, a bimetallic enzyme binuclear Mn2-metalloenzyme arginase, crucial for pathogenesis of the bacterium in human stomach,[63] a member of the ureohydrolase family, catalyzes the conversion of L-arginine to L-ornithine and urea, where ornithine is further converted into polyamines, which are essential for various critical metabolic processes.[63]
This provides acid resistance and is thus important for colonization of the bacterium in the gastric epithelial cells. Arginase of H. pylori also plays a role in evasion of the pathogen from the host immune system mainly by various proposed mechanisms, arginase competes with host-inducible nitric oxide (NO) synthase for the common substrate L-arginine, and thus reduces the synthesis of NO, an important component of innate immunity and an effective antimicrobial agent that is able to kill the invading pathogens directly.[63]
Alterations in the availability of L-arginine and its metabolism into polyamines contribute significantly to the dysregulation of the host immune response to H. pylori infection.[63]
Inflammation, gastritis and ulcer
Helicobacter pylori harms the stomach and duodenal linings by several mechanisms. The ammonia produced to regulate pH is toxic to epithelial cells, as are biochemicals produced by H. pylori such as proteases, vacuolating cytotoxin A (VacA) (this damages epithelial cells, disrupts tight junctions and causes apoptosis), and certain phospholipases.[64] Cytotoxin associated gene CagA can also cause inflammation and is potentially a carcinogen.[65]
Colonization of the stomach by H. pylori can result in chronic gastritis, an inflammation of the stomach lining, at the site of infection. Helicobacter cysteine-rich proteins (Hcp), particularly HcpA (hp0211), are known to trigger an immune response, causing inflammation.[66] H. pylori has been shown to increase the levels of COX2 in H. pylori positive gastritis.[67] Chronic gastritis is likely to underlie H. pylori-related diseases.[68]
Ulcers in the stomach and duodenum result when the consequences of inflammation allow stomach acid and the digestive enzyme pepsin to overwhelm the mechanisms that protect the stomach and duodenal mucous membranes. The location of colonization of H. pylori, which affects the location of the ulcer, depends on the acidity of the stomach.[69] In people producing large amounts of acid, H. pylori colonizes near the pyloric antrum (exit to the duodenum) to avoid the acid-secreting parietal cells at the fundus (near the entrance to the stomach).[12] In people producing normal or reduced amounts of acid, H. pylori can also colonize the rest of the stomach.
The inflammatory response caused by bacteria colonizing near the pyloric antrum induces G cells in the antrum to secrete the hormone gastrin, which travels through the bloodstream to parietal cells in the fundus.[70] Gastrin stimulates the parietal cells to secrete more acid into the stomach lumen, and over time increases the number of parietal cells, as well.[71] The increased acid load damages the duodenum, which may eventually result in ulcers forming in the duodenum.
When H. pylori colonizes other areas of the stomach, the inflammatory response can result in atrophy of the stomach lining and eventually ulcers in the stomach. This also may increase the risk of stomach cancer.[16]
Cag pathogenicity island
The pathogenicity of H. pylori may be increased by genes of the cag pathogenicity island; about 50–70% of H. pylori strains in Western countries carry it.[72] Western people infected with strains carrying the cag PAI have a stronger inflammatory response in the stomach and are at a greater risk of developing peptic ulcers or stomach cancer than those infected with strains lacking the island.[12] Following attachment of H. pylori to stomach epithelial cells, the type IV secretion system expressed by the cag PAI "injects" the inflammation-inducing agent, peptidoglycan, from their own cell walls into the epithelial cells. The injected peptidoglycan is recognized by the cytoplasmic pattern recognition receptor (immune sensor) Nod1, which then stimulates expression of cytokines that promote inflammation.[73]
The type-IV secretion apparatus also injects the cag PAI-encoded protein CagA into the stomach's epithelial cells, where it disrupts the cytoskeleton, adherence to adjacent cells, intracellular signaling, cell polarity, and other cellular activities.[74] Once inside the cell, the CagA protein is phosphorylated on tyrosine residues by a host cell membrane-associated tyrosine kinase (TK). CagA then allosterically activates protein tyrosine phosphatase/protooncogene Shp2.[75] Pathogenic strains of H. pylori have been shown to activate the epidermal growth factor receptor (EGFR), a membrane protein with a TK domain. Activation of the EGFR by H. pylori is associated with altered signal transduction and gene expression in host epithelial cells that may contribute to pathogenesis. A C-terminal region of the CagA protein (amino acids 873–1002) has also been suggested to be able to regulate host cell gene transcription, independent of protein tyrosine phosphorylation.[48][49] A great deal of diversity exists between strains of H. pylori, and the strain that infects a person can predict the outcome.
Cancer
Two related mechanisms by which H. pylori could promote cancer are under investigation. One mechanism involves the enhanced production of free radicals near H. pylori and an increased rate of host cell mutation. The other proposed mechanism has been called a "perigenetic pathway",[76] and involves enhancement of the transformed host cell phenotype by means of alterations in cell proteins, such as adhesion proteins. H. pylori has been proposed to induce inflammation and locally high levels of TNF-α and/or interleukin 6 (IL-6). According to the proposed perigenetic mechanism, inflammation-associated signaling molecules, such as TNF-α, can alter gastric epithelial cell adhesion and lead to the dispersion and migration of mutated epithelial cells without the need for additional mutations in tumor suppressor genes, such as genes that code for cell adhesion proteins.[77]
The strain of H. pylori a person is exposed to may influence the risk of developing gastric cancer. Strains of H. pylori that produce high levels of two proteins, vacuolating toxin A (VacA) and the cytotoxin-associated gene A (CagA), appear to cause greater tissue damage than those that produce lower levels or that lack those genes completely.[78] These proteins are directly toxic to cells lining the stomach and signal strongly to the immune system that an invasion is under way. As a result of the bacterial presence, neutrophils and macrophages set up residence in the tissue to fight the bacteria assault.[79]
H. pylori is a major source of worldwide cancer mortality.[80] Although the data varies between different countries, overall about 1% to 3% of people infected with Helicobacter pylori develop gastric cancer in their lifetime compared to 0.13% of individuals who have had no H. pylori infection.[81][12] H. pylori infection is very prevalent. As evaluated in 2002, it is present in the gastric tissues of 74% of middle-aged adults in developing countries and 58% in developed countries.[82] Since 1% to 3% of infected individuals are likely to develop gastric cancer,[83] H. pylori-induced gastric cancer is the third highest cause of worldwide cancer mortality as of 2018.[80]
Infection by H. pylori causes no symptoms in about 80% of those infected.[84] About 75% of individuals infected with H. pylori develop gastritis.[85] Thus, the usual consequence of H. pylori infection is chronic asymptomatic gastritis.[86] Because of the usual lack of symptoms, when gastric cancer is finally diagnosed it is often fairly advanced. More than half of gastric cancer patients have lymph node metastasis when they are initially diagnosed.[87]
The gastritis caused by H. pylori is accompanied by inflammation, characterized by infiltration of neutrophils and macrophages to the gastric epithelium, which favors the accumulation of pro-inflammatory cytokines and reactive oxygen species/reactive nitrogen species (ROS/RNS).[88] The substantial presence of ROS/RNS causes DNA damage including 8-oxo-2'-deoxyguanosine (8-OHdG).[88] If the infecting H. pylori carry the cytotoxic cagA gene (present in about 60% of Western isolates and a higher percentage of Asian isolates), they can increase the level of 8-OHdG in gastric cells by 8-fold, while if the H. pylori do not carry the cagA gene, the increase in 8-OHdG is about 4-fold.[89] In addition to the oxidative DNA damage 8-OHdG, H. pylori infection causes other characteristic DNA damages including DNA double-strand breaks.[90]
H. pylori also causes many epigenetic alterations linked to cancer development.[91][92] These epigenetic alterations are due to H. pylori-induced methylation of CpG sites in promoters of genes[91] and H. pylori-induced altered expression of multiple microRNAs.[92]
As reviewed by Santos and Ribeiro[93] H. pylori infection is associated with epigenetically reduced efficiency of the DNA repair machinery, which favors the accumulation of mutations and genomic instability as well as gastric carcinogenesis. In particular, Raza et al.[94] showed that expression of two DNA repair proteins, ERCC1 and PMS2, was severely reduced once H. pylori infection had progressed to cause dyspepsia. Dyspepsia occurs in about 20% of infected individuals.[95] In addition, as reviewed by Raza et al.,[94] human gastric infection with H. pylori causes epigenetically reduced protein expression of DNA repair proteins MLH1, MGMT and MRE11. Reduced DNA repair in the presence of increased DNA damage increases carcinogenic mutations and is likely a significant cause of H. pylori carcinogenesis.
Survival of H. pylori
The pathogenesis of H. pylori depends on its ability to survive in the harsh gastric environment characterized by acidity, peristalsis, and attack by phagocytes accompanied by release of reactive oxygen species.[96] In particular, H. pylori elicits an oxidative stress response during host colonization. This oxidative stress response induces potentially lethal and mutagenic oxidative DNA adducts in the H. pylori genome.[97]
Vulnerability to oxidative stress and oxidative DNA damage occurs commonly in many studied bacterial pathogens, including Neisseria gonorrhoeae, Hemophilus influenzae, Streptococcus pneumoniae, S. mutans, and H. pylori.[98] For each of these pathogens, surviving the DNA damage induced by oxidative stress appears supported by transformation-mediated recombinational repair. Thus, transformation and recombinational repair appear to contribute to successful infection.
Transformation (the transfer of DNA from one bacterial cell to another through the intervening medium) appears to be part of an adaptation for DNA repair. H. pylori is naturally competent for transformation. While many organisms are competent only under certain environmental conditions, such as starvation, H. pylori is competent throughout logarithmic growth.[99] All organisms encode genetic programs for response to stressful conditions including those that cause DNA damage.[99] In H. pylori, homologous recombination is required for repairing DNA double-strand breaks (DSBs). The AddAB helicase-nuclease complex resects DSBs and loads RecA onto single-strand DNA (ssDNA), which then mediates strand exchange, leading to homologous recombination and repair. The requirement of RecA plus AddAB for efficient gastric colonization suggests, in the stomach, H. pylori is either exposed to double-strand DNA damage that must be repaired or requires some other recombination-mediated event. In particular, natural transformation is increased by DNA damage in H. pylori, and a connection exists between the DNA damage response and DNA uptake in H. pylori,[99] suggesting natural competence contributes to persistence of H. pylori in its human host and explains the retention of competence in most clinical isolates.
