Pharmacodynamics of spironolactone
The pharmacodynamics of spironolactone, an antimineralocorticoid and antiandrogen medication, concern its mechanisms of action, including its biological targets and activities, as well as its physiological effects. The pharmacodynamics of spironolactone are characterized by high antimineralocorticoid activity, moderate antiandrogenic activity, and weak steroidogenesis inhibition. In addition, spironolactone has sometimes been found to increase estradiol and cortisol levels and hence could have slight indirect estrogenic and glucocorticoid effects. The medication has also been found to interact very weakly with the estrogen and progesterone receptors, and to act as an agonist of the pregnane X receptor. Likely due to increased activation of the estrogen and/or progesterone receptors, spironolactone has very weak but significant antigonadotropic effects.[13][14]
| Site | Value (nM) | Type | Action | Species | Ref |
|---|---|---|---|---|---|
| ARTooltip Androgen receptor | 39.4 120 13–670 >20,000 | Ki IC50a IC50b EC50 | Antagonist | Human | [5] [6] [7][8] [8] |
| ERTooltip Estrogen receptorc | >1,100 5,700 | Ki IC50b | Antagonist | Human | [5] [7] |
| ERαTooltip Estrogen receptor alpha | 5,970–>20,000 >20,000 | IC50b EC50 | Agonist | Human | [9][8] [8] |
| ERβTooltip Estrogen receptor beta | 4940–>20,000 3,300 | IC50b EC50 | Inconsistent | Human | [9][8] [8] |
| GRTooltip Glucocorticoid receptor | 32.6 1,400 2,410–6,920 >20,000 | Ki IC50a IC50b EC50 | Antagonist | Human | [5] [6] [9][10] [8] |
| MRTooltip Mineralocorticoid receptor | 2.32 49 2.4–60 17.7 | Ki IC50a IC50b Kb | Antagonist | Human | [5] [6] [7][6] [5] |
| PRTooltip Progesterone receptorc | 400 650 >25,000 740–2,619 | Ki IC50a IC50b EC50 | Agonist | Human | [5] [6] [7][10] [9][7] |
| PR-BTooltip Progesterone receptor B | 4,000 >20,000 | IC50b EC50 | Antagonist | Human | [8] [8] |
| Notes: The ranges are the values reported in different studies. Footnotes: a = Binding inhibition. b = Functional antagonism. c = Subtype unspecified (probably ERα and PR-B, however). Sources: [11][12] | |||||
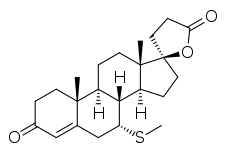
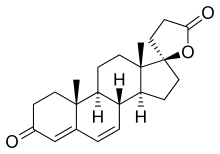
Spironolactone has a very short biological half-life and is considered to be a prodrug; hence, its active metabolites are responsible for most of its pharmacodynamics. The major active forms of spironolactone include 7α-thiomethylspironolactone (7α-TMS) and canrenone (7α-desthioacetyl-δ6-spironolactone), while more minor metabolites of spironolactone include 7α-thiospironolactone (7α-TS), 6β-hydroxy-7α-thiomethylspironolactone (6β-OH-7α-TMS), and a number of others.
Aside from its primary mechanisms of action of antimineralocorticoid and antiandrogenic action, spironolactone has been found in preclinical research to interact very weakly with the progesterone and estrogen receptors and to have very weak mixed progestogenic and antiprogestogenic activity as well as very weak mixed estrogenic and antiestrogenic activity.[15][14][16] The clinical significance of these actions, if any, is uncertain.[16] However, a small clinical study found that high doses of spironolactone had neither progestogenic nor antiprogestogenic effects in women.[16][17] In any case, if one or both of these actions are clinically relevant, they might contribute to the menstrual irregularities and breast side effects of spironolactone.[14][18] Spironolactone is also an agonist of the pregnane X receptor,[19] and is able to induce the expression of CYP3A4 and P-glycoprotein in the body via this action.[20][21][22] This effect may contribute to the drug interactions of spironolactone.[20][21][22]
Antimineralocorticoid activity
Spironolactone inhibits the effects of mineralocorticoids, namely, aldosterone, by displacing them from MR in the cortical collecting duct of kidney nephrons. This decreases the reabsorption of sodium and water while limiting the excretion of potassium (A K+ sparing diuretic). The medication has a slightly delayed onset of action, and so it takes several days for diuresis to occur. This is because the MR is a nuclear receptor which works through regulating gene transcription and gene expression, in this case, to decrease the production and expression of ENaC and ROMK electrolyte channels in the distal nephrons. In addition to direct antagonism of the MRs, the antimineralocorticoid effects of spironolactone may also in part be mediated by direct inactivation of 11β-hydroxylase and aldosterone synthase (18-hydroxylase), enzymes involved in the biosynthesis of mineralocorticoids. If levels of mineralocorticoids are decreased then there are lower circulating levels to compete with spironolactone to influence gene expression as mentioned above.[23] The onset of action of the antimineralocorticoid effects of spironolactone is relatively slow, with the peak effect sometimes occurring 48 hours or more after the first dose.[1][24]
Canrenone is an antagonist of the MR similarly to spironolactone,[25] but is slightly more potent in comparison.[24][26] It has been determined that 7α-TMS accounts for around 80% of the potassium-sparing effect of spironolactone[1][2][3] while canrenone accounts for the remaining approximate 10 to 25%.[4] In accordance, 7α-TMS occurs at higher circulating concentrations than does canrenone in addition to having a higher relative affinity for the MR.[2]
Antiandrogenic activity
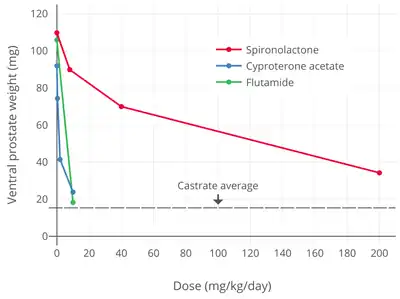
Spironolactone is an antagonist of the AR, the biological target of androgens like testosterone and DHT.[28][29] Its affinity for the AR has been found to vary widely between different studies, with a range of 2.7 to 67% of that of DHT.[30][31][27][32] One study found affinities for the AR of 3.0% for spironolactone, 4.2% for 7α-TMS, and 3.1% for 7α-TS.[31] Conversely, the affinity of canrenone for the AR was found to be 0.84% of that of DHT in another study, relative to 67% for spironolactone.[32] However, another study found the affinity of canrenone for the AR to be 2.5 to 14%, relative to 4.1 to 31% in the case of spironolactone.[33] Another study that directly compared the affinities of spironolactone and canrenone reported that spironolactone had 5-fold higher affinity for the AR than canrenone (5% and 1% of that of DHT, respectively).[28] A comparative study of binding inhibition to the AR in rat prostate cytosol AR found IC50 values of 3 nM for DHT, 24 nM for cyproterone acetate, and 67 nM for spironolactone.[34] Spironolactone antagonizes the effects of exogenous testosterone administered to castrated animals.[30] It works by binding to the AR and displacing androgens like testosterone and DHT from the receptor, thereby reducing its activation by these hormones.[28] A study found that oral spironolactone had "about 10 to 20% of the feminizing effect of cyproterone acetate" on sexual differentiation in male rat fetuses, with 40 mg/day spironolactone having an equal effect to 1 to 3 mg/day cyproterone acetate.[35][36]
The AR antagonism of spironolactone mostly underlies its antiandrogenic activity and is the major mechanism responsible for its therapeutic benefits in the treatment of androgen-dependent conditions like acne, hirsutism, and pattern hair loss and its usefulness in hormone therapy for transgender women.[28][16] In addition, the AR antagonism of spironolactone is involved in its feminizing side effects in men like gynecomastia.[28] Spironolactone has been found to produce gynecomastia without changes in testosterone or estradiol levels, implicating AR antagonism in this side effect.[30] Gynecomastia is a major known side effect of AR antagonists.[37]
Spironolactone, similarly to other steroidal antiandrogens such as cyproterone acetate, is actually not a pure, or silent, antagonist of the AR, but rather is a weak partial agonist with the capacity for both antagonistic and agonistic effects.[38][39][40][41] However, in the presence of sufficiently high levels of potent full agonists like testosterone and DHT (the cases in which spironolactone is usually used even with regards to the "lower" relative levels present in females),[41] spironolactone will behave more similarly to a pure antagonist. Nonetheless, there may still be a potential for spironolactone to produce androgenic effects in the body at sufficiently high dosages and/or in those with very low endogenous androgen concentrations. As an example, one condition in which spironolactone is contraindicated is prostate cancer in men being treated with androgen deprivation therapy,[42] as spironolactone has been shown in vitro to significantly accelerate carcinoma growth in the absence of any other androgens.[39] In accordance, three case reports have described significant worsening of prostate cancer with spironolactone treatment in patients with the disease, leading the authors to conclude that spironolactone has the potential for androgenic effects in some contexts and that it should perhaps be considered to be a selective androgen receptor modulator (SARM), albeit with mostly antagonistic effects.[43][44][45] However, in another case report, spironolactone was effective in normalizing prostate-specific antigen in a man with prostate cancer.[46] In addition, spironolactone has been studied limitedly in the treatment of prostate cancer.[47][48]
