Miliaria
| Miliaria | |
|---|---|
| Other names: Sweat rash, heat rash, prickly heat,[1] eccrine miliaria[2] | |
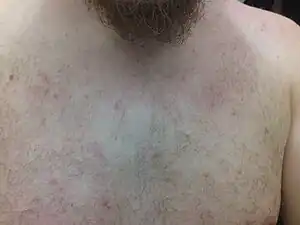 | |
| Typical red spots on chest, neck and shoulders, in miliaria rubra | |
| Pronunciation |
|
| Specialty | Dermatology |
| Symptoms | Small clear blisters or bumps, itchiness, redness[1] |
| Complications | Bacterial skin infection, increased sweating[1] |
| Types | Crystallina, rubra, profunda[1] |
| Risk factors | Hot and humid environment, exercise, fever, poorly breathable clothing[1] |
| Diagnostic method | Based on symptoms[1] |
| Differential diagnosis | Herpes simplex, bacterial folliculitis, acne[1] |
| Treatment | Cooler and dryer environment, loose fitting clothing[2] |
| Medication | Calamine lotion, corticosteroid or antibiotic creams[1][2] |
| Frequency | Common[1] |
Miliaria, also called heat rash, is a skin disease that presents as small clear blisters or bumps.[1] Itchiness and redness may also be present.[1] Complications may include subsequent bacterial skin infection, increased sweating, or poor ability to temperature regulate.[1]
Risk factors include a hot and humid environment, exercise, fever, and poorly breathable material against the skin.[1] The underlying mechanism involves sweat gland blockage.[1] There are three types crystallina, rubra, and profunda.[1] Diagnosis is based on symptoms.[1]
Treatment involves a cooler and dryer environment and loose fitting clothing.[2] Calamine lotion may also help.[1] Occasionally corticosteroid or antibiotic creams may be used.[2] The condition generally resolves after a few days of cooler temperatures.[1]
Miliaria is common.[1] Up to 10% of newborns are affected, often around the first few week of life.[1][2] Up to 30% of people who newly move to the tropics are also affected.[1] The term is named for the small seeds known as millet.[3]
Signs and symptoms
Symptoms of miliaria include small red rashes, called papules, which are irritated and itchy. These may simultaneously occur at a number of areas on a sufferer's body, the most common including the upper chest, neck, elbow creases, under the breasts and under the scrotum.[4] Other areas include skin folds, areas of the body that may rub against clothing, such as the back, chest, and stomach. A related and sometimes simultaneous condition is folliculitis, where hair follicles become plugged with foreign matter, resulting in inflammation.
The symptoms relating to miliaria should not be confused with shingles as they can be very similar. Shingles will restrict itself to one side of the body but also has a rash-like appearance. It is also accompanied by a prickling sensation and pain throughout the region. Those who suspect they have shingles and not miliaria should seek medical advice immediately as the sooner antivirals are taken, the better.
.jpg.webp) Miliaria
Miliaria.jpg.webp) Miliaria
Miliaria Miliaria rubra in a forehead
Miliaria rubra in a forehead
Miliaria can be classified according to the top level at which obstruction occurs in the sweat glands.
Miliaria crystalline
The most superficial obstruction (with the most mild presentation), is known as miliaria crystalline; instead of a rash, the patient presents with multiple tiny blister-like lesions that look like beads of perspiration and essentially cause no symptoms.[5]: 23 [6] Miliaria crystalline is also known as "Miliaria crystallina,"[7] and "Sudamina". The superficial vesicles are not associated with an inflammatory reaction.[5]: 23
Miliaria rubra
The most commonly encountered form of the illness is miliaria rubra, in which obstruction causes leakage of sweat into the deeper layers of the epidermis, provoking a local inflammatory reaction and giving rise to the typical appearance of redness (hence rubra) and larger (but still only a few millimetres), blister-like lesions. This form of the illness is often accompanied by the typical symptoms—intense itching or "pins and needles" with a lack of sweating (anhidrosis) to affected areas.[5]: 23 There is a small risk of heat exhaustion due to inability to sweat if the rash affects a large proportion of the body's surface area or the sufferer continues to engage in heat-producing activity. Miliaria rubra is also known as prickly heat and heat rash.[7] Differential diagnosis should be used to rule out polycythemia vera, which is a rare hematological disorder and appears more often in males than females, generally not before the age of 40. Both disorders share the common denominator of appearing after taking a hot shower.