RuvC protein is essential to the process of recombinational repair, since it resolves intermediates in this process termed Holliday junctions. H. pylori mutants that are defective in RuvC have increased sensitivity to DNA-damaging agents and to oxidative stress, exhibit reduced survival within macrophages, and are unable to establish successful infection in a mouse model.[100] Similarly, RecN protein plays an important role in DSB repair in H. pylori.[101] An H. pylori recN mutant displays an attenuated ability to colonize mouse stomachs, highlighting the importance of recombinational DNA repair in survival of H. pylori within its host.[101]
Diagnosis
Colonization with H. pylori is not a disease in itself, but a condition associated with a number of disorders of the upper gastrointestinal tract.[12] Testing is recommended if peptic ulcer disease or low-grade gastric MALT lymphoma (MALToma) is present, after endoscopic resection of early gastric cancer, for first-degree relatives with gastric cancer, and in certain cases of dyspepsia.[102] Several methods of testing exist, including invasive and noninvasive testing methods.
Noninvasive tests for H. pylori infection include blood antibody tests, stool antigen tests, or the carbon urea breath test (in which the person drinks 14C – or 13C-labelled urea, which the bacterium metabolizes, producing labelled carbon dioxide that can be detected in the breath).[102][103] It is not known which non-invasive test is more accurate, and the significance of the levels obtained with these tests is not clear.[103] The blood antigen test cannot seperate between current and past infection.[5] Taking a proton pump inhibitor in the last two weeks can make the breath test and the stool antigen test falsely negative.[5]
An endoscopic biopsy is an invasive means to test for H. pylori infection. Low-level infections can be missed by biopsy, so multiple samples are recommended. The most accurate method for detecting H. pylori infection is with a histological examination from two sites after endoscopic biopsy, combined with either a rapid urease test or microbial culture.[104]
Retesting to confirm eradication of the infection may occur at least 4 weeks after stopping antibiotics and at least two weeks after stopping proton pump inhibitors.[3]
Prevention
Due to H. pylori’s role as a major cause of certain diseases and its consistently increasing antibiotic resistance, there is a clear need for new therapeutic strategies to prevent or remove the bacterium from colonizing humans.[105]
Vaccine
Efforts to develop an H. pylori vaccine are ongoing.[106] A recombinant H pylori vaccine, which is taken by mouth, has been studied and appears successful in young children in China.[3] Whether a vaccine would just be preventative or could be used after infection is unclear.[107]
An economic evaluation of the use of a potential H. pylori vaccine in babies found its introduction could, at least in the Netherlands, prove cost-effective for the prevention of peptic ulcer and stomach adenocarcinoma.[108] A similar approach has also been studied for the United States.[109]
Early infection
Many investigations have attempted to prevent the development of Helicobacter pylori-related diseases by eradicating the bacterium during the early stages of its infestation using antibiotics. Studies find that such treatments, when effectively eradicating H. pylori from the stomach, reduce the inflammation and some of the histopathological abnormalities associated with the infestation. However studies disagree on the ability of these treatments to alleviate the more serious histopathological abnormalities in H. pylori infections, e.g. gastric atrophy and metaplasia, both of which are precursors to gastric adenocarcinoma.[110] There is similar disagreement on the ability of antibiotic-based regiments to prevent gastric adenocarcinoma. A review in 2014 found that these regimens did not appear to prevent development of adenocarcinoma.[111] However, two subsequent prospective cohort studies of high-risk individuals in China and Taiwan found that eradication of the bacterium produced a decrease in the number of individuals developing the disease. These results agreed with a retrospective cohort study done in Japan and published in 2016[112] as well as a meta-analysis, also published in 2016, on individuals with varying levels of risk for developing the disease.[113] These more recent studies suggest that the eradication of H. pylori infection reduces the rate of H. pylori-related gastric adenocarcinoma in individuals at all levels of baseline risk.[113] Further studies will be required to clarify this issue. In all events, studies agree that antibiotic-based regimens effectively reduce the occurrence of metachronous H. pylori-associated gastric adenocarcinoma.[110] Metachronous cancers are cancers that reoccur 6 months or later after resection of the original cancer. It is suggested that antibiotic-based drug regimens be used after resecting H. pylori-associated gastric adenocarcinoma in order to reduce its metachronus reoccurrence.[114]
Treatment

Antibiotics
Various antibiotic plus proton pump inhibitor regimens are used to eradicate the bacterium and thereby treat the disorder.[111] As of 2023 concomitant therapy with clarithromycin 500 mg BID, amoxicillin 1 gram BID, metronidazole 500 mg BID, and a proton-pump inhibitor (PPI), such as omeprazole BID, for 14–21 days is often used.[5][115][116] A PPI, bismuth subsalicylate, metronidazole, and tetracycline may also be used.[5]
In areas with higher rates of clarithromycin resistance, other options are recommended.[117] antibiotic resistance may require additional rounds of antibiotic therapy or alternative strategies, such as a quadruple therapy, which adds a bismuth colloid, such as bismuth subsalicylate.[102][118][119] In people with previous macrolide exposure or who are allergic to penicillin, a quadruple therapy consisting of a proton pump inhibitor, bismuth, tetracycline, and a nitroimidazole for 10–14 days is a recommended first-line option.[120] For clarithromycin-resistant strains, levofloxacin as part of the therapy has been suggested.[121][122]
Other measures
Probiotics, when used with standard treatment, do not appear to change outcomes.[3] There is tentative evidence that scaling and root planing may prevent recurrence.[123]
Cancers
Extranodal marginal zone B-cell lymphomas
Extranodal marginal zone B-cell lymphomas (also termed MALT lymphomas) are generally indolent malignancies. Recommended treatment of H. pylori-positive extranodal marginal zone B-cell lymphoma of the stomach, when localized (i.e. Ann Arbor stage I and II), employs one of the antibiotic-proton pump inhibitor regiments listed in the H. pylori eradication protocols. If the initial regimen fails to eradicate the pathogen, patients are treated with an alternate protocol. Eradication of the pathogen is successful in 70–95% of cases.[124] Some 50-80% of patients who experience eradication of the pathogen develop within 3–28 months a remission and long-term clinical control of their lymphoma. Radiation therapy to the stomach and surrounding (i.e. peri-gastric) lymph nodes has also been used to successfully treat these localized cases. Patients with non-localized (i.e. systemic Ann Arbor stage III and IV) disease who are free of symptoms have been treated with watchful waiting or, if symptomatic, with the immunotherapy drug, rituximab, (given for 4 weeks) combined with the chemotherapy drug, chlorambucil, for 6–12 months; 58% of these patients attain a 58% progression-free survival rate at 5 years. Frail stage III/IV patients have been successfully treated with rituximab or the chemotherapy drug, cyclophosphamide, alone.[125] Only rare cases of H. pylori-positive extranodal marginal zone B-cell lymphoma of the colon have been successfully treated with an antibiotic-proton pump inhibitor regimen; the currently recommended treatments for this disease are surgical resection, endoscopic resection, radiation, chemotherapy, or, more recently, rituximab.[23] In the few reported cases of H. pylori-positive extranodal marginal zone B-cell lymphoma of the esophagus, localized disease has been successfully treated with antibiotic-proton pump inhibitor regimens; however, advanced disease appears less responsive or unresponsive to these regimens but partially responsive to rituximab.[28] Antibiotic-proton pump inhibitor eradication therapy and localized radiation therapy have been used successfully to treat H. pylori-positive extranodal marginal zone B-cell lymphomas of the rectum; however radiation therapy has given slightly better results and therefore been suggested to be the disease' preferred treatment.[27] The treatment of localized H. pylori-positive extranodal marginal zone B-cell lymphoma of the ocular adenexa with antibiotic/proton pump inhibitor regimens has achieved 2 year and 5 year failure-free survival rates of 67% and 55%, respectively, and a 5 year progression-free rate of 61%.[29] However, the generally recognized treatment of choice for patients with systemic involvement uses various chemotherapy drugs often combined with rituximab.[126]
Diffuse large B-cell lymphoma
Diffuse large B-cell lymphoma is a far more aggressive cancer than extranodal marginal zone B-cell lymphoma. Cases of this malignancy that are H. pylori-positive may be derived from the latter lymphoma[127] and are less aggressive as well as more susceptible to treatment than H. pylori negative cases.[128][129] Several recent studies strongly suggest that localized, early-stage diffuse Helicobacter pylori positive diffuse large B-cell lymphoma, when limited to the stomach, can be successfully treated with antibiotic-proton pump inhibitor regimens.[24][128][130][129] However, these studies also agree that, given the aggressiveness of diffuse large B-cell lymphoma, patients treated with one of these H. pylori eradication regimes need to be carefully followed. If found unresponsive to or clinically worsening on these regimens, these patients should be switched to more conventional therapy such as chemotherapy (e.g. CHOP or a CHOP-like regimen), immunotherapy (e.g. rituximab), surgery, and/or local radiotherapy.[128] H. pylori positive diffuse large B-cell lymphoma has been successfully treated with one or a combination of these methods.[129]
Stomach adenocarcinoma
Helicobacter pylori is linked to the majority of gastric adenocarcinoma cases, particularly those that are located outside of the stomach's cardia (i.e. esophagus-stomach junction).[112] The treatment for this cancer is highly aggressive with even localized disease being treated sequentially with chemotherapy and radiotherapy before surgical resection.[131] Since this cancer, once developed, is independent of H. pylori infection, antibiotic-proton pump inhibitor regimens are not used in its treatment.[112]
Prognosis
Helicobacter pylori colonizes the stomach and induces chronic gastritis, a long-lasting inflammation of the stomach. The bacterium persists in the stomach for decades in most people. Most individuals infected by H. pylori never experience clinical symptoms, despite having chronic gastritis. About 10–20% of those colonized by H. pylori ultimately develop gastric and duodenal ulcers.[12] H. pylori infection is also associated with a 1–2% lifetime risk of stomach cancer and a less than 1% risk of gastric MALT lymphoma.[12]