Canrenone binds to and blocks the AR in vitro.[29] However, relative to spironolactone, canrenone is described as having very weak affinity for the AR.[49] In accordance, replacement of spironolactone with canrenone in male patients has been found to reverse spironolactone-induced gynecomastia, suggesting that canrenone is comparatively much less potent in vivo as an antiandrogen.[29] As such, based on the above, the antiandrogenic effects of spironolactone are considered to be largely due to other metabolites rather than due to canrenone.[29][50][51] In accordance, 7α-TS and 7α-TMS have been found to possess approximately equivalent affinity for the rat prostate AR relative to that of spironolactone, thus likely accounting for the retention of the antiandrogenic activity of spironolactone.[31]
Spironolactone is described as having relatively weak antiandrogenic activity.[52][49][53][54] Nonetheless, it is useful as an antiandrogen in women, who have low androgen levels compared to men.[55][56] In addition, considerable incidences of gynecomastia, decreased libido, and erectile dysfunction have been reported in men taking very high doses of spironolactone (200 to 400 mg/day).[55]
| Compound | ARTooltip Androgen receptor RBATooltip Relative binding affinity (%) | ARTooltip Androgen receptor Ki (nM) |
|---|---|---|
| Metribolone | 100 | 1.18 |
| Dihydrotestosterone | 136 | 0.87 |
| Testosterone | 117 | 1.01 |
| Spironolactone | 67.0 | 1.76 |
| Trimethyltrienolone | 14.8 | 8.0 |
| Megestrol acetate | 13.6 | 8.7 |
| Cyproterone acetate | 12.5 | 9.5 |
| Progesterone | 6.6 | 18 |
| Estradiol | 4.9 | 24 |
| Androstenedione | 2.0 | 58 |
| Canrenone | 0.84 | 140 |
| Flutamide | 0.079 | 1200 |
| Cimetidine | 0.00084 | 140,000 |
| Notes: (1) Human skin fibroblasts used for assays. (2) Situation in vivo is different for flutamide and spironolactone due biotransformation. (3) Conflicting findings for spironolactone. Sources: Main: [35][32] Related: [57][58][59] | ||
Spironolactone has been found to have effectiveness in the treatment of hirsutism in women at a dosage of as low as 50 mg/day.[60] The effectiveness of spironolactone in the treatment of hirsutism in women has been found to be near-significantly greater at a dosage of 100 mg/day relative to a dosage of 200 mg/day (19% ± 8% and 30% ± 3% reduction in hair shaft diameter, respectively; p = 0.07).[61][62][35] Levels of free testosterone were unchanged, suggesting that the antiandrogenic efficacy of spironolactone was due exclusively to direct AR blockade.[61][62] In addition, other studies have found that 100 mg/day spironolactone is significantly or near-significantly inferior to 500 mg/day flutamide in improving symptoms of acne and hirsutism.[63][64][65] One study compared placebo and dosages of spironolactone of 50, 100, 150, and 200 mg/day in the treatment of acne in women and observed progressive increases in response rates up to the 200 mg/day dosage.[35][66] These findings suggest that the antiandrogenic effectiveness of spironolactone is not maximal below a dosage of 200 mg/day, and are in accordance with the typical dosage range of spironolactone of 50 to 200 mg/day in women.[63][52][67][66]
Studies have found that spironolactone is associated with a significantly lower risk of prostate cancer in men (HRTooltip hazard ratio = 0.69).[68][69] This was apparent for high-dose spironolactone, using doses of 75 mg/day and above (HR = 0.74).[68] Conversely, lower doses of spironolactone (<75 mg/day) were not associated with a decreased risk of prostate cancer (HR = 0.99).[68] Levels of prostate-specific antigen (PSA) were assessed and were found to be significantly lower in spironolactone-treated men.[68] The decreased incidence of prostate cancer with spironolactone was hypothesized to be due to its known antiandrogenic activity.[68]
Steroidogenesis inhibition
Spironolactone is sometimes able to significantly lower testosterone levels at high dosages in spite of not acting as an antigonadotropin, and this is thought to be due to direct enzymatic inhibition of 17α-hydroxylase and 17,20-lyase, enzymes necessary for the biosynthesis of testosterone.[30][70][71][72] Although spironolactone is said to be a relatively weak inhibitor of 17α-hydroxylase and 17,20-lyase,[73][30] at least compared to more potent steroidogenesis inhibitors like ketoconazole and abiraterone acetate (which can reduce testosterone concentrations to castrate levels), this action may contribute to a significant portion of the antiandrogenic activity of spironolactone, for instance lowering testosterone levels in women with hyperandrogenism and in transgender women.[74][75][76] Canrenone inhibits steroidogenic enzymes such as 17α-hydroxylase, 17,20-lyase, 11β-hydroxylase, cholesterol side-chain cleavage enzyme, and 21-hydroxylase similarly to spironolactone, but is more potent in doing so in comparison.[77] In spite of the findings of spironolactone and canrenone on these steroidogenic enzymes however, spironolactone has shown mixed and highly inconsistent effects on steroid hormone levels in clinical studies.[30][16] In some studies, it significantly lowers testosterone levels, whereas in other studies, testosterone and estradiol levels remain unchanged, even at high dosages.[30][78][79] It has been suggested that spironolactone may weakly and partially inhibit 17α-hydroxylase, which in turn results in upregulation of the HPG axis such that steroid hormone levels remain normal.[30] Conversely however, inhibition of 17α-hydroxylase in the ovary may disrupt the menstrual cycle and thereby result in menstrual irregularities.[30]
Animal studies have found that spironolactone inhibits testicular CYP450-mediated steroidogenesis by 5 to 75% across a dosage range of 1 to 100 mg/kg, with 50% inhibition occurring at a dose of 40 mg/kg.[30] A decrease in the production of testosterone and 17α-hydroxyprogesterone due to inhibition of steroidogenic enzymes like 17α-hydroxylase has been found to occur at dosages of 40 to 200 mg/kg.[30] For comparison, the clinical dosage range of spironolactone in humans is usually about 4 to 8 mg/kg.[30]
There is also mixed/conflicting evidence that spironolactone may inhibit 5α-reductase, and thus the synthesis of the potent androgen DHT from testosterone, to some extent.[28][80][81][82][83] However, the combination of spironolactone and the potent 5α-reductase inhibitor finasteride has been found to have significant improved effectiveness in the treatment of hirsutism relative to spironolactone therapy alone, suggesting that any inhibition of 5α-reductase by spironolactone is only weak or at best incomplete.[83] Spironolactone has been found not to have activity as an aromatase inhibitor.[84][85]
Estrogenic activity
Spironolactone has been found to directly interact with the ER.[15] A study using human uterine tissue found that a 1,000-fold excess of spironolactone (0.3–2 μM) resulted in no displacement of estradiol from the ER.[86] However, a subsequent study found that the medication did interact with the human ER at higher concentrations, albeit with very low affinity (Ki = 20 μM).[15] In the same study, spironolactone was administered to rats and found to produce mixed estrogenic and antiestrogenic or selective estrogen receptor modulator (SERM)-like effects that were described as very similar to those of tamoxifen.[15] In spite of the fact that tamoxifen had two orders of magnitude higher affinity for the ER than spironolactone however, the two medications showed similar potency in vivo.[15] The likelihood of spironolactone interacting with the ER itself is remote in consideration of its very low affinity for the receptor in vitro.[14] However, it has been hypothesized that metabolism of spironolactone might result in active metabolites with greater ER affinity, which might potentially account for the activity.[15][14] One of the major active metabolites of spironolactone, canrenone, likewise did not interact with the human uterine ER at up to a more than 5,000-fold excess (25 μM).[87] In other research, spironolactone has been found to have no estrogenic or antiestrogenic effects in the uterus when administered by subcutaneous injection in rodents even at very high doses.[88]