Miliaria profunda
The most severe form of miliaria, miliaria profunda, sometimes referred to as "wildfire" due to the rapid spread and severe burning sensations, generally occurs as a complication of repeated episodes of miliaria rubra. The obstruction is deep in the structure of the sweat gland, causing the gland's secretions to leak between the superficial and deep layers of the skin. The rash, and associated symptoms, tend to appear within hours of an activity provoking sweating but similarly fade within hours when the stimulus for the sweating is removed. Miliaria profunda is characterised by non-pruritic, flesh-coloured, deep-seated, whitish papules.[5]: 24 The rash tends to be flesh-coloured as opposed to the prominent redness of miliaria rubra, and the risk of heat exhaustion is larger. Miliaria profunda is also less-commonly known as "mammillaria"[7]: chapter 40 [8]
Miliaria pustulosa
Miliaria pustulosa describes pustules due to inflammation and bacterial infection.[9] Miliaria pustulosa is preceded by another dermatitis that has produced injury, destruction, or blocking of the sweat duct.[5]: 23
Postmiliarial hypohidrosis
Postmiliarial hypohidrosis is a skin condition that results from occlusion of sweat ducts and pores, and may be severe enough to impair an individual's ability to perform sustained work in a hot environment.[5]: 24
Tropical anhidrotic asthenia
Tropical anhidrotic asthenia is a skin condition, a rare form of miliaria, with long-lasting poral occlusion, which produces anhidrosis and heat retention.[5]: 24 [7]
Occlusion miliaria
Occlusion miliaria is a skin condition that is accompanied by anhidrosis and increased heat-stress susceptibility, all after the application of extensive polyethylene film occlusion for 48 hours or longer.[5]: 24
Colloid milium
Colloid milium is a skin condition characterized by a translucent, flesh-colored, or slightly yellow 1- to 5-mm papule.[5]: 31
Pathophysiology
Miliaria occurs when the sweat gland ducts get clogged due to dead skin cells or bacteria such as Staphylococcus epidermidis,[10] a common bacterium that occurs on the skin which is also associated with acne.
The trapped sweat leads to irritation (prickling), itching and to a rash of very small blisters, usually in a localized area of the skin.
Prevention
Prickly heat can be prevented by avoiding activities that induce sweating, using air conditioning to cool the environment,[11] wearing light clothing and in general, avoiding hot and humid weather. Frequent cool showers or cool baths with mild soap can help to prevent heat rash.
Treatment
The primary remedy is to wear lighter clothing, or otherwise avoid overheating. The immediate treatment of the involved skin areas involves the use of a soothing ointment such as calamine lotion. Talcum powder may be used in some cases.
Medical assistance should be sought for the first episode of a rash with the appearance of miliaria. The differential diagnosis includes several conditions that an experienced practitioner should be able to recognise and may require treatment distinct from the usual measures taken for miliaria. In most cases, the rash of miliaria will resolve without intervention. However, severe cases can last for weeks and cause significant disability. General measures should be recommended for all patients, including moving to an air-conditioned environment if possible, avoiding sweat-provoking activities and occlusive clothing, and taking frequent cool showers.