In the absence of treatment, H. pylori infection – once established in its gastric niche – is widely believed to persist for life.[33] In the elderly, however, infection likely can disappear as the stomach's mucosa becomes increasingly atrophic and inhospitable to colonization. The proportion of acute infections that persist is not known, but several studies that followed the natural history in populations have reported apparent spontaneous elimination.[132][133]
It is possible for H. pylori to re-establish in a person after eradication. This recurrence can be caused by the original strain (recrudescence), or be caused by a different strain (reinfection). According to a 2017 meta-analysis by Hu et al., the global per-person annual rates of recurrence, reinfection, and recrudescence is 4.3%, 3.1%, and 2.2% resepctively. It is unclear what the main risk factors are.[134]
Mounting evidence suggests H. pylori has an important role in protection from some diseases.[135] The incidence of acid reflux disease, Barrett's esophagus, and esophageal cancer have been rising dramatically at the same time as H. pylori's presence decreases.[136] In 1996, Martin J. Blaser advanced the hypothesis that H. pylori has a beneficial effect by regulating the acidity of the stomach contents.[70][136] The hypothesis is not universally accepted as several randomized controlled trials failed to demonstrate worsening of acid reflux disease symptoms following eradication of H. pylori.[137][138] Nevertheless, Blaser has reasserted his view that H. pylori is a member of the normal flora of the stomach.[139] He postulates that the changes in gastric physiology caused by the loss of H. pylori account for the recent increase in incidence of several diseases, including type 2 diabetes, obesity, and asthma.[139][140] His group has recently shown that H. pylori colonization is associated with a lower incidence of childhood asthma.[141]
Epidemiology
At least half the world's population is infected by the bacterium, making it the most widespread infection in the world.[142] Actual infection rates vary from nation to nation; the developing world has much higher infection rates than the West (Western Europe, North America, Australasia), where rates are estimated to be around 25%.[142]
The age when someone acquires this bacterium seems to influence the pathologic outcome of the infection. People infected at an early age are likely to develop more intense inflammation that may be followed by atrophic gastritis with a higher subsequent risk of gastric ulcer, gastric cancer, or both. Acquisition at an older age brings different gastric changes more likely to lead to duodenal ulcer.[33] Infections are usually acquired in early childhood in all countries.[12] However, the infection rate of children in developing nations is higher than in industrialized nations, probably due to poor sanitary conditions, perhaps combined with lower antibiotics usage for unrelated pathologies. In developed nations, it is currently uncommon to find infected children, but the percentage of infected people increases with age, with about 50% infected for those over the age of 60 compared with around 10% between 18 and 30 years.[142] The higher prevalence among the elderly reflects higher infection rates in the past when the individuals were children rather than more recent infection at a later age of the individual.[12] In the United States, prevalence appears higher in African-American and Hispanic populations, most likely due to socioeconomic factors.[143][144] The lower rate of infection in the West is largely attributed to higher hygiene standards and widespread use of antibiotics. Despite high rates of infection in certain areas of the world, the overall frequency of H. pylori infection is declining.[145] However, antibiotic resistance is appearing in H. pylori; many metronidazole- and clarithromycin-resistant strains are found in most parts of the world.[146]
History
Helicobacter pylori migrated out of Africa along with its human host circa 60,000 years ago.[147] Recent research states that genetic diversity in H. pylori, like that of its host, decreases with geographic distance from East Africa. Using the genetic diversity data, researchers have created simulations that indicate the bacteria seem to have spread from East Africa around 58,000 years ago. Their results indicate modern humans were already infected by H. pylori before their migrations out of Africa, and it has remained associated with human hosts since that time.[148]
H. pylori was first discovered in the stomachs of patients with gastritis and ulcers in 1982 by Drs. Barry Marshall and Robin Warren of Perth, Western Australia. At the time, the conventional thinking was that no bacterium could live in the acid environment of the human stomach. In recognition of their discovery, Marshall and Warren were awarded the 2005 Nobel Prize in Physiology or Medicine.[149]
Before the research of Marshall and Warren, German scientists found spiral-shaped bacteria in the lining of the human stomach in 1875, but they were unable to culture them, and the results were eventually forgotten.[136] The Italian researcher Giulio Bizzozero described similarly shaped bacteria living in the acidic environment of the stomach of dogs in 1893.[150] Professor Walery Jaworski of the Jagiellonian University in Kraków investigated sediments of gastric washings obtained by lavage from humans in 1899. Among some rod-like bacteria, he also found bacteria with a characteristic spiral shape, which he called Vibrio rugula. He was the first to suggest a possible role of this organism in the pathogenesis of gastric diseases. His work was included in the Handbook of Gastric Diseases, but it had little impact, as it was written in Polish.[151] Several small studies conducted in the early 20th century demonstrated the presence of curved rods in the stomachs of many people with peptic ulcers and stomach cancers.[152] Interest in the bacteria waned, however, when an American study published in 1954 failed to observe the bacteria in 1180 stomach biopsies.[153]
Interest in understanding the role of bacteria in stomach diseases was rekindled in the 1970s, with the visualization of bacteria in the stomachs of people with gastric ulcers.[154] The bacteria had also been observed in 1979, by Robin Warren, who researched it further with Barry Marshall from 1981. After unsuccessful attempts at culturing the bacteria from the stomach, they finally succeeded in visualizing colonies in 1982, when they unintentionally left their Petri dishes incubating for five days over the Easter weekend. In their original paper, Warren and Marshall contended that most stomach ulcers and gastritis were caused by bacterial infection and not by stress or spicy food, as had been assumed before.[155]
Some skepticism was expressed initially, but within a few years multiple research groups had verified the association of H. pylori with gastritis and, to a lesser extent, ulcers.[156] To demonstrate H. pylori caused gastritis and was not merely a bystander, Marshall drank a beaker of H. pylori culture. He became ill with nausea and vomiting several days later. An endoscopy 10 days after inoculation revealed signs of gastritis and the presence of H. pylori. These results suggested H. pylori was the causative agent. Marshall and Warren went on to demonstrate antibiotics are effective in the treatment of many cases of gastritis. In 1994, the National Institutes of Health stated most recurrent duodenal and gastric ulcers were caused by H. pylori, and recommended antibiotics be included in the treatment regimen.[157]
The bacterium was initially named Campylobacter pyloridis, then renamed C. pylori in 1987 (pylori being the genitive of pylorus, the circular opening leading from the stomach into the duodenum, from the Ancient Greek word πυλωρός, which means gatekeeper.[158]).[159] When 16S ribosomal RNA gene sequencing and other research showed in 1989 that the bacterium did not belong in the genus Campylobacter, it was placed in its own genus, Helicobacter from the ancient Greek έλιξ (hělix) "spiral" or "coil".[158][160]
In October 1987, a group of experts founded the European Helicobacter Study Group (EHSG), an international multidisciplinary research group and the only institution focused on H. pylori.[161] The Group is involved with the Annual International Workshop on Helicobacter and Related Bacteria,[162] the Maastricht Consensus Reports (European Consensus on the management of H. pylori),[163][164][165][166] and other educational and research projects, including two international long-term projects:
- European Registry on H. pylori Management (Hp-EuReg) – a database systematically registering the routine clinical practice of European gastroenterologists.[167]
- Optimal H. pylori management in primary care (OptiCare) – a long-term educational project aiming to disseminate the evidence based recommendations of the Maastricht IV Consensus to primary care physicians in Europe, funded by an educational grant from United European Gastroenterology.[168][169]
Research
Some investigators have suggested that H. pylori causes or prevents a wide range of other diseases, but many of these relationships remain controversial.[112][170][171][172] Some studies suggest that H. pylori plays an important role in the natural stomach ecology, e.g. by influencing the type of bacteria that colonize the gastrointestinal tract.[139][171] Other studies suggest that non-pathogenic strains of H. pylori may beneficially normalize stomach acid secretion,[173] and regulate appetite.[173]
Results from in vitro studies suggest that fatty acids, mainly polyunsaturated fatty acids, have a bactericidal effect against H. pylori, but their in vivo effects have not been proven.[174]
References
- ↑ "Helicobacter". Merriam-Webster Dictionary., "pylori". Merriam-Webster Dictionary..
- ↑ "pylori". Dictionary.com Unabridged. Random House.
- 1 2 3 4 5 6 7 8 9 10 11 12 Parikh, NS; Ahlawat, R (January 2022). "Helicobacter Pylori". StatPearls. PMID 30480966.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 "Helicobacter pylori - Chapter 4 - 2020 Yellow Book | Travelers' Health | CDC". wwwnc.cdc.gov. Archived from the original on 20 January 2022. Retrieved 23 February 2022.
- 1 2 3 4 5 6 7 8 "Management of Helicobacter pylori in 2023: who should be tested, treated, and how | This Changed My Practice". thischangedmypractice.com. Archived from the original on 20 October 2023. Retrieved 24 September 2023.
- 1 2 Hooi JK, Lai WY, Ng WK, Suen MM, Underwood FE, Tanyingoh D, et al. (August 2017). "Global Prevalence of Helicobacter pylori Infection: Systematic Review and Meta-Analysis". Gastroenterology. 153 (2): 420–429. doi:10.1053/j.gastro.2017.04.022. PMID 28456631.
- ↑ Minalyan A, Gabrielyan L, Scott D, Jacobs J, Pisegna JR (August 2017). "The Gastric and Intestinal Microbiome: Role of Proton Pump Inhibitors". Current Gastroenterology Reports. 19 (8): 42. doi:10.1007/s11894-017-0577-6. PMC 5621514. PMID 28733944.
- ↑ Rees, Alan M. (1997). Consumer Health USA. Greenwood Publishing Group. p. 194. ISBN 978-1-57356-068-9. Archived from the original on 2022-02-23. Retrieved 2022-02-23.
- ↑ Warren JR, Marshall B (June 1983). "Unidentified curved bacilli on gastric epithelium in active chronic gastritis". Lancet. 1 (8336): 1273–5. doi:10.1016/S0140-6736(83)92719-8. PMID 6134060. S2CID 1641856.
- ↑ Bytzer P, Dahlerup JF, Eriksen JR, Jarbøl DE, Rosenstock S, Wildt S (April 2011). "Diagnosis and treatment of Helicobacter pylori infection". Danish Medical Bulletin. 58 (4): C4271. PMID 21466771. Archived from the original on 5 January 2014.