The authors of the study concluded that direct interaction of spironolactone (and/or its metabolites) with the ER could be involved in the gynecomastia, feminization, and effects on gonadotropin levels that the medication is associated with.[15] Subsequently, it has also been suggested that, as a SERM-like medication, ER agonistic activity of spironolactone in the pituitary gland could be responsible for its antigonadotropic effects while ER antagonistic activity of spironolactone in the endometrium could be responsible for the menstrual disturbances that are associated with it.[14] Such actions might explain these effects of spironolactone in light of the finding that it is not significantly progestogenic or antiprogestogenic in women even at high dosages.[16][17][14]
In accordance, a study found that in women treated with a GnRH analogue, spironolactone therapy almost completely prevented the bone loss that is associated with these medications, whereas treatment with the selective AR antagonist flutamide had no such effect.[89][53] Other studies have also found an inverse relationship between spironolactone and decreased bone mineral density and bone fractures in men.[90][91] Estrogens are well known for maintaining and having positive effects on bone, and it has been suggested that the estrogenic activity of spironolactone may be involved in its positive effects on bone mineral density.[89][53][92] High levels of aldosterone have been associated with adverse bone changes, and so the antimineralocorticoid activity of spironolactone might partially or fully be responsible for these effects as a potential alternative explanation.[91]
In addition to potential direct interaction with the ER, spironolactone also has some indirect estrogenic activity, which it mediates via several actions, including:
- By acting as an antiandrogen, as androgens can suppress both estrogen production and signaling (e.g., in the breasts).[29][93]
- Inhibition of the conversion of estradiol to estrone, resulting in an increase in the ratio of circulating estradiol to estrone.[84] Estradiol is far more potent than estrone as an estrogen, which is comparatively almost inactive.[94][95]
- Enhancement of the rate of peripheral conversion of testosterone into estradiol, thus decreasing the ratio of circulating testosterone to estradiol.[75]
Spironolactone has been found to act as a reversible inhibitor of human 17β-hydroxysteroid dehydrogenase 2 (17β-HSD2), albeit with weak potency (Ki = 0.25–2.4 μM; IC50 = 0.27–1.1 μM).[96][97][98][85] C7α thioalkyl derivatives of spironolactone like the 7α-thioethyl analogue were found to inhibit the enzyme with greater potency, suggesting that the actual active metabolites of spironolactone like 7α-TMS might be more potent inhibitors.[96][85] 17β-HSD2 is a key enzyme responsible for inactivation of estradiol into estrone in various tissues, and inhibition of 17β-HSD2 by spironolactone may be involved in the gynecomastia and altered ratio of circulating testosterone to estradiol associated with the medication.[84][99] Spironolactone has also been associated with positive effects on bone, and it is notable that 17β-HSD2 inhibitors are under investigation as potential novel treatments for osteoporosis due to their ability to prevent estradiol inactivation in this tissue.[100][101] In contrast to 17β-HSD2, spironolactone does not appear to inhibit 17β-hydroxysteroid dehydrogenase 1 (17β-HSD1) in vitro.[30]
In contrast to estrogens and SERMs,[95][102] spironolactone does not increase sex hormone-binding globulin (SHBG) levels[35][66][103] or risk of venous thromboembolism.[104] Nor is there an increase in the risk of breast cancer or endometrial cancer with spironolactone.[105][106][99][68][107][108][109]
Spironolactone is known to produce a high rate of menstrual irregularities in women at around the middle of the menstrual cycle, when ovulation occurs.[14][110] A study investigated the effects of 100 mg/day spironolactone on the endometrium and hormone levels and the mechanism for the menstrual abnormalities associated with it in a group of women with polycystic ovary syndrome.[14][110] They found that spironolactone, likely due to inhibition of steroidogenesis, blunted the surge in estradiol levels around ovulation, with estradiol levels of about 41 to 66% of normal at this time.[110][14] Conversely, periovulatory levels of the gonadotropins, luteinizing hormone and follicle-stimulating hormone, were unchanged.[110][14] Spironolactone significantly decreased endometrial thickness in the women (by 22 to 33%), and as estrogens stimulate endometrial growth, this effect of spironolactone may have been due to the decreased levels of estradiol.[110][14] As such, spironolactone may have a functional antiestrogenic effect around ovulation in women, and this may be involved in its side effect of menstrual irregularities at high doses.[110][14]
Progestogenic activity
Spironolactone has weak progestogenic activity in bioassays.[73][111] Its actions in this regard are a result of direct agonist activity at the PR, though with a very low half-maximal potency.[112] Spironolactone's progestogenic activity has been suggested to be involved in some of its side effects,[18] including the menstrual irregularities seen in women and the undesirable serum lipid profile changes that are seen at higher doses.[113][114][115] It has also been suggested to augment the gynecomastia caused by the estrogenic effects of spironolactone,[116] as progesterone is known to be involved in mammary gland development.[117] A major active metabolite of spironolactone, canrenone, has been found to interact with the human uterine PR with a Ki of 300 nM.[87] This is relatively weak at approximately 100-fold less than that of progesterone.[87] In any case, levels of canrenone of up to 1,200 nM have been observed in some studies with 100 to 200 mg doses of spironolactone.[87]
It has been widely stated that the menstrual irregularities associated with spironolactone are due to its progestogenic activity, and animal studies, both in rabbits and rhesus monkeys, have shown clear progestogenic effects of spironolactone.[118] However, the dosages of spironolactone used in animals to produce progestogenic effects were very high (50–200 mg/kg/day in rabbits, 400 mg/day in rhesus monkeys).[118] In one study, the threshold dose by subcutaneous injection for endometrial transformation in rabbits was 0.003–0.01 mg for cyproterone acetate, 0.1–0.3 mg for drospirenone, 0.5 mg for progesterone, and 10–20 mg for spironolactone.[119] Spironolactone orally at 40 mg/kg/day failed to show an antigonadotropic effect or decrease testosterone levels in male cynomolgus monkeys, whereas oral drospirenone at 4 mg/day was effective and strongly suppressed testosterone levels.[119] In addition, no evidence of progestogenic nor antiprogestogenic effects (as assessed by endometrial changes) have been observed in women even with high doses of spironolactone.[16][17] As such, the progestogenic potency of spironolactone appears to be below the level of clinical significance in humans.[16][17] Moreover, the menstrual abnormalities associated with spironolactone must have a different cause.[16][17] Suggestions for other possible mechanisms for the menstrual disturbances of spironolactone include interference with the hypothalamic–pituitary–gonadal axis, inhibition of enzymatic steroidogenesis,[29] and mixed estrogenic and antiestrogenic activity.[14][16][17]
Antigonadotropic effects
Pure AR antagonists like flutamide and bicalutamide are potent progonadotropins with indirect estrogenic activity in males.[120] This is because they block the AR in the pituitary gland and hypothalamus and thereby inhibit the negative feedback of androgens on the hypothalamic–pituitary–gonadal axis (HPG axis).[120] This, in turn, results in increased gonadotropin secretion, activation of gonadal steroidogenesis, and an up to 2-fold increase in testosterone levels and 2.5-fold increase in estradiol levels.[121] Conversely, AR antagonists that are also progestogens, like cyproterone acetate, are not progonadotropic, as activation of the PR is antigonadotropic and preserves negative feedback on the HPG axis, and these medications are indeed potently antigonadotropic in clinical practice.[120]