It has been suggested that the use of topical antibacterials (including antibacterial soaps) may shorten the duration of symptoms in miliaria rubra even in the absence of obvious superinfection. Other topical agents that may reduce the severity of symptoms include anti-itch preparations such as calamine or menthol- or camphor-based preparations, and topical steroid creams. However, caution should be used with oil-based preparations (ointments and oily creams as opposed to water-based or aqueous lotions) that may increase blockage to the sweat glands and prolong the duration of illness. Other agents have been investigated including supplemental vitamin A and C and vitamin A based medications, but it is worth noting that there is little scientific evidence supporting any of the above treatments in reducing the duration of symptoms or frequency of complications.
In most tropical areas the local dispensaries sell prickly heat powder, a talc admixture containing drying milk proteins (Labilin) and Triclosan to fight the infection. These include cooling menthol to help alleviate difficulty getting to sleep. This is an effective treatment—the powder stays on the skin longer and treats bacteria dispersed into bed linens, providing a reasonably dry refuge area for healing. Miliaria often covers large areas, and generous use of Cortisone may be contraindicated for reasons stated on package warnings. Regular talcum powder will not reduce the rash but can alleviate burning and itching.
In cases where the rash has developed into open blisters or pustular lesions a doctor should be consulted since more aggressive, medically monitored treatment may be required.
See also
References
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 "Miliaria". DermNet NZ. Archived from the original on 27 April 2022. Retrieved 9 July 2022.
- 1 2 3 4 5 6 Guerra, KC; Toncar, A; Krishnamurthy, K (January 2022). "Miliaria". PMID 30725861.
{{cite journal}}: Cite journal requires|journal=(help) - ↑ Mosby's Medical Dictionary - E-Book. Elsevier Health Sciences. 29 April 2016. p. 1143. ISBN 978-0-323-41426-5. Archived from the original on 11 July 2022. Retrieved 9 July 2022.
- ↑ Jacklitsch, Brenda L. (June 29, 2011). "Summer Heat Can Be Deadly for Outdoor Workers". NIOSH: Workplace Safety and Health. Medscape and NIOSH. Archived from the original on December 4, 2012. Retrieved June 2, 2015.
- 1 2 3 4 5 6 7 8 9 James, William D.; Berger, Timothy G. (2006). Andrews' Diseases of the Skin: clinical Dermatology. Saunders Elsevier. ISBN 0-7216-2921-0.
- ↑ Haas N, Martens F, Henz BM (2004). "Miliaria crystallina in an intensive care setting". Clin. Exp. Dermatol. 29 (1): 32–34. doi:10.1111/j.1365-2230.2004.01444.x. PMID 14723716.
- 1 2 3 4 Rapini, Ronald P.; Bolognia, Jean L.; Jorizzo, Joseph L. (2007). Dermatology: 2-Volume Set. St. Louis: Mosby. p. 541. ISBN 1-4160-2999-0.
- ↑ G.O. Horne, F.R.C.P.E.† and R.H. Mole, M.A., B.M., M.R.C.P., Trans R Soc Trop Med Hyg (1951) 44 (4): 465-471. doi: 10.1016/S0035-9203(51)80023-3
- ↑ "Miliaria". Archived from the original on 2009-03-08. Retrieved 2009-05-14.
- ↑ Mowad CM, McGinley KJ, Foglia A, Leyden JJ (1995). "The role of extracellular polysaccharide substance produced by Staphylococcus epidermidis in miliaria". J. Am. Acad. Dermatol. 33 (5 Pt 1): 729–733. doi:10.1016/0190-9622(95)91809-4. PMID 7593770.
- ↑ Niparko, John Kim; Klag, Michael J.; Lawrence, Robert M.; Romaine-Davis, Ada (1999). Johns Hopkins family health book. London: HarperCollins. p. 1308. ISBN 0-06-270149-5.
External links
- Prickly Heat at Merck Manual of Diagnosis and Therapy Home Edition - with pictures
- WebMd Description Archived 2010-09-10 at the Wayback Machine
- Clinical pictures of heat rash/prickly heat - Skinsight Archived 2010-07-26 at the Wayback Machine
| Classification | |
|---|---|
| External resources |