- 1 2 Chang AH, Parsonnet J (October 2010). "Role of bacteria in oncogenesis". Clinical Microbiology Reviews. 23 (4): 837–57. doi:10.1128/CMR.00012-10. PMC 2952975. PMID 20930075.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 Kusters JG, van Vliet AH, Kuipers EJ (July 2006). "Pathogenesis of Helicobacter pylori infection". Clinical Microbiology Reviews. 19 (3): 449–90. doi:10.1128/CMR.00054-05. PMC 1539101. PMID 16847081.
- ↑ Butcher, Graham P. (2003). Gastroenterology: An illustrated colour text. Elsevier Health Sciences. p. 25. ISBN 978-0-443-06215-5. Archived from the original on 2021-06-25. Retrieved 2022-02-22.
- ↑ Butcher 2003, pp. 24–5
- ↑ Ryan, Kenneth (2010). Sherris Medical Microbiology. McGraw-Hill. pp. 573, 576. ISBN 978-0-07-160402-4.
- 1 2 Suerbaum S, Michetti P (October 2002). "Helicobacter pylori infection". The New England Journal of Medicine. 347 (15): 1175–86. CiteSeerX 10.1.1.572.9262. doi:10.1056/NEJMra020542. PMID 12374879.
- ↑ Wagner AD, Syn NL, Moehler M, Grothe W, Yong WP, Tai BC, et al. (August 2017). "Chemotherapy for advanced gastric cancer". The Cochrane Database of Systematic Reviews. 8: CD004064. doi:10.1002/14651858.cd004064.pub4. PMC 6483552. PMID 28850174.
- ↑ Wu Q, Yang ZP, Xu P, Gao LC, Fan DM (July 2013). "Association between Helicobacter pylori infection and the risk of colorectal neoplasia: a systematic review and meta-analysis". Colorectal Disease. 15 (7): e352-64. doi:10.1111/codi.12284. PMID 23672575. S2CID 5444584.
- ↑ "Helicobacter pylori" (PDF). cdc.gov. Center for Disease Control. Archived (PDF) from the original on 12 January 2019. Retrieved 7 October 2017.
- 1 2 Markowski AR, Markowska A, Guzinska-Ustymowicz K (October 2016). "Pathophysiological and clinical aspects of gastric hyperplastic polyps". World Journal of Gastroenterology. 22 (40): 8883–8891. doi:10.3748/wjg.v22.i40.8883. PMC 5083793. PMID 27833379.
- ↑ Soetikno RM, Kaltenbach T, Rouse RV, Park W, Maheshwari A, Sato T, et al. (March 2008). "Prevalence of nonpolypoid (flat and depressed) colorectal neoplasms in asymptomatic and symptomatic adults". JAMA. 299 (9): 1027–35. doi:10.1001/jama.299.9.1027. PMID 18319413.
- ↑ Nocturne G, Pontarini E, Bombardieri M, Mariette X (March 2019). "Lymphomas complicating primary Sjögren's syndrome: from autoimmunity to lymphoma". Rheumatology. Oxford, UK. 60 (8): 3513–3521. doi:10.1093/rheumatology/kez052. PMC 8328496. PMID 30838413.
- 1 2 3 Abbas H, Niazi M, Makker J (May 2017). "Mucosa-Associated Lymphoid Tissue (MALT) Lymphoma of the Colon: A Case Report and a Literature Review". The American Journal of Case Reports. 18: 491–497. doi:10.12659/AJCR.902843. PMC 5424574. PMID 28469125.
- 1 2 Paydas S (April 2015). "Helicobacter pylori eradication in gastric diffuse large B cell lymphoma". World Journal of Gastroenterology. 21 (13): 3773–6. doi:10.3748/wjg.v21.i13.3773. PMC 4385524. PMID 25852262.
- ↑ Schreuder MI, van den Brand M, Hebeda KM, Groenen PJ, van Krieken JH, Scheijen B (December 2017). "Novel developments in the pathogenesis and diagnosis of extranodal marginal zone lymphoma". Journal of Hematopathology. 10 (3–4): 91–107. doi:10.1007/s12308-017-0302-2. PMC 5712330. PMID 29225710.
- 1 2 Smedby KE, Ponzoni M (November 2017). "The aetiology of B-cell lymphoid malignancies with a focus on chronic inflammation and infections". Journal of Internal Medicine. 282 (5): 360–370. doi:10.1111/joim.12684. PMID 28875507. S2CID 42071521.
- 1 2 Kobayashi T, Takahashi N, Hagiwara Y, Tamaru J, Kayano H, Jin-nai I, et al. (January 2008). "Successful radiotherapy in a patient with primary rectal mucosa-associated lymphoid tissue lymphoma without the API2-MALT1 fusion gene: a case report and review of the literature". Leukemia Research. 32 (1): 173–5. doi:10.1016/j.leukres.2007.04.017. PMID 17570523.
- 1 2 Ma Q, Zhang C, Fang S, Zhong P, Zhu X, Lin L, Xiao H (March 2017). "Primary esophageal mucosa-associated lymphoid tissue lymphoma: A case report and review of literature". Medicine. 96 (13): e6478. doi:10.1097/MD.0000000000006478. PMC 5380272. PMID 28353588.
- 1 2 Guffey Johnson J, Terpak LA, Margo CE, Setoodeh R (April 2016). "Extranodal Marginal Zone B-cell Lymphoma of the Ocular Adnexa". Cancer Control. 23 (2): 140–9. doi:10.1177/107327481602300208. PMID 27218791.
- ↑ Saccà SC, Vagge A, Pulliero A, Izzotti A (December 2014). "Helicobacter pylori infection and eye diseases: a systematic review". Medicine. 93 (28): e216. doi:10.1097/md.0000000000000216. PMC 4603085. PMID 25526440.
- ↑ Mégraud F (1995). "Transmission of Helicobacter pylori: faecal-oral versus oral-oral route". Alimentary Pharmacology & Therapeutics. 9 Suppl 2 (Suppl 2): 85–91. PMID 8547533.
- ↑ Cave DR (May 1996). "Transmission and epidemiology of Helicobacter pylori". The American Journal of Medicine. 100 (5A): 12S–17S, discussion 17S-18S. doi:10.1016/s0002-9343(96)80224-5. PMID 8644777.
- 1 2 3 4 Brown LM (2000). "Helicobacter pylori: epidemiology and routes of transmission". Epidemiologic Reviews. 22 (2): 283–97. doi:10.1093/oxfordjournals.epirev.a018040. PMID 11218379.
- ↑ Delport W, van der Merwe SW (2007). "The transmission of Helicobacter pylori: the effects of analysis method and study population on inference". Best Practice & Research. Clinical Gastroenterology. 21 (2): 215–36. doi:10.1016/j.bpg.2006.10.001. hdl:2263/4083. PMID 17382274.
- ↑ Stark RM, Gerwig GJ, Pitman RS, Potts LF, Williams NA, Greenman J, et al. (February 1999). "Biofilm formation by Helicobacter pylori". Letters in Applied Microbiology. 28 (2): 121–6. doi:10.1046/j.1365-2672.1999.00481.x. PMID 10063642. S2CID 8912327.
- ↑ Chan WY, Hui PK, Leung KM, Chow J, Kwok F, Ng CS (October 1994). "Coccoid forms of Helicobacter pylori in the human stomach". American Journal of Clinical Pathology. 102 (4): 503–7. doi:10.1093/ajcp/102.4.503. PMID 7524304.
- ↑ Josenhans C, Eaton KA, Thevenot T, Suerbaum S (August 2000). "Switching of flagellar motility in Helicobacter pylori by reversible length variation of a short homopolymeric sequence repeat in fliP, a gene encoding a basal body protein". Infection and Immunity. 68 (8): 4598–603. doi:10.1128/IAI.68.8.4598-4603.2000. PMC 98385. PMID 10899861.
- ↑ Rust M, Schweinitzer T, Josenhans C (2008). "Helicobacter Flagella, Motility and Chemotaxis". In Yamaoka, Y. (ed.). Helicobacter pylori: Molecular Genetics and Cellular Biology. Caister Academic Press. ISBN 978-1-904455-31-8. Archived from the original on 2016-08-18. Retrieved 2022-02-22.
- ↑ Olson JW, Maier RJ (November 2002). "Molecular hydrogen as an energy source for Helicobacter pylori". Science. 298 (5599): 1788–90. Bibcode:2002Sci...298.1788O. doi:10.1126/science.1077123. PMID 12459589. S2CID 27205768.
- 1 2 Tomb JF, White O, Kerlavage AR, Clayton RA, Sutton GG, Fleischmann RD, et al. (August 1997). "The complete genome sequence of the gastric pathogen Helicobacter pylori". Nature. 388 (6642): 539–47. Bibcode:1997Natur.388..539T. doi:10.1038/41483. PMID 9252185. S2CID 4411220.
- ↑ "Genome information for the H. pylori 26695 and J99 strains". Institut Pasteur. 2002. Archived from the original on 26 November 2017. Retrieved 1 September 2008.
- ↑ "Helicobacter pylori 26695, complete genome". National Center for Biotechnology Information. Retrieved 1 September 2008.
- ↑ "Helicobacter pylori J99, complete genome". National Center for Biotechnology Information. Archived from the original on 26 August 2011. Retrieved 1 September 2008.
- ↑ Oh JD, Kling-Bäckhed H, Giannakis M, Xu J, Fulton RS, Fulton LA, et al. (June 2006). "The complete genome sequence of a chronic atrophic gastritis Helicobacter pylori strain: evolution during disease progression". Proceedings of the National Academy of Sciences of the United States of America. 103 (26): 9999–10004. Bibcode:2006PNAS..103.9999O. doi:10.1073/pnas.0603784103. PMC 1480403. PMID 16788065.
- ↑ van Vliet AH (January 2017). "Use of pan-genome analysis for the identification of lineage-specific genes of Helicobacter pylori". FEMS Microbiology Letters. 364 (2): fnw296. doi:10.1093/femsle/fnw296. PMID 28011701.
- ↑ Uchiyama I, Albritton J, Fukuyo M, Kojima KK, Yahara K, Kobayashi I (9 August 2016). "A Novel Approach to Helicobacter pylori Pan-Genome Analysis for Identification of Genomic Islands". PLOS ONE. 11 (8): e0159419. Bibcode:2016PLoSO..1159419U. doi:10.1371/journal.pone.0159419. PMC 4978471. PMID 27504980.