Although spironolactone is an AR antagonist with no significant progestogenic effects in women even at high dosages and hence is a pure-like AR antagonist, many studies have not found it to be progonadotropic in men, nor to increase testosterone or estradiol levels.[30][122][123] Moreover, spironolactone is also said to possess very little or no antigonadotropic activity (in terms of lowering gonadotropin levels to below normal) even at high dosages,[13][124] although some conflicting reports exist.[125][126][127] Nonetheless, since spironolactone does not generally increase gonadotropin levels in spite of inhibition of androgen signaling, it must have some degree of antigonadotropic activity sufficient to at least keep the HPG axis from being upregulated.[120] As estrogens are antigonadotropic similarly to progestogens, and as SERM-like activity has been described for spironolactone, the antigonadotropic effects of spironolactone may be due to estrogenic activity.[14]
Glucocorticoid activity
Spironolactone weakly binds to and acts as an antagonist of the GR, showing antiglucocorticoid properties, but to a significant degree only at very high concentrations that are probably not clinically relevant.[112][128][129]
Most studies have found that spironolactone has no effect on cortisol levels.[16] However, some studies have observed increased cortisol levels with spironolactone treatment.[130][131] It is thought that this is due to the antimineralocorticoid activity of spironolactone, which prevents negative feedback of mineralocorticoids like aldosterone on the hypothalamic–pituitary–adrenal axis (HPA axis), and thereby upregulates adrenocorticotropic hormone (ACTH) and adrenal gland synthesis of corticosteroids such as cortisol and aldosterone.[130][131] Although spironolactone usually doesn't affect cortisol levels, it does significantly increase concentrations of aldosterone.[132]
Spironolactone has been shown to weakly inhibit 11β-hydroxylase in vitro.[23][133] This enzyme is responsible for the transformation of 11-deoxycorticosterone into corticosterone and of 11-deoxycortisol into cortisol.[13] The clinical significance of this action, if any, is unclear.[23][133][13] Spironolactone notably does not decrease cortisol or aldosterone levels.[16][132]
Other activities
Spironolactone is an agonist of the pregnane X receptor (PXR), a xenobiotic-sensing receptor.[21][134][20] By activating the PXR, spironolactone induces the expression of cytochrome P450 CYP3A enzymes and of the ATP-binding cassette transporter (ABC transporters) P-glycoprotein (multidrug resistance protein 1; MRP1; ABCB1) and multidrug resistance protein 2 (MRP2; ABCC2).[21][134][20][135][19][136][137][138][22] These proteins are involved in the metabolism and elimination of xenobiotics, and as a result, their induction by spironolactone may contribute to drug interactions of spironolactone.[21][134][20] Examples of such interactions include oral digoxin and estradiol.[136][79]
There is evidence that spironolactone may block voltage-dependent Ca2+ channels.[139][140] It has also been found to block voltage-gated potassium (K+) channels.[141]
Spironolactone has been identified as an inhibitor of NRG1‐ERBB4 signaling.[142]
Spironolactone has been found to act as a potent inhibitor of the pannexin 1 channel, and this action appears to be involved in its antihypertensive effects independently of MR antagonism.[143]
Hormone levels
A 2 sysreview of 18 studies found that spironolactone shows no significant effects on levels of estrogen, estradiol, testosterone, androstened, dehydroep sulfate, luteinizing hormone, or follicle-stimulating hormone in women.[145] A 2017 hybrid systematic review reported that data from 50 studies on androgen levels with spironolactone in women were equivocal.[67] A 1993 review reported that changes in hormone levels with spironolactone were very heterogeneous, with most changes not achieving significance.[16] Levels of cortisol were unchanged in all studies (four total) and levels of dehydroepiandrosterone sulfate were unchanged in all but one of seven studies.[16] However, it was reported that testosterone levels were decreased in 81% of the studies (13 of 16).[16] However, neither of the two placebo-controlled trials in the review found a significant difference in testosterone levels between the placebo and treatment groups.[16] A 1991 review reported that the influences of spironolactone on androgen levels in women were variable and inconsistent.[78]
Spironolactone has shown no significant effect on levels of testosterone, estradiol, luteinizing hormone, and follicle-stimulating hormone in men.[146][78]
No or only small changes in cortisol levels have been observed in clinical studies with spironolactone.[147][148][149][150][151][152]
The influence of canrenoate potassium on cortisol levels has been studied.[153][154][155][156][157][158]
Spironolactone has no influence on sex hormone-binding globulin levels in women or men.[159][66]
References
- Sica, Domenic A. (2005). "Pharmacokinetics and Pharmacodynamics of Mineralocorticoid Blocking Agents and their Effects on Potassium Homeostasis". Heart Failure Reviews. 10 (1): 23–29. doi:10.1007/s10741-005-2345-1. ISSN 1382-4147. PMID 15947888. S2CID 21437788.
- Agusti, Géraldine; Bourgeois, Sandrine; Cartiser, Nathalie; Fessi, Hatem; Le Borgne, Marc; Lomberget, Thierry (2013). "A safe and practical method for the preparation of 7α-thioether and thioester derivatives of spironolactone". Steroids. 78 (1): 102–107. doi:10.1016/j.steroids.2012.09.005. ISSN 0039-128X. PMID 23063964. S2CID 8992318.
- International Agency for Research on Cancer; World Health Organization (2001). Some Thyrotropic Agents. World Health Organization. pp. 325–. ISBN 978-92-832-1279-9.
- Pere Ginés; Vicente Arroyo; Juan Rodés; Robert W. Schrier (15 April 2008). Ascites and Renal Dysfunction in Liver Disease: Pathogenesis, Diagnosis, and Treatment. John Wiley & Sons. pp. 229, 231. ISBN 978-1-4051-4370-7.
The most rational treatment of cirrhotic patients with ascites appears to be the administration of an aldosterone antagonist. A stepwise equential therapy with increasing oral doses of an aldosterone antagonist (up to 400 mg/day) may be effective in mobilizing ascites in 60-80% of non-azotemic cirrhotic patients with ascites who do not respond to bed rest and dietary sodium restriction (11,12,74). The effective dosage of aldosterone antagonists depends on plasma aldosterone levels (75). Patients with moderately increased plasma levels require low doses of those drugs (100-150 mg/day), whereas patients with marked hyperaldosteronism may require as much as 200-400 mg/day. A further increase of the dosage up to 500-600 mg/day is of limited usefulness (11,12).
- Bell MG, Gernert DL, Grese TA, Belvo MD, Borromeo PS, Kelley SA, Kennedy JH, Kolis SP, Lander PA, Richey R, Sharp VS, Stephenson GA, Williams JD, Yu H, Zimmerman KM, Steinberg MI, Jadhav PK (2007). "(S)-N-{3-[1-cyclopropyl-1-(2,4-difluoro-phenyl)-ethyl]-1H-indol-7-yl}-methanesulfonamide: a potent, nonsteroidal, functional antagonist of the mineralocorticoid receptor". J. Med. Chem. 50 (26): 6443–5. doi:10.1021/jm701186z. PMID 18038968.
- Hasui T, Matsunaga N, Ora T, Ohyabu N, Nishigaki N, Imura Y, Igata Y, Matsui H, Motoyaji T, Tanaka T, Habuka N, Sogabe S, Ono M, Siedem CS, Tang TP, Gauthier C, De Meese LA, Boyd SA, Fukumoto S (2011). "Identification of benzoxazin-3-one derivatives as novel, potent, and selective nonsteroidal mineralocorticoid receptor antagonists". J. Med. Chem. 54 (24): 8616–31. doi:10.1021/jm2011645. PMID 22074142.
- Hu X, Li S, McMahon EG, Lala DS, Rudolph AE (2005). "Molecular mechanisms of mineralocorticoid receptor antagonism by eplerenone". Mini Rev Med Chem. 5 (8): 709–18. doi:10.2174/1389557054553811. PMID 16101407.
- Yang C, Shen HC, Wu Z, Chu HD, Cox JM, Balsells J, Crespo A, Brown P, Zamlynny B, Wiltsie J, Clemas J, Gibson J, Contino L, Lisnock J, Zhou G, Garcia-Calvo M, Bateman T, Xu L, Tong X, Crook M, Sinclair P (2013). "Discovery of novel oxazolidinedione derivatives as potent and selective mineralocorticoid receptor antagonists". Bioorg. Med. Chem. Lett. 23 (15): 4388–92. doi:10.1016/j.bmcl.2013.05.077. PMID 23777778.
- Pitt B, Filippatos G, Gheorghiade M, Kober L, Krum H, Ponikowski P, Nowack C, Kolkhof P, Kim SY, Zannad F (June 2012). "Rationale and design of ARTS: a randomized, double-blind study of BAY 94-8862 in patients with chronic heart failure and mild or moderate chronic kidney disease". Eur. J. Heart Fail. 14 (6): 668–75. doi:10.1093/eurjhf/hfs061. PMID 22562554.
- Meyers MJ, Arhancet GB, Hockerman SL, Chen X, Long SA, Mahoney MW, Rico JR, Garland DJ, Blinn JR, Collins JT, Yang S, Huang HC, McGee KF, Wendling JM, Dietz JD, Payne MA, Homer BL, Heron MI, Reitz DB, Hu X (2010). "Discovery of (3S,3aR)-2-(3-chloro-4-cyanophenyl)-3-cyclopentyl-3,3a,4,5-tetrahydro-2H-benzo[g]indazole-7-carboxylic acid (PF-3882845), an orally efficacious mineralocorticoid receptor (MR) antagonist for hypertension and nephropathy". J. Med. Chem. 53 (16): 5979–6002. doi:10.1021/jm100505n. PMID 20672822.