- 1 2 3 Sharma CM, Hoffmann S, Darfeuille F, Reignier J, Findeiss S, Sittka A, et al. (March 2010). "The primary transcriptome of the major human pathogen Helicobacter pylori". Nature. 464 (7286): 250–5. Bibcode:2010Natur.464..250S. doi:10.1038/nature08756. PMID 20164839. S2CID 205219639.
- 1 2 Baldwin DN, Shepherd B, Kraemer P, Hall MK, Sycuro LK, Pinto-Santini DM, Salama NR (February 2007). "Identification of Helicobacter pylori genes that contribute to stomach colonization". Infection and Immunity. 75 (2): 1005–16. doi:10.1128/IAI.01176-06. PMC 1828534. PMID 17101654.
- 1 2 Broutet N, Marais A, Lamouliatte H, de Mascarel A, Samoyeau R, Salamon R, Mégraud F (April 2001). "cagA Status and eradication treatment outcome of anti-Helicobacter pylori triple therapies in patients with nonulcer dyspepsia". Journal of Clinical Microbiology. 39 (4): 1319–22. doi:10.1128/JCM.39.4.1319-1322.2001. PMC 87932. PMID 11283049.
- ↑ Zawilak-Pawlik A, Zarzecka U, Żyła-Uklejewicz D, Lach J, Strapagiel D, Tegtmeyer N, et al. (August 2019). "Establishment of serine protease htrA mutants in Helicobacter pylori is associated with secA mutations". Scientific Reports. 9 (1): 11794. Bibcode:2019NatSR...911794Z. doi:10.1038/s41598-019-48030-6. PMC 6692382. PMID 31409845.
- ↑ Miehlke S, Yu J, Schuppler M, Frings C, Kirsch C, Negraszus N, et al. (April 2001). "Helicobacter pylori vacA, iceA, and cagA status and pattern of gastritis in patients with malignant and benign gastroduodenal disease". The American Journal of Gastroenterology. 96 (4): 1008–13. PMID 11316139. Archived from the original on 2022-02-23. Retrieved 2022-02-22.
- ↑ Capurro MI, Greenfield LK, Prashar A, Xia S, Abdullah M, Wong H, et al. (August 2019). "VacA generates a protective intracellular reservoir for Helicobacter pylori that is eliminated by activation of the lysosomal calcium channel TRPML1". Nature Microbiology. 4 (8): 1411–1423. doi:10.1038/s41564-019-0441-6. PMC 6938649. PMID 31110360.
- ↑ Müller, Stephan A.; Pernitzsch, Sandy R.; Haange, Sven-Bastiaan; Uetz, Peter; von Bergen, Martin; Sharma, Cynthia M.; Kalkhof, Stefan (2015-08-03). "Stable isotope labeling by amino acids in cell culture based proteomics reveals differences in protein abundances between spiral and coccoid forms of the gastric pathogen Helicobacter pylori". Journal of Proteomics. 126: 34–45. doi:10.1016/j.jprot.2015.05.011. ISSN 1874-3919. PMID 25979772. Archived from the original on 2021-07-27. Retrieved 2022-02-22.
- ↑ Wuchty, Stefan; Müller, Stefan A.; Caufield, J. Harry; Häuser, Roman; Aloy, Patrick; Kalkhof, Stefan; Uetz, Peter (May 2018). "Proteome Data Improves Protein Function Prediction in the Interactome of Helicobacter pylori". Molecular & Cellular Proteomics. 17 (5): 961–973. doi:10.1074/mcp.RA117.000474. PMC 5930399. PMID 29414760.
- ↑ Amieva MR, El-Omar EM (January 2008). "Host-bacterial interactions in Helicobacter pylori infection". Gastroenterology. 134 (1): 306–23. doi:10.1053/j.gastro.2007.11.009. PMID 18166359. S2CID 22061161.
- ↑ Schreiber S, Konradt M, Groll C, Scheid P, Hanauer G, Werling HO, et al. (April 2004). "The spatial orientation of Helicobacter pylori in the gastric mucus". Proceedings of the National Academy of Sciences of the United States of America. 101 (14): 5024–9. Bibcode:2004PNAS..101.5024S. doi:10.1073/pnas.0308386101. PMC 387367. PMID 15044704.
- ↑ Petersen AM, Krogfelt KA (May 2003). "Helicobacter pylori: an invading microorganism? A review". FEMS Immunology and Medical Microbiology (Review). 36 (3): 117–26. doi:10.1016/S0928-8244(03)00020-8. PMID 12738380.
- ↑ Ilver D, Arnqvist A, Ogren J, Frick IM, Kersulyte D, Incecik ET, et al. (January 1998). "Helicobacter pylori adhesin binding fucosylated histo-blood group antigens revealed by retagging". Science. 279 (5349): 373–7. Bibcode:1998Sci...279..373I. doi:10.1126/science.279.5349.373. PMID 9430586.
- ↑ Bugaytsova JA, Björnham O, Chernov YA, Gideonsson P, Henriksson S, Mendez M, et al. (March 2017). "Helicobacter pylori Adapts to Chronic Infection and Gastric Disease via pH-Responsive BabA-Mediated Adherence". Cell Host & Microbe. 21 (3): 376–389. doi:10.1016/j.chom.2017.02.013. PMC 5392239. PMID 28279347.
- ↑ Mahdavi J, Sondén B, Hurtig M, Olfat FO, Forsberg L, Roche N, et al. (July 2002). "Helicobacter pylori SabA adhesin in persistent infection and chronic inflammation". Science. 297 (5581): 573–8. Bibcode:2002Sci...297..573M. doi:10.1126/science.1069076. PMC 2570540. PMID 12142529.
- ↑ Mobley HL (1 January 2001). "Urease". In Mobley HL, Mendz GL, Hazell SL (eds.). Helicobacter pylori: Physiology and Genetics. Washington, DC: ASM Press. ISBN 978-1-55581-213-3. PMID 21290719. Archived from the original on 7 May 2021. Retrieved 22 February 2022.
- ↑ Debowski AW, Walton SM, Chua EG, Tay AC, Liao T, Lamichhane B, et al. (June 2017). "Helicobacter pylori gene silencing in vivo demonstrates urease is essential for chronic infection". PLOS Pathogens. 13 (6): e1006464. doi:10.1371/journal.ppat.1006464. PMC 5500380. PMID 28644872.
- 1 2 3 4 George G, Kombrabail M, Raninga N, Sau AK (March 2017). "Arginase of Helicobacter Gastric Pathogens Uses a Unique Set of Non-catalytic Residues for Catalysis". Biophysical Journal. 112 (6): 1120–1134. Bibcode:2017BpJ...112.1120G. doi:10.1016/j.bpj.2017.02.009. PMC 5376119. PMID 28355540.
- ↑ Smoot DT (December 1997). "How does Helicobacter pylori cause mucosal damage? Direct mechanisms". Gastroenterology. 113 (6 Suppl): S31-4, discussion S50. doi:10.1016/S0016-5085(97)80008-X. PMID 9394757.
- ↑ Hatakeyama M, Higashi H (December 2005). "Helicobacter pylori CagA: a new paradigm for bacterial carcinogenesis". Cancer Science. 96 (12): 835–43. doi:10.1111/j.1349-7006.2005.00130.x. PMID 16367902. S2CID 5721063.
- ↑ Dumrese C, Slomianka L, Ziegler U, Choi SS, Kalia A, Fulurija A, et al. (May 2009). "The secreted Helicobacter cysteine-rich protein A causes adherence of human monocytes and differentiation into a macrophage-like phenotype". FEBS Letters. 583 (10): 1637–43. doi:10.1016/j.febslet.2009.04.027. PMC 2764743. PMID 19393649.
- ↑ Sajib S, Zahra FT, Lionakis MS, German NA, Mikelis CM (February 2018). "Mechanisms of angiogenesis in microbe-regulated inflammatory and neoplastic conditions". Angiogenesis. 21 (1): 1–14. doi:10.1007/s10456-017-9583-4. PMID 29110215. S2CID 3346742.
- ↑ Shiotani A, Graham DY (November 2002). "Pathogenesis and therapy of gastric and duodenal ulcer disease". The Medical Clinics of North America. 86 (6): 1447–66, viii. CiteSeerX 10.1.1.550.8580. doi:10.1016/S0025-7125(02)00083-4. PMID 12510460.
- ↑ Dixon MF (February 2000). "Patterns of inflammation linked to ulcer disease". Bailliere's Best Practice & Research. Clinical Gastroenterology. 14 (1): 27–40. doi:10.1053/bega.1999.0057. PMID 10749087.
- 1 2 Blaser MJ, Atherton JC (February 2004). "Helicobacter pylori persistence: biology and disease". The Journal of Clinical Investigation. 113 (3): 321–33. doi:10.1172/JCI20925. PMC 324548. PMID 14755326.
- ↑ Schubert ML, Peura DA (June 2008). "Control of gastric acid secretion in health and disease". Gastroenterology. 134 (7): 1842–60. doi:10.1053/j.gastro.2008.05.021. PMID 18474247. S2CID 206210451.
- ↑ Peek RM, Crabtree JE (January 2006). "Helicobacter infection and gastric neoplasia". The Journal of Pathology. 208 (2): 233–48. doi:10.1002/path.1868. PMID 16362989. S2CID 31718278.
- ↑ Viala J, Chaput C, Boneca IG, Cardona A, Girardin SE, Moran AP, et al. (November 2004). "Nod1 responds to peptidoglycan delivered by the Helicobacter pylori cag pathogenicity island". Nature Immunology. 5 (11): 1166–74. doi:10.1038/ni1131. PMID 15489856. S2CID 2898805.
- ↑ Backert S, Selbach M (August 2008). "Role of type IV secretion in Helicobacter pylori pathogenesis". Cellular Microbiology. 10 (8): 1573–81. doi:10.1111/j.1462-5822.2008.01156.x. PMID 18410539. S2CID 37626.
- ↑ Hatakeyama M (September 2004). "Oncogenic mechanisms of the Helicobacter pylori CagA protein". Nature Reviews. Cancer. 4 (9): 688–94. doi:10.1038/nrc1433. PMID 15343275. S2CID 1218835.
- ↑ Tsuji S, Kawai N, Tsujii M, Kawano S, Hori M (July 2003). "Review article: inflammation-related promotion of gastrointestinal carcinogenesis--a perigenetic pathway". Alimentary Pharmacology & Therapeutics. 18 Suppl 1 (Suppl 1): 82–9. doi:10.1046/j.1365-2036.18.s1.22.x. PMID 12925144. S2CID 22646916.