- "The Binding Database (Binding DB)". University of California, San Diego and ChemAxon. Retrieved 21 December 2017.
- Roth, BL; Driscol, J. "PDSP Ki Database". Psychoactive Drug Screening Program (PDSP). University of North Carolina at Chapel Hill and the United States National Institute of Mental Health. Retrieved 14 August 2017.
- Kenneth L. Becker (2001). Principles and Practice of Endocrinology and Metabolism. Lippincott Williams & Wilkins. pp. 708, 777, 1087, 1196. ISBN 978-0-7817-1750-2.
Spironolactone has been used successfully in dosages of 100 to 200 mg daily for the treatment of idiopathic hirsutism and hirsutism associated with polycystic ovarian disease (see Chaps. 96 and 101).184 [...] Spironolactone also is both an antiandrogen and a progestagen, and this explains many of its distressing side effects; decreased libido, mastodynia, and gynecomastia may occur in 50% or more of men, and menometrorrhagia and breast pain may occur in an equally large number of women taking the drug.27
- Sabbadin C, Andrisani A, Zermiani M, Donà G, Bordin L, Ragazzi E, Boscaro M, Ambrosini G, Armanini D (2016). "Spironolactone and intermenstrual bleeding in polycystic ovary syndrome with normal BMI". J. Endocrinol. Invest. 39 (9): 1015–21. doi:10.1007/s40618-016-0466-0. PMID 27072668. S2CID 34201900.
- Levy J, Burshell A, Marbach M, Afllalo L, Glick SM (March 1980). "Interaction of spironolactone with oestradiol receptors in cytosol". J. Endocrinol. 84 (3): 371–9. doi:10.1677/joe.0.0840371. PMID 7391714.
- McMullen GR, Van Herle AJ (December 1993). "Hirsutism and the effectiveness of spironolactone in its management". J. Endocrinol. Invest. 16 (11): 925–32. doi:10.1007/BF03348960. PMID 8144871. S2CID 42231952.
- Nakajima ST, Brumsted JR, Riddick DH, Gibson M (1989). "Absence of progestational activity of oral spironolactone". Fertil. Steril. 52 (1): 155–8. doi:10.1016/s0015-0282(16)60807-5. PMID 2744183.
- Delyani, John A (2000). "Mineralocorticoid receptor antagonists: The evolution of utility and pharmacology". Kidney International. 57 (4): 1408–1411. doi:10.1046/j.1523-1755.2000.00983.x. ISSN 0085-2538. PMID 10760075.
- Pelkonen O, Mäenpää J, Taavitsainen P, Rautio A, Raunio H (1998). "Inhibition and induction of human cytochrome P450 (CYP) enzymes". Xenobiotica. 28 (12): 1203–53. doi:10.1080/004982598238886. PMID 9890159. Archived (PDF) from the original on 2015-09-24.
- Rigalli JP, Ruiz ML, Perdomo VG, Villanueva SS, Mottino AD, Catania VA (July 2011). "Pregnane X receptor mediates the induction of P-glycoprotein by spironolactone in HepG2 cells". Toxicology. 285 (1–2): 18–24. doi:10.1016/j.tox.2011.03.015. PMID 21459122.
- Lehmann JM, McKee DD, Watson MA, Willson TM, Moore JT, Kliewer SA (September 1998). "The human orphan nuclear receptor PXR is activated by compounds that regulate CYP3A4 gene expression and cause drug interactions". J. Clin. Invest. 102 (5): 1016–23. doi:10.1172/JCI3703. PMC 508967. PMID 9727070.
- Christians U, Schmitz V, Haschke M (December 2005). "Functional interactions between P-glycoprotein and CYP3A in drug metabolism". Expert Opin Drug Metab Toxicol. 1 (4): 641–54. doi:10.1517/17425255.1.4.641. PMID 16863430. S2CID 17742146.
- Cheng SC, Suzuki K, Sadee W, Harding BW (October 1976). "Effects of spironolactone, canrenone and canrenoate-K on cytochrome P450, and 11beta- and 18-hydroxylation in bovine and human adrenal cortical mitochondria". Endocrinology. 99 (4): 1097–106. doi:10.1210/endo-99-4-1097. PMID 976190.
- Maron BA, Leopold JA (2008). "Mineralocorticoid receptor antagonists and endothelial function". Curr Opin Investig Drugs. 9 (9): 963–9. PMC 2967484. PMID 18729003.
- Michelle A. Clark; Richard A. Harvey; Richard Finkel; Jose A. Rey; Karen Whalen (15 December 2011). Pharmacology. Lippincott Williams & Wilkins. pp. 286, 337. ISBN 978-1-4511-1314-3.
- Juruena MF, Pariante CM, Papadopoulos AS, Poon L, Lightman S, Cleare AJ (2013). "The role of mineralocorticoid receptor function in treatment-resistant depression". J. Psychopharmacol. (Oxford). 27 (12): 1169–79. doi:10.1177/0269881113499205. PMID 23904409. S2CID 41678453.
- Yamasaki K, Sawaki M, Noda S, Muroi T, Takakura S, Mitoma H, Sakamoto S, Nakai M, Yakabe Y (2004). "Comparison of the Hershberger assay and androgen receptor binding assay of twelve chemicals". Toxicology. 195 (2–3): 177–86. doi:10.1016/j.tox.2003.09.012. PMID 14751673.
- Corvol P, Michaud A, Menard J, Freifeld M, Mahoudeau J (July 1975). "Antiandrogenic effect of spirolactones: mechanism of action". Endocrinology. 97 (1): 52–8. doi:10.1210/endo-97-1-52. PMID 166833.
- Donald W. Seldin; Gerhard H. Giebisch (23 September 1997). Diuretic Agents: Clinical Physiology and Pharmacology. Academic Press. pp. 630–632. ISBN 978-0-08-053046-8. Archived from the original on 4 July 2014.
The incidence of spironolactone in men is dose related. It is estimated that 50% of men treated with ≥150 mg/day of spironolactone will develop gynecomastia. The degree of gynecomastia varies considerably from patient to patient but in most instances causes mild symptoms. Associated breast tenderness is common but an inconsistent feature.
- Loriaux, D. Lynn (November 1976). "Spironolactone and endocrine dysfunction". Annals of Internal Medicine. 85 (5): 630–6. doi:10.7326/0003-4819-85-5-630. PMID 984618.
- Cutler GB, Pita JC, Rifka SM, Menard RH, Sauer MA, Loriaux DL (1978). "SC 25152: A potent mineralocorticoid antagonist with reduced affinity for the 5 alpha-dihydrotestosterone receptor of human and rat prostate". J. Clin. Endocrinol. Metab. 47 (1): 171–5. doi:10.1210/jcem-47-1-171. PMID 263288.
- Eil C, Edelson SK (July 1984). "The use of human skin fibroblasts to obtain potency estimates of drug binding to androgen receptors". J. Clin. Endocrinol. Metab. 59 (1): 51–5. doi:10.1210/jcem-59-1-51. PMID 6725525.
- Pita JC, Lippman ME, Thompson EB, Loriaux DL (December 1975). "Interaction of spironolactone and digitalis with the 5 alpha-dihydrotestosterone (DHT) receptor of rat ventral prostate". Endocrinology. 97 (6): 1521–7. doi:10.1210/endo-97-6-1521. PMID 173527.
- Liang T, Rasmusson GH, Brooks JR (July 1983). "12. Androgens: Pharmacodynamics and antagonists. Biochemical and biological studies with 4-aza-steroidal 5 alpha-reductase inhibitors". J. Steroid Biochem. 19 (1A): 385–90. doi:10.1016/s0022-4731(83)80051-x. PMID 6887871.
- Hammerstein, J. (1990). "Antiandrogens: Clinical Aspects". Hair and Hair Diseases. pp. 827–886. doi:10.1007/978-3-642-74612-3_35. ISBN 978-3-642-74614-7.
- Hecker A, Hasan SH, Neumann F (December 1980). "Disturbances in sexual differentiation of rat foetuses following spironolactone treatment". Acta Endocrinol. 95 (4): 540–5. doi:10.1530/acta.0.0950540. PMID 7456979.
- Di Lorenzo G, Autorino R, Perdonà S, De Placido S (December 2005). "Management of gynaecomastia in patients with prostate cancer: a systematic review". Lancet Oncol. 6 (12): 972–9. doi:10.1016/S1470-2045(05)70464-2. PMID 16321765.