- ↑ Suganuma M, Yamaguchi K, Ono Y, Matsumoto H, Hayashi T, Ogawa T, et al. (July 2008). "TNF-alpha-inducing protein, a carcinogenic factor secreted from H. pylori, enters gastric cancer cells". International Journal of Cancer. 123 (1): 117–22. doi:10.1002/ijc.23484. PMID 18412243. S2CID 5532769.
- ↑ Alfarouk KO, Bashir AH, Aljarbou AN, Ramadan AM, Muddathir AK, AlHoufie ST, et al. (22 February 2019). "Helicobacter pylori in Gastric Cancer and Its Management". Frontiers in Oncology. 9: 75. doi:10.3389/fonc.2019.00075. PMC 6395443. PMID 30854333.
- ↑ Kim W, Moss SF (December 2008). "The role of H. pylori in the development of stomach cancer". Oncology Review. 1 (Supp l1): 165–168. Archived from the original on 20 December 2014. Retrieved 25 August 2014.
- 1 2 Ferlay J, Colombet M, Soerjomataram I, Mathers C, Parkin DM, Piñeros M, et al. (April 2019). "Estimating the global cancer incidence and mortality in 2018: GLOBOCAN sources and methods". International Journal of Cancer. 144 (8): 1941–1953. doi:10.1002/ijc.31937. PMID 30350310.
- ↑ Kuipers EJ (March 1999). "Review article: exploring the link between Helicobacter pylori and gastric cancer". Alimentary Pharmacology & Therapeutics. 13 Suppl 1: 3–11. doi:10.1046/j.1365-2036.1999.00002.x. PMID 10209681. S2CID 19231673.
- ↑ Parkin DM (June 2006). "The global health burden of infection-associated cancers in the year 2002". International Journal of Cancer. 118 (12): 3030–44. doi:10.1002/ijc.21731. PMID 16404738. S2CID 10042384.
- ↑ Wroblewski LE, Peek RM, Wilson KT (October 2010). "Helicobacter pylori and gastric cancer: factors that modulate disease risk". Clinical Microbiology Reviews. 23 (4): 713–39. doi:10.1128/CMR.00011-10. PMC 2952980. PMID 20930071.
- ↑ Meurer LN, Bower DJ (April 2002). "Management of Helicobacter pylori infection". American Family Physician. 65 (7): 1327–36. PMID 11996414.
- ↑ Prabhu SR, Ranganathan S, Amarapurkar DN (November 1994). "Helicobacter pylori in normal gastric mucosa". The Journal of the Association of Physicians of India. 42 (11): 863–4. PMID 7868485.
- ↑ White JR, Winter JA, Robinson K (2015). "Differential inflammatory response to Helicobacter pylori infection: etiology and clinical outcomes". Journal of Inflammation Research. 8: 137–47. doi:10.2147/JIR.S64888. PMC 4540215. PMID 26316793.
- ↑ Deng JY, Liang H (April 2014). "Clinical significance of lymph node metastasis in gastric cancer". World Journal of Gastroenterology. 20 (14): 3967–75. doi:10.3748/wjg.v20.i14.3967. PMC 3983452. PMID 24744586.
- 1 2 Valenzuela MA, Canales J, Corvalán AH, Quest AF (December 2015). "Helicobacter pylori-induced inflammation and epigenetic changes during gastric carcinogenesis". World Journal of Gastroenterology. 21 (45): 12742–56. doi:10.3748/wjg.v21.i45.12742. PMC 4671030. PMID 26668499.
- ↑ Raza Y, Khan A, Farooqui A, Mubarak M, Facista A, Akhtar SS, et al. (October 2014). "Oxidative DNA damage as a potential early biomarker of Helicobacter pylori associated carcinogenesis". Pathology & Oncology Research. 20 (4): 839–46. doi:10.1007/s12253-014-9762-1. PMID 24664859. S2CID 18727504.
- ↑ Koeppel M, Garcia-Alcalde F, Glowinski F, Schlaermann P, Meyer TF (June 2015). "Helicobacter pylori Infection Causes Characteristic DNA Damage Patterns in Human Cells". Cell Reports. 11 (11): 1703–13. doi:10.1016/j.celrep.2015.05.030. PMID 26074077.
- 1 2 Muhammad JS, Eladl MA, Khoder G (February 2019). "Helicobacter pylori-induced DNA Methylation as an Epigenetic Modulator of Gastric Cancer: Recent Outcomes and Future Direction". Pathogens. 8 (1): 23. doi:10.3390/pathogens8010023. PMC 6471032. PMID 30781778.
- 1 2 Noto JM, Peek RM (2011). "The role of microRNAs in Helicobacter pylori pathogenesis and gastric carcinogenesis". Frontiers in Cellular and Infection Microbiology. 1: 21. doi:10.3389/fcimb.2011.00021. PMC 3417373. PMID 22919587.
- ↑ Santos JC, Ribeiro ML (August 2015). "Epigenetic regulation of DNA repair machinery in Helicobacter pylori-induced gastric carcinogenesis". World Journal of Gastroenterology. 21 (30): 9021–37. doi:10.3748/wjg.v21.i30.9021. PMC 4533035. PMID 26290630.
- 1 2 Raza Y, Ahmed A, Khan A, Chishti AA, Akhter SS, Mubarak M, et al. (May 2020). "Helicobacter pylori severely reduces expression of DNA repair proteins PMS2 and ERCC1 in gastritis and gastric cancer". DNA Repair. 89: 102836. doi:10.1016/j.dnarep.2020.102836. PMID 32143126.
- ↑ Dore MP, Pes GM, Bassotti G, Usai-Satta P (2016). "Dyspepsia: When and How to Test for Helicobacter pylori Infection". Gastroenterology Research and Practice. 2016: 8463614. doi:10.1155/2016/8463614. PMC 4864555. PMID 27239194.
- ↑ Olczak AA, Olson JW, Maier RJ (June 2002). "Oxidative-stress resistance mutants of Helicobacter pylori". Journal of Bacteriology. 184 (12): 3186–93. doi:10.1128/JB.184.12.3186-3193.2002. PMC 135082. PMID 12029034.
- ↑ O'Rourke EJ, Chevalier C, Pinto AV, Thiberge JM, Ielpi L, Labigne A, Radicella JP (March 2003). "Pathogen DNA as target for host-generated oxidative stress: role for repair of bacterial DNA damage in Helicobacter pylori colonization". Proceedings of the National Academy of Sciences of the United States of America. 100 (5): 2789–94. Bibcode:2003PNAS..100.2789O. doi:10.1073/pnas.0337641100. PMC 151419. PMID 12601164.
- ↑ Michod RE, Bernstein H, Nedelcu AM (May 2008). "Adaptive value of sex in microbial pathogens". Infection, Genetics and Evolution. 8 (3): 267–85. doi:10.1016/j.meegid.2008.01.002. PMID 18295550.
- 1 2 3 Dorer MS, Fero J, Salama NR (July 2010). Blanke SR (ed.). "DNA damage triggers genetic exchange in Helicobacter pylori". PLOS Pathogens. 6 (7): e1001026. doi:10.1371/journal.ppat.1001026. PMC 2912397. PMID 20686662.
- ↑ Loughlin MF, Barnard FM, Jenkins D, Sharples GJ, Jenks PJ (April 2003). "Helicobacter pylori mutants defective in RuvC Holliday junction resolvase display reduced macrophage survival and spontaneous clearance from the murine gastric mucosa". Infection and Immunity. 71 (4): 2022–31. doi:10.1128/IAI.71.4.2022-2031.2003. PMC 152077. PMID 12654822.
- 1 2 Wang G, Maier RJ (January 2008). "Critical role of RecN in recombinational DNA repair and survival of Helicobacter pylori". Infection and Immunity. 76 (1): 153–60. doi:10.1128/IAI.00791-07. PMC 2223656. PMID 17954726.
- 1 2 3 Stenström B, Mendis A, Marshall B (August 2008). "Helicobacter pylori--the latest in diagnosis and treatment". Australian Family Physician. 37 (8): 608–12. PMID 18704207.
- 1 2 Best LM, Takwoingi Y, Siddique S, Selladurai A, Gandhi A, Low B, et al. (March 2018). "Non-invasive diagnostic tests for Helicobacter pylori infection". The Cochrane Database of Systematic Reviews. 2018 (3): CD012080. doi:10.1002/14651858.CD012080.pub2. PMC 6513531. PMID 29543326.
- ↑ Logan RP, Walker MM (October 2001). "ABC of the upper gastrointestinal tract: Epidemiology and diagnosis of Helicobacter pylori infection". BMJ. 323 (7318): 920–2. doi:10.1136/bmj.323.7318.920. PMC 1121445. PMID 11668141.
- ↑ Selgrad M, Malfertheiner P (October 2008). "New strategies for Helicobacter pylori eradication". Current Opinion in Pharmacology. 8 (5): 593–7. doi:10.1016/j.coph.2008.04.010. PMID 18555746.
- ↑ Blanchard TG, Nedrud JG (2010). "9. Helicobacter pylori Vaccines". In Sutton P, Mitchell H (eds.). Helicobacter pylori in the 21st Century. CABI. pp. 167–189. ISBN 978-1-84593-594-8. Archived from the original on 11 May 2016. Retrieved 7 August 2013.
- ↑ Sutton P, Boag JM (November 2019). "Status of vaccine research and development for Helicobacter pylori". Vaccine. 37 (50): 7295–7299. doi:10.1016/j.vaccine.2018.01.001. PMC 6892279. PMID 29627231.
- ↑ de Vries R, Klok RM, Brouwers JR, Postma MJ (February 2009). "Cost-effectiveness of a potential future Helicobacter pylori vaccine in the Netherlands: the impact of varying the discount rate for health". Vaccine. 27 (6): 846–52. doi:10.1016/j.vaccine.2008.11.081. PMID 19084566. Archived from the original on 2021-05-10. Retrieved 2022-02-22.
- ↑ Rupnow MF, Chang AH, Shachter RD, Owens DK, Parsonnet J (October 2009). "Cost-effectiveness of a potential prophylactic Helicobacter pylori vaccine in the United States". The Journal of Infectious Diseases. 200 (8): 1311–7. doi:10.1086/605845. PMID 19751153.
- 1 2 Tsukamoto T, Nakagawa M, Kiriyama Y, Toyoda T, Cao X (August 2017). "Prevention of Gastric Cancer: Eradication of Helicobacter Pylori and Beyond". International Journal of Molecular Sciences. 18 (8): 1699. doi:10.3390/ijms18081699. PMC 5578089. PMID 28771198.
- 1 2 Burkitt MD, Duckworth CA, Williams JM, Pritchard DM (February 2017). "Helicobacter pylori-induced gastric pathology: insights from in vivo and ex vivo models". Disease Models & Mechanisms. 10 (2): 89–104. doi:10.1242/dmm.027649. PMC 5312008. PMID 28151409.
- 1 2 3 4 Laird-Fick HS, Saini S, Hillard JR (August 2016). "Gastric adenocarcinoma: the role of Helicobacter pylori in pathogenesis and prevention efforts". Postgraduate Medical Journal. 92 (1090): 471–7. doi:10.1136/postgradmedj-2016-133997. PMID 27222587. S2CID 20739020.
- 1 2 Lee YC, Chiang TH, Chou CK, Tu YK, Liao WC, Wu MS, Graham DY (May 2016). "Association Between Helicobacter pylori Eradication and Gastric Cancer Incidence: A Systematic Review and Meta-analysis". Gastroenterology. 150 (5): 1113–1124.e5. doi:10.1053/j.gastro.2016.01.028. PMID 26836587.
- ↑ Li L, Yu C (2019). "Helicobacter pylori Infection following Endoscopic Resection of Early Gastric Cancer". BioMed Research International. 2019: 9824964. doi:10.1155/2019/9824964. PMC 6816031. PMID 31737682.
- ↑ Azer, S. A.; Akhondi, H. (2019). "Gastritis". StatPearls. PMID 31334970.
- ↑ Malfertheiner P, Megraud F, O'Morain CA, Atherton J, Axon AT, Bazzoli F, et al. (European Helicobacter Study Group) (May 2012). "Management of Helicobacter pylori infection--the Maastricht IV/ Florence Consensus Report". Gut. 61 (5): 646–64. doi:10.1136/gutjnl-2012-302084. PMID 22491499. S2CID 1401974. Archived from the original on 2021-07-04. Retrieved 2022-02-22.
- ↑ Malfertheiner P, Megraud F, O'Morain CA, Gisbert JP, Kuipers EJ, Axon AT, et al. (European Helicobacter and microbiota study group and consensus panel) (January 2017). "Management of Helicobacter pylori infection-the Maastricht V/Florence Consensus Report". Gut. 66 (1): 6–30. doi:10.1136/gutjnl-2016-312288. PMID 27707777. S2CID 52868868.
- ↑ Fischbach L, Evans EL (August 2007). "Meta-analysis: the effect of antibiotic resistance status on the efficacy of triple and quadruple first-line therapies for Helicobacter pylori". Alimentary Pharmacology & Therapeutics (Meta-analysis). 26 (3): 343–57. doi:10.1111/j.1365-2036.2007.03386.x. PMID 17635369. S2CID 20973127.
- ↑ Graham DY, Shiotani A (June 2008). "New concepts of resistance in the treatment of Helicobacter pylori infections". Nature Clinical Practice. Gastroenterology & Hepatology. 5 (6): 321–31. doi:10.1038/ncpgasthep1138. PMC 2841357. PMID 18446147.
- ↑ William, Chey; Leontiadis, Grigorios (February 2017). "ACG Clinical Guideline: Treatment of Helicobacter pylori Infection". The American Journal of Gastroenterology. 112 (2): 212–239. doi:10.1038/ajg.2016.563. PMID 28071659. S2CID 9390953. Archived from the original on 2021-02-12. Retrieved 2022-02-22.
- ↑ Perna F, Zullo A, Ricci C, Hassan C, Morini S, Vaira D (November 2007). "Levofloxacin-based triple therapy for Helicobacter pylori re-treatment: role of bacterial resistance". Digestive and Liver Disease. 39 (11): 1001–5. doi:10.1016/j.dld.2007.06.016. PMID 17889627.
- ↑ Hsu PI, Wu DC, Chen A, Peng NJ, Tseng HH, Tsay FW, et al. (June 2008). "Quadruple rescue therapy for Helicobacter pylori infection after two treatment failures". European Journal of Clinical Investigation. 38 (6): 404–9. doi:10.1111/j.1365-2362.2008.01951.x. PMID 18435764. S2CID 205290582.
- ↑ Ren Q, Yan X, Zhou Y, Li WX (February 2016). "Periodontal therapy as adjunctive treatment for gastric Helicobacter pylori infection". The Cochrane Database of Systematic Reviews. 2016 (2): CD009477. doi:10.1002/14651858.CD009477.pub2. PMC 8255095. PMID 26852297.
- ↑ Violeta Filip P, Cuciureanu D, Sorina Diaconu L, Maria Vladareanu A, Silvia Pop C (2018). "MALT lymphoma: epidemiology, clinical diagnosis and treatment". Journal of Medicine and Life. 11 (3): 187–193. doi:10.25122/jml-2018-0035. PMC 6197515. PMID 30364585.
- ↑ Bron D, Meuleman N (September 2019). "Marginal zone lymphomas: second most common lymphomas in older patients". Current Opinion in Oncology. 31 (5): 386–393. doi:10.1097/CCO.0000000000000554. PMID 31246587. S2CID 195765608.
- ↑ Sassone M, Ponzoni M, Ferreri AJ (2017). "Ocular adnexal marginal zone lymphoma: Clinical presentation, pathogenesis, diagnosis, prognosis, and treatment". Best Practice & Research. Clinical Haematology. 30 (1–2): 118–130. doi:10.1016/j.beha.2016.11.002. PMID 28288706.
- ↑ Casulo C, Friedberg J (2017). "Transformation of marginal zone lymphoma (and association with other lymphomas)". Best Practice & Research. Clinical Haematology. 30 (1–2): 131–138. doi:10.1016/j.beha.2016.08.029. PMID 28288708.
- 1 2 3 Kuo SH, Yeh KH, Chen LT, Lin CW, Hsu PN, Hsu C, et al. (June 2014). "Helicobacter pylori-related diffuse large B-cell lymphoma of the stomach: a distinct entity with lower aggressiveness and higher chemosensitivity". Blood Cancer Journal. 4 (6): e220. doi:10.1038/bcj.2014.40. PMC 4080211. PMID 24949857.
- 1 2 3 Cheng Y, Xiao Y, Zhou R, Liao Y, Zhou J, Ma X (August 2019). "Prognostic significance of helicobacter pylori-infection in gastric diffuse large B-cell lymphoma". BMC Cancer. 19 (1): 842. doi:10.1186/s12885-019-6067-5. PMC 6712724. PMID 31455250.
- ↑ Tsai HJ, Tai JJ, Chen LT, Wu MS, Yeh KH, Lin CW, et al. (July 2020). "A multicenter prospective study of first-line antibiotic therapy for early-stage gastric mucosa-associated lymphoid tissue lymphoma and diffuse large B-cell lymphoma with histological evidence of mucosa-associated lymphoid tissue". Haematologica. 105 (7): e349–e354. doi:10.3324/haematol.2019.228775. PMC 7327622. PMID 31727764.
- ↑ Badgwell B, Das P, Ajani J (August 2017). "Treatment of localized gastric and gastroesophageal adenocarcinoma: the role of accurate staging and preoperative therapy". Journal of Hematology & Oncology. 10 (1): 149. doi:10.1186/s13045-017-0517-9. PMC 5558742. PMID 28810883.
- ↑ Goodman KJ, O'rourke K, Day RS, Wang C, Nurgalieva Z, Phillips CV, et al. (December 2005). "Dynamics of Helicobacter pylori infection in a US-Mexico cohort during the first two years of life". International Journal of Epidemiology. 34 (6): 1348–55. doi:10.1093/ije/dyi152. PMID 16076858.
- ↑ Goodman KJ, Cockburn M (March 2001). "The role of epidemiology in understanding the health effects of Helicobacter pylori". Epidemiology. 12 (2): 266–71. doi:10.1097/00001648-200103000-00023. PMID 11246592. S2CID 33212751.
- ↑ Li, R; Zhang, P; Hu, Z; Yi, Y; Chen, L; Zhang, H (14 May 2021). "Helicobacter pylori reinfection and its risk factors after initial eradication: A protocol for systematic review and meta-analysis". Medicine. 100 (19): e25949. doi:10.1097/MD.0000000000025949. PMC 8133036. PMID 34106668.
- ↑ Testerman TL, Morris J (September 2014). "Beyond the stomach: an updated view of Helicobacter pylori pathogenesis, diagnosis, and treatment". World Journal of Gastroenterology (Review). 20 (36): 12781–808. doi:10.3748/wjg.v20.i36.12781. PMC 4177463. PMID 25278678.
- 1 2 3 Blaser MJ (February 2005). "An endangered species in the stomach". Scientific American. 292 (2): 38–45. Bibcode:2005SciAm.292b..38B. doi:10.1038/scientificamerican0205-38. PMID 15715390.
- ↑ Graham DY, Yamaoka Y, Malaty HM (November 2007). "Contemplating the future without Helicobacter pylori and the dire consequences hypothesis". Helicobacter. 12 Suppl 2 (Suppl 2): 64–8. doi:10.1111/j.1523-5378.2007.00566.x. PMC 3128250. PMID 17991179.
- ↑ Delaney B, McColl K (August 2005). "Review article: Helicobacter pylori and gastro-oesophageal reflux disease". Alimentary Pharmacology & Therapeutics (Review). 22 Suppl 1 (Suppl 1): 32–40. doi:10.1111/j.1365-2036.2005.02607.x. PMID 16042657. S2CID 34921548.
- 1 2 3 Blaser MJ (October 2006). "Who are we? Indigenous microbes and the ecology of human diseases". EMBO Reports. 7 (10): 956–60. doi:10.1038/sj.embor.7400812. PMC 1618379. PMID 17016449.
- ↑ Blaser MJ, Chen Y, Reibman J (May 2008). "Does Helicobacter pylori protect against asthma and allergy?". Gut. 57 (5): 561–7. doi:10.1136/gut.2007.133462. PMC 3888205. PMID 18194986.
- ↑ Chen Y, Blaser MJ (August 2008). "Helicobacter pylori colonization is inversely associated with childhood asthma". The Journal of Infectious Diseases. 198 (4): 553–60. doi:10.1086/590158. PMC 3902975. PMID 18598192.