- Labrie F (December 1993). "Mechanism of action and pure antiandrogenic properties of flutamide". Cancer. 72 (12 Suppl): 3816–27. doi:10.1002/1097-0142(19931215)72:12+<3816::AID-CNCR2820721711>3.0.CO;2-3. PMID 8252497. S2CID 2195250.
- Luthy IA, Begin DJ, Labrie F (November 1988). "Androgenic activity of synthetic progestins and spironolactone in androgen-sensitive mouse mammary carcinoma (Shionogi) cells in culture". Journal of Steroid Biochemistry. 31 (5): 845–52. doi:10.1016/0022-4731(88)90295-6. PMID 2462135.
- Térouanne B, Tahiri B, Georget V, et al. (February 2000). "A stable prostatic bioluminescent cell line to investigate androgen and antiandrogen effects". Molecular and Cellular Endocrinology. 160 (1–2): 39–49. doi:10.1016/S0303-7207(99)00251-8. PMID 10715537. S2CID 13737435.
- Marc A. Fritz; Leon Speroff (20 December 2010). Clinical Gynecologic Endocrinology and Infertility. Lippincott Williams & Wilkins. p. 80. ISBN 978-0-7817-7968-5. Archived from the original on 4 July 2014. Retrieved 27 May 2012.
- Attard G, Reid AH, Olmos D, de Bono JS (June 2009). "Antitumor activity with CYP17 blockade indicates that castration-resistant prostate cancer frequently remains hormone driven". Cancer Research. 69 (12): 4937–40. doi:10.1158/0008-5472.CAN-08-4531. PMID 19509232.
- Sundar S, Dickinson PD (2012). "Spironolactone, a possible selective androgen receptor modulator, should be used with caution in patients with metastatic carcinoma of the prostate". BMJ Case Rep. 2012: bcr1120115238. doi:10.1136/bcr.11.2011.5238. PMC 3291010. PMID 22665559.
- Flynn T, Guancial EA, Kilari M, Kilari D (2016). "Case Report: Spironolactone Withdrawal Associated With a Dramatic Response in a Patient With Metastatic Castrate-Resistant Prostate Cancer". Clin Genitourin Cancer. 15 (1): e95–e97. doi:10.1016/j.clgc.2016.08.006. PMID 27641657. S2CID 38441469.
- Dhondt, Bert; Buelens, Sarah; Van Besien, Jeroen; Beysens, Matthias; De Bleser, Elise; Ost, Piet; Lumen, Nicolaas (26 November 2018). "Abiraterone and spironolactone in prostate cancer: a combination to avoid". Acta Clinica Belgica. 74 (6): 439–444. doi:10.1080/17843286.2018.1543827. hdl:1854/LU-8582726. PMID 30477405. S2CID 53738534.
- Rybikowski S, Maurin C, Deturmeny J, Delaporte V, Lechevallier E, Coulange C (February 2010). "PSA et spironolactone" [PSA and spironolactone]. Prog. Urol. (in French). 20 (2): 154–7. doi:10.1016/j.purol.2009.04.002. PMID 20142058.
- Scott WW, Menon M, Walsh PC (April 1980). "Hormonal Therapy of Prostatic Cancer". Cancer. 45 (Suppl 7): 1929–1936. doi:10.1002/cncr.1980.45.s7.1929. PMID 29603164. S2CID 4492779.
- Smith JA (January 1987). "New methods of endocrine management of prostatic cancer". J. Urol. 137 (1): 1–10. doi:10.1016/S0022-5347(17)43855-9. PMID 3540320.
- H.J.T. Coelingh Benni; H.M. Vemer (15 December 1990). Chronic Hyperandrogenic Anovulation. CRC Press. pp. 152–. ISBN 978-1-85070-322-8.
- Armanini D, Karbowiak I, Goi A, Mantero F, Funder JW (1985). "In-vivo metabolites of spironolactone and potassium canrenoate: determination of potential anti-androgenic activity by a mouse kidney cytosol receptor assay". Clin. Endocrinol. 23 (4): 341–7. doi:10.1111/j.1365-2265.1985.tb01090.x. PMID 4064345. S2CID 20161982.
- Andriulli A, Arrigoni A, Gindro T, Karbowiak I, Buzzetti G, Armanini D (1989). "Canrenone and androgen receptor-active materials in plasma of cirrhotic patients during long-term K-canrenoate or spironolactone therapy". Digestion. 44 (3): 155–62. doi:10.1159/000199905. PMID 2697627.
- Jashin J. Wu (18 October 2012). Comprehensive Dermatologic Drug Therapy E-Book. Elsevier Health Sciences. pp. 364–. ISBN 978-1-4557-3801-4.
Spironolactone is an aldosterone antagonist and a relatively weak antiandrogen that blocks the AR and inhibits androgen biosynthesis. Spironolactone does not inhibit 5α-reductase. [...] The progestational activity of spironolactone is variable. The drug influences the ratio of luteinizing hormone (LH) to follicle-stimulating hormone (FSH) by reducing the response of LH to GnRH. [...] In a dose range of 25-200 mg a linear relationship between a single dose of spironolactone and plasma levels of canrenone occurs within 96 hours. [...] Common doses [of spironolactone for dermatological indications] range between 50 and 200 mg daily, with 100 mg daily typically being better tolerated than higher dosages.20
- Doggrell SA, Brown L (2001). "The spironolactone renaissance". Expert Opin Investig Drugs. 10 (5): 943–54. doi:10.1517/13543784.10.5.943. PMID 11322868. S2CID 39820875.
- Shaw JC (November 1996). "Antiandrogen therapy in dermatology". Int. J. Dermatol. 35 (11): 770–8. doi:10.1111/j.1365-4362.1996.tb02970.x. PMID 8915726. S2CID 39334280.
- Tremblay RR (May 1986). "Treatment of hirsutism with spironolactone". Clin Endocrinol Metab. 15 (2): 363–71. doi:10.1016/S0300-595X(86)80030-5. PMID 2941190.
- Haff , G. Gregory; Triplett , N. Travis (23 September 2015). Essentials of Strength Training and Conditioning 4th Edition. Human Kinetics. pp. 76–. ISBN 978-1-4925-0162-6.
- Brown TR, Rothwell SW, Sultan C, Migeon CJ (June 1981). "Inhibition of androgen binding in human foreskin fibroblasts by antiandrogens". Steroids. 37 (6): 635–48. doi:10.1016/S0039-128X(81)90173-2. PMID 6457421. S2CID 88959.
- Breiner M, Romalo G, Schweikert HU (August 1986). "Inhibition of androgen receptor binding by natural and synthetic steroids in cultured human genital skin fibroblasts". Klinische Wochenschrift. 64 (16): 732–7. doi:10.1007/BF01734339. PMID 3762019. S2CID 34846760.
- Breiner M, Romalo G, Schweikert HU (1986). "Inhibition of androgen receptor binding by drugs in cultured human genital skin fibroblasts". Acta Endocrinologica. 113 (1_Suppl): S152. doi:10.1530/acta.0.111S152. ISSN 0804-4643.
- Diamanti-Kandarakis E, Tolis G, Duleba AJ (1995). "Androgens and therapeutic aspects of antiandrogens in women". J. Soc. Gynecol. Investig. 2 (4): 577–92. doi:10.1177/107155769500200401. PMID 9420861. S2CID 32242838.
- Lobo RA, Shoupe D, Serafini P, Brinton D, Horton R (February 1985). "The effects of two doses of spironolactone on serum androgens and anagen hair in hirsute women". Fertil. Steril. 43 (2): 200–5. doi:10.1016/S0015-0282(16)48373-1. PMID 3967781.
- Brown, Julie; Farquhar, Cindy; Lee, Olivia; Toomath, Robyn; Jepson, Ruth G (2009). "Spironolactone versus placebo or in combination with steroids for hirsutism and/or acne". Cochrane Database of Systematic Reviews (2): CD000194. doi:10.1002/14651858.CD000194.pub2. ISSN 1465-1858. PMID 19370553.
- Shaw JC (October 1996). "Antiandrogen and hormonal treatment of acne". Dermatol Clin. 14 (4): 803–11. doi:10.1016/S0733-8635(05)70405-8. PMID 9238337.
- Erenus M, Gürbüz O, Durmuşoğlu F, Demirçay Z, Pekin S (April 1994). "Comparison of the efficacy of spironolactone versus flutamide in the treatment of hirsutism". Fertil. Steril. 61 (4): 613–6. doi:10.1016/S0015-0282(16)56634-5. PMID 8150100.