- 1 2 3 Pounder RE, Ng D (1995). "The prevalence of Helicobacter pylori infection in different countries". Alimentary Pharmacology & Therapeutics. 9 Suppl 2 (Suppl 2): 33–9. PMID 8547526.
- ↑ Smoak BL, Kelley PW, Taylor DN (March 1994). "Seroprevalence of Helicobacter pylori infections in a cohort of US Army recruits". American Journal of Epidemiology. 139 (5): 513–9. doi:10.1093/oxfordjournals.aje.a117034. PMID 8154475.
- ↑ Everhart JE, Kruszon-Moran D, Perez-Perez GI, Tralka TS, McQuillan G (April 2000). "Seroprevalence and ethnic differences in Helicobacter pylori infection among adults in the United States". The Journal of Infectious Diseases. 181 (4): 1359–63. doi:10.1086/315384. PMID 10762567.
- ↑ Malaty HM (2007). "Epidemiology of Helicobacter pylori infection". Best Practice & Research. Clinical Gastroenterology. 21 (2): 205–14. doi:10.1016/j.bpg.2006.10.005. PMID 17382273.
- ↑ Mégraud F (September 2004). "H pylori antibiotic resistance: prevalence, importance, and advances in testing". Gut. 53 (9): 1374–84. doi:10.1136/gut.2003.022111. PMC 1774187. PMID 15306603.
- ↑ Correa P, Piazuelo MB (January 2012). "Evolutionary History of the Helicobacter pylori Genome: Implications for Gastric Carcinogenesis". Gut and Liver. 6 (1): 21–8. doi:10.5009/gnl.2012.6.1.21. PMC 3286735. PMID 22375167.
- ↑ Linz B, Balloux F, Moodley Y, Manica A, Liu H, Roumagnac P, et al. (February 2007). "An African origin for the intimate association between humans and Helicobacter pylori". Nature. 445 (7130): 915–918. Bibcode:2007Natur.445..915L. doi:10.1038/nature05562. PMC 1847463. PMID 17287725.
- ↑ "The Nobel Prize in Physiology or Medicine 2005". Archived from the original on 23 May 2020. Retrieved 30 August 2018.
- ↑ Bizzozero G (1893). "Ueber die schlauchförmigen Drüsen des Magendarmkanals und die Beziehungen ihres Epitheles zu dem Oberflächenepithel der Schleimhaut". Archiv für Mikroskopische Anatomie. 42: 82–152. doi:10.1007/BF02975307. S2CID 85338121. Archived from the original on 2020-12-02. Retrieved 2022-02-22.
- ↑ Konturek JW (December 2003). "Discovery by Jaworski of Helicobacter pylori and its pathogenetic role in peptic ulcer, gastritis and gastric cancer" (PDF). Journal of Physiology and Pharmacology. 54 Suppl 3 (Suppl 3): 23–41. PMID 15075463. Archived from the original (PDF) on 30 September 2004. Retrieved 25 August 2008.
- ↑ Egan BJ, O'Morain CA (2007). "A historical perspective of Helicobacter gastroduodenitis and its complications". Best Practice & Research. Clinical Gastroenterology. 21 (2): 335–46. doi:10.1016/j.bpg.2006.12.002. PMID 17382281.
- ↑ Palmer ED (August 1954). "Investigation of the gastric mucosa spirochetes of the human". Gastroenterology. 27 (2): 218–20. doi:10.1016/S0016-5085(19)36173-6. PMID 13183283.
- ↑ Steer HW (August 1975). "Ultrastructure of cell migration throught [sic] the gastric epithelium and its relationship to bacteria". Journal of Clinical Pathology. 28 (8): 639–46. doi:10.1136/jcp.28.8.639. PMC 475793. PMID 1184762.
- ↑ Marshall BJ, Warren JR (June 1984). "Unidentified curved bacilli in the stomach of patients with gastritis and peptic ulceration". Lancet. 1 (8390): 1311–5. doi:10.1016/S0140-6736(84)91816-6. PMID 6145023. S2CID 10066001.
- ↑ Atwood, K.C. IV (2004). "Bacteria, Ulcers, and Ostracism? H. pylori and the making of a myth". Archived from the original on 5 November 2009. Retrieved 2 August 2008.
- ↑ Helicobacter pylori in peptic ulcer disease (Report). NIH Consensus Statement Online. Vol. 12. 7–9 January 1994. pp. 1–23. Archived from the original on 26 August 2011. Retrieved 21 December 2004.
- 1 2 Liddell HG, Scott R (1966). A Lexicon: Abridged from Liddell and Scott's Greek-English Lexicon. Oxford, UK: Oxford University Press. ISBN 978-0-19-910207-5.
- ↑ Marshall BS, Goodwin CS (1987). "Revised nomenclature of Campylobacter pyloridis". International Journal of Systematic Bacteriology. 37 (1): 68. doi:10.1099/00207713-37-1-68.
- ↑ Goodwin CS, Armstrong JA, Chilvers T, Peters M, Collins MD, Sly L, et al. (1989). "Transfer of Campylobacter pylori and Campylobacter mustelae to Helicobacter gen. nov. as Helicobacter pylori comb. nov. and Helicobacter mustelae comb. nov. respectively". International Journal of Systematic Bacteriology. 39 (4): 397–405. doi:10.1099/00207713-39-4-397.
- ↑ Buckley MJ, O'Morain CA (1998). "Helicobacter biology--discovery". British Medical Bulletin. 54 (1): 7–16. doi:10.1093/oxfordjournals.bmb.a011681. PMID 9604426.
- ↑ Mégraud F, et al. (European Helicobacter Study Group) (November 2007). "Evolution of Helicobacter pylori research as observed through the workshops of the European Helicobacter Study Group". Helicobacter. 12 Suppl 2 (Suppl 2): 1–5. doi:10.1111/j.1523-5378.2007.00581.x. PMID 17991169. S2CID 45841196.
- ↑ Malfertheiner P, Megraud F, O'Morain CA, Atherton J, Axon AT, Bazzoli F, et al. (European Helicobacter Study Group) (May 2012). "Management of Helicobacter pylori infection--the Maastricht IV/ Florence Consensus Report". Gut. 61 (5): 646–64. doi:10.1136/gutjnl-2012-302084. PMID 22491499. S2CID 1401974.
- ↑ Malfertheiner P, Megraud F, O'Morain C, Bazzoli F, El-Omar E, Graham D, et al. (June 2007). "Current concepts in the management of Helicobacter pylori infection: the Maastricht III Consensus Report". Gut. 56 (6): 772–81. doi:10.1136/gut.2006.101634. PMC 1954853. PMID 17170018.
- ↑ Malfertheiner P, Mégraud F, O'Morain C, Hungin AP, Jones R, Axon A, et al. (European Helicobacter Pylori Study Group (EHPSG)) (February 2002). "Current concepts in the management of Helicobacter pylori infection--the Maastricht 2-2000 Consensus Report". Alimentary Pharmacology & Therapeutics. 16 (2): 167–80. doi:10.1046/j.1365-2036.2002.01169.x. PMID 11860399. S2CID 6166458.
- ↑ Malfertheiner P, Mégraud F, O'Morain C, Bell D, Bianchi Porro G, Deltenre M, et al. (European Helicobacter Pylori Study Group (EHPSG)) (January 1997). "Current European concepts in the management of Helicobacter pylori infection--the Maastricht Consensus Report. The European Helicobacter Pylori Study Group (EHPSG)". European Journal of Gastroenterology & Hepatology. 9 (1): 1–2. doi:10.1097/00042737-199701000-00002. PMID 9031888. S2CID 36930542. Archived from the original on 2021-03-04. Retrieved 2022-02-22.
- ↑ McNicholl AG, Gasbarrini A, Tepes B, et al. (September 2014). "Pan-European registry on H. pylori management (Hp-EuReg): Interim analysis of 5,792 patients". Helicobacter. 2014: 69.
- ↑ "Management of Helicobacter pylori infection". Online courses. United European Gastroenterology. Archived from the original on 2 April 2015.
- ↑ "Annual Report 2012". United European Gastroenterology. Archived from the original on 4 June 2016. Retrieved 25 February 2015.
- ↑ Salama NR, Hartung ML, Müller A (June 2013). "Life in the human stomach: persistence strategies of the bacterial pathogen Helicobacter pylori". Nature Reviews. Microbiology. 11 (6): 385–99. doi:10.1038/nrmicro3016. PMC 3733401. PMID 23652324.
- 1 2 Gravina AG, Zagari RM, De Musis C, Romano L, Loguercio C, Romano M (August 2018). "Helicobacter pylori and extragastric diseases: A review". World Journal of Gastroenterology (Review). 24 (29): 3204–3221. doi:10.3748/wjg.v24.i29.3204. PMC 6079286. PMID 30090002.
- ↑ Bravo D, Hoare A, Soto C, Valenzuela MA, Quest AF (July 2018). "Helicobacter pylori in human health and disease: Mechanisms for local gastric and systemic effects". World Journal of Gastroenterology. 24 (28): 3071–3089. doi:10.3748/wjg.v24.i28.3071. PMC 6064966. PMID 30065554.
- 1 2 Ackerman J (June 2012). "The ultimate social network". Scientific American. Vol. 306, no. 6. pp. 36–43. doi:10.1038/scientificamerican0612-36. PMID 22649992.
- ↑ Jung SW, Lee SW (January 2016). "The antibacterial effect of fatty acids on Helicobacter pylori infection". The Korean Journal of Internal Medicine (Review). 31 (1): 30–5. doi:10.3904/kjim.2016.31.1.30. PMC 4712431. PMID 26767854.
External links
| Wikispecies has information related to Helicobacter pylori |
- "Information on tests for H. pylori". National Institutes of Health. U.S. Department of Health and Human Services. Archived from the original on 2013-06-13.
- "European Helicobacter Study Group (EHSG)". Archived from the original on 2010-03-15. Retrieved 2022-03-14.
- "Type strain of Helicobacter pylori at BacDive". Bacterial Diversity Metadatabase. Archived from the original on 2021-06-25. Retrieved 2022-02-22.
- "Helicobacter pylori". Genome. KEGG. Japan. 26695. Archived from the original on 2021-06-25. Retrieved 2022-02-22.
| Classification | |
|---|---|
| External resources |
|