- Cusan L, Dupont A, Gomez JL, Tremblay RR, Labrie F (February 1994). "Comparison of flutamide and spironolactone in the treatment of hirsutism: a randomized controlled trial". Fertil. Steril. 61 (2): 281–7. doi:10.1016/S0015-0282(16)56518-2. PMID 8299783.
- Goodfellow, A.; Alaghband-Zadeh, J.; Carter, G.; Cream, J.J.; Holland, S.; Scully, J.; Wise, P. (1984). "Oral spironolactone improves acne vulgaris and reduces sebum excretion". British Journal of Dermatology. 111 (2): 209–214. doi:10.1111/j.1365-2133.1984.tb04045.x. ISSN 0007-0963. PMID 6235834. S2CID 24518527.
- Layton AM, Eady EA, Whitehouse H, Del Rosso JQ, Fedorowicz Z, van Zuuren EJ (April 2017). "Oral Spironolactone for Acne Vulgaris in Adult Females: A Hybrid Systematic Review". Am J Clin Dermatol. 18 (2): 169–191. doi:10.1007/s40257-016-0245-x. PMC 5360829. PMID 28155090.
- Mackenzie IS, Morant SV, Wei L, Thompson AM, MacDonald TM (March 2017). "Spironolactone use and risk of incident cancers: a retrospective, matched cohort study". Br J Clin Pharmacol. 83 (3): 653–663. doi:10.1111/bcp.13152. PMC 5306481. PMID 27735065.
- Beckmann K, Garmo H, Lindahl B, Holmberg L, Stattin P, Adolfsson J, Cruickshank JK, Van Hemelrijck M (March 2020). "Spironolactone use is associated with lower prostate cancer risk: a population-wide case-control study". Prostate Cancer Prostatic Dis. 23 (3): 527–533. doi:10.1038/s41391-020-0220-8. PMID 32123316. S2CID 211729232.
- Melmed S, Polonsky KS, Larsen PR, Kronenberg HM (30 November 2015). Williams Textbook of Endocrinology. Elsevier Health Sciences. pp. 743–. ISBN 978-0-323-29738-7.
- Sengupta (1 January 2007). Gynaecology For Postgraduate And Practitioners. Elsevier India. pp. 172–. ISBN 978-81-312-0436-8.
- Bruce R. Carr; Richard E. Blackwell (1998). Textbook of Reproductive Medicine. McGraw-Hill Professional Publishing. p. 261. ISBN 978-0-8385-8893-2.
- Desai; Meena P.; Vijayalakshmi Bhatia & P.S.N. Menon (1 January 2001). Pediatric Endocrine Disorders. Orient Blackswan. p. 167. ISBN 978-81-250-2025-7. Archived from the original on 20 June 2013. Retrieved 28 May 2012.
- Masahashi T, Wu MC, Ohsawa M, et al. (January 1986). "Spironolactone therapy for hyperandrogenic anovulatory women--clinical and endocrinological study". Nihon Sanka Fujinka Gakkai Zasshi. 38 (1): 95–101. PMID 3950464.
- Rose LI, Underwood RH, Newmark SR, Kisch ES, Williams GH (October 1977). "Pathophysiology of spironolactone-induced gynecomastia". Annals of Internal Medicine. 87 (4): 398–403. doi:10.7326/0003-4819-87-4-398. PMID 907238.
- Haynes BA, Mookadam F (August 2009). "Male gynecomastia". Mayo Clinic Proceedings. 84 (8): 672. doi:10.4065/84.8.672. PMC 2719518. PMID 19648382.
- Colby HD (1981). "Chemical suppression of steroidogenesis". Environ. Health Perspect. 38: 119–27. doi:10.1289/ehp.8138119. PMC 1568425. PMID 6786868.
- Shaw JC (February 1991). "Spironolactone in dermatologic therapy". J. Am. Acad. Dermatol. 24 (2 Pt 1): 236–43. doi:10.1016/0190-9622(91)70034-Y. PMID 1826112.
- Leinung MC, Feustel PJ, Joseph J (2018). "Hormonal Treatment of Transgender Women with Oral Estradiol". Transgend Health. 3 (1): 74–81. doi:10.1089/trgh.2017.0035. PMC 5944393. PMID 29756046.
- Serafini PC, Catalino J, Lobo RA (August 1985). "The effect of spironolactone on genital skin 5 alpha-reductase activity". Journal of Steroid Biochemistry. 23 (2): 191–4. doi:10.1016/0022-4731(85)90236-5. PMID 4033118.
- Wong IL, Morris RS, Chang L, Spahn MA, Stanczyk FZ, Lobo RA (January 1995). "A prospective randomized trial comparing finasteride to spironolactone in the treatment of hirsute women". The Journal of Clinical Endocrinology and Metabolism. 80 (1): 233–8. doi:10.1210/jcem.80.1.7829618. PMID 7829618.
- Miles RA, Cassidenti DL, Carmina E, Gentzschein E, Stanczyk FZ, Lobo RA (October 1992). "Cutaneous application of an androstenedione gel as an in vivo test of 5 alpha-reductase activity in women". Fertility and Sterility. 58 (4): 708–12. doi:10.1016/S0015-0282(16)55316-3. PMID 1426314.
- Keleştimur F, Everest H, Unlühizarci K, Bayram F, Sahin Y (March 2004). "A comparison between spironolactone and spironolactone plus finasteride in the treatment of hirsutism". European Journal of Endocrinology. 150 (3): 351–4. doi:10.1530/eje.0.1500351. PMID 15012621. S2CID 32780296.
- Satoh T, Itoh S, Seki T, Itoh S, Nomura N, Yoshizawa I (October 2002). "On the inhibitory action of 29 drugs having side effect gynecomastia on estrogen production". The Journal of Steroid Biochemistry and Molecular Biology. 82 (2–3): 209–16. doi:10.1016/S0960-0760(02)00154-1. PMID 12477487. S2CID 9972497.
- Tremblay MR, Luu-The V, Leblanc G, Noël P, Breton E, Labrie F, Poirier D (1999). "Spironolactone-related inhibitors of type II 17beta-hydroxysteroid dehydrogenase: chemical synthesis, receptor binding affinities, and proliferative/antiproliferative activities". Bioorg. Med. Chem. 7 (6): 1013–23. doi:10.1016/s0968-0896(98)00260-0. PMID 10428369.
- Rifka SM, Pita JC, Vigersky RA, Wilson YA, Loriaux DL (1978). "Interaction of digitalis and spironolactone with human sex steroid receptors". J. Clin. Endocrinol. Metab. 46 (2): 338–44. doi:10.1210/jcem-46-2-338. PMID 86546.
- Fernandez MD, Carter GD, Palmer TN (January 1983). "The interaction of canrenone with oestrogen and progesterone receptors in human uterine cytosol". Br J Clin Pharmacol. 15 (1): 95–101. doi:10.1111/j.1365-2125.1983.tb01470.x. PMC 1427833. PMID 6849751.
- Ralph I. Dorfman (5 December 2016). Steroidal Activity in Experimental Animals and Man. Elsevier Science. pp. 371–. ISBN 978-1-4832-7299-3.
- Moghetti P, Castello R, Zamberlan N, Rossini M, Gatti D, Negri C, Tosi F, Muggeo M, Adami S (1999). "Spironolactone, but not flutamide, administration prevents bone loss in hyperandrogenic women treated with gonadotropin-releasing hormone agonist". J. Clin. Endocrinol. Metab. 84 (4): 1250–4. doi:10.1210/jcem.84.4.5606. PMID 10199763. S2CID 36382302.
- Carbone LD, Cross JD, Raza SH, Bush AJ, Sepanski RJ, Dhawan S, Khan BQ, Gupta M, Ahmad K, Khouzam RN, Dishmon DA, Nesheiwat JP, Hajjar MA, Chishti WA, Nasser W, Khan M, Womack CR, Cho T, Haskin AR, Weber KT (2008). "Fracture risk in men with congestive heart failure risk reduction with spironolactone". J. Am. Coll. Cardiol. 52 (2): 135–8. doi:10.1016/j.jacc.2008.03.039. PMID 18598893. S2CID 28002410.
- Ghosh M, Majumdar SR (2014). "Antihypertensive medications, bone mineral density, and fractures: a review of old cardiac drugs that provides new insights into osteoporosis". Endocrine. 46 (3): 397–405. doi:10.1007/s12020-014-0167-4. PMID 24504763. S2CID 19284432.
- Moghetti, Paolo; Castello, Roberto; Zamberlan, Nicoletta; Rossini, Maurizio; Gatti, Davide; Negri, Carlo; Tosi, Flavia; Muggeo, Michele; Adami, Silvano (1999). "Authors' Response: Spironolactone But Not Flutamide Administration Prevents Bone Loss in Hyperandrogenic Women Treated with Gonadotropin-Releasing Hormone Agonist". The Journal of Clinical Endocrinology & Metabolism. 84 (12): 4747–b–4747. doi:10.1210/jcem.84.12.4747b. ISSN 0021-972X.
- Zhou J, Ng S, Adesanya-Famuiya O, Anderson K, Bondy CA (September 2000). "Testosterone inhibits estrogen-induced mammary epithelial proliferation and suppresses estrogen receptor expression". FASEB Journal. 14 (12): 1725–30. doi:10.1096/fj.99-0863com. PMID 10973921. S2CID 17172449.
- Ruggiero RJ, Likis FE (2002). "Estrogen: physiology, pharmacology, and formulations for replacement therapy". Journal of Midwifery & Women's Health. 47 (3): 130–8. doi:10.1016/s1526-9523(02)00233-7. PMID 12071379.
- Kuhl H (2005). "Pharmacology of estrogens and progestogens: influence of different routes of administration" (PDF). Climacteric. 8 (Suppl 1): 3–63. doi:10.1080/13697130500148875. PMID 16112947. S2CID 24616324. Archived (PDF) from the original on 2016-08-22.
- Poirier D (2003). "Inhibitors of 17 beta-hydroxysteroid dehydrogenases". Curr. Med. Chem. 10 (6): 453–77. doi:10.2174/0929867033368222. PMID 12570693.
- Poirier D (2009). "Advances in development of inhibitors of 17beta hydroxysteroid dehydrogenases". Anticancer Agents Med Chem. 9 (6): 642–60. doi:10.2174/187152009788680000. PMID 19601747.
- Sam KM, Auger S, Luu-The V, Poirier D (1995). "Steroidal spiro-gamma-lactones that inhibit 17 beta-hydroxysteroid dehydrogenase activity in human placental microsomes". J. Med. Chem. 38 (22): 4518–28. doi:10.1021/jm00022a018. PMID 7473580.
- Biggar RJ, Andersen EW, Wohlfahrt J, Melbye M (December 2013). "Spironolactone use and the risk of breast and gynecologic cancers". Cancer Epidemiol. 37 (6): 870–5. doi:10.1016/j.canep.2013.10.004. PMID 24189467.
- Marchais-Oberwinkler S, Henn C, Möller G, Klein T, Negri M, Oster A, Spadaro A, Werth R, Wetzel M, Xu K, Frotscher M, Hartmann RW, Adamski J (2011). "17β-Hydroxysteroid dehydrogenases (17β-HSDs) as therapeutic targets: protein structures, functions, and recent progress in inhibitor development". J. Steroid Biochem. Mol. Biol. 125 (1–2): 66–82. doi:10.1016/j.jsbmb.2010.12.013. PMID 21193039. S2CID 23767100.
- Soubhye J, Alard IC, van Antwerpen P, Dufrasne F (2015). "Type 2 17-β hydroxysteroid dehydrogenase as a novel target for the treatment of osteoporosis". Future Med Chem. 7 (11): 1431–56. doi:10.4155/fmc.15.74. PMID 26230882.
- Fabian CJ, Kimler BF (March 2005). "Selective estrogen-receptor modulators for primary prevention of breast cancer". J. Clin. Oncol. 23 (8): 1644–55. doi:10.1200/JCO.2005.11.005. PMID 15755972.
- Sato K, Matsumoto D, Iizuka F, Aiba-Kojima E, Watanabe-Ono A, Suga H, Inoue K, Gonda K, Yoshimura K (2006). "Anti-androgenic therapy using oral spironolactone for acne vulgaris in Asians". Aesthetic Plast Surg. 30 (6): 689–94. doi:10.1007/s00266-006-0081-0. PMID 17077951. S2CID 13332616.
- Elbers, Laura P.B.; Sjouke, Barbara; Zannad, Faïez; Cicoira, Mariantonietta; Vizzardi, Enrico; Václavík, Jan; Gerdes, Victor E.A.; Squizzato, Alessandro (2016). "Effects of mineralocorticoid receptor antagonists on the risk of thrombosis, bleeding and mortality: A systematic review and meta-analysis of randomized controlled trials". Thrombosis Research. 144: 32–39. doi:10.1016/j.thromres.2016.04.027. ISSN 0049-3848. PMID 27270220.
- Endly DC, Miller RA (August 2017). "Oily Skin: A review of Treatment Options". J Clin Aesthet Dermatol. 10 (8): 49–55. PMC 5605215. PMID 28979664.
- Mackenzie IS, Macdonald TM, Thompson A, Morant S, Wei L (July 2012). "Spironolactone and risk of incident breast cancer in women older than 55 years: retrospective, matched cohort study". BMJ. 345: e4447. doi:10.1136/bmj.e4447. PMC 3396460. PMID 22797844.
- Sabatier P, Amar J, Montastruc F, Rousseau V, Chebane L, Bouhanick B, Montastruc JL (November 2019). "Breast cancer and spironolactone: an observational postmarketing study". Eur. J. Clin. Pharmacol. 75 (11): 1593–1598. doi:10.1007/s00228-019-02740-y. PMID 31418056. S2CID 199668277.
- Wei C, Bovonratwet P, Gu A, Moawad G, Silverberg JI, Friedman AJ (May 2020). "Spironolactone use does not increase the risk of female breast cancer recurrence: A retrospective analysis". J. Am. Acad. Dermatol. 83 (4): 1021–1027. doi:10.1016/j.jaad.2020.05.081. PMID 32446820. S2CID 218873257.
- Heymann WR (July 2020). "Spironolactone and breast cancer: Fear not!". J. Am. Acad. Dermatol. 83 (4): 1008–1009. doi:10.1016/j.jaad.2020.07.104. PMID 32738426. S2CID 220924754.
- Fiore C, Zermiani M, Sabbadin C, Anddrisani A, Ambrosini G, Bordin L, Dona G, Clari G, Ragazzi E, Armanini D (June 2011). "Effect of Spironolactone on Endometrium in Patients with Polycystic Ovary Syndrome" (PDF). Endocrine Reviews. 32 (3 Suppl). ISSN 0163-769X.
- Schane, H. P.; Potts, G. O. (1978). "Oral Progestational Activity of Spironolactone". Journal of Clinical Endocrinology & Metabolism. 47 (3): 691–4. doi:10.1210/jcem-47-3-691. ISSN 0021-972X. PMID 95623.
- Fagart J, Hillisch A, Huyet J, et al. (September 2010). "A new mode of mineralocorticoid receptor antagonism by a potent and selective nonsteroidal molecule". The Journal of Biological Chemistry. 285 (39): 29932–40. doi:10.1074/jbc.M110.131342. PMC 2943305. PMID 20650892.
- Douglas T. Carrell (12 April 2010). Reproductive Endocrinology and Infertility: Integrating Modern Clinical and Laboratory Practice. Springer. pp. 162–163. ISBN 978-1-4419-1435-4. Archived from the original on 4 July 2014. Retrieved 28 May 2012.
- Melmed S, Polonsky KS, Larsen PR, Kronenberg HM (31 May 2011). Williams Textbook of Endocrinology E-Book: Expert Consult. Elsevier Health Sciences. p. 2057. ISBN 978-1-4377-3600-7. Archived from the original on 21 June 2013. Retrieved 27 May 2012.
- Nakhjavani M, Hamidi S, Esteghamati A, Abbasi M, Nosratian-Jahromi S, Pasalar P (October 2009). "Short term effects of spironolactone on blood lipid profile: a 3-month study on a cohort of young women with hirsutism". British Journal of Clinical Pharmacology. 68 (4): 634–7. doi:10.1111/j.1365-2125.2009.03483.x. PMC 2780289. PMID 19843067.
- Eckhard Ottow; Hilmar Weinmann (9 July 2008). Nuclear Receptors As Drug Targets. John Wiley & Sons. p. 410. ISBN 978-3-527-62330-3. Archived from the original on 21 June 2013. Retrieved 28 May 2012.
- Anderson E (2002). "The role of oestrogen and progesterone receptors in human mammary development and tumorigenesis". Breast Cancer Research. 4 (5): 197–201. doi:10.1186/bcr452. PMC 138744. PMID 12223124.
- Schane HP, Potts GO (1978). "Oral progestational activity of spironolactone". J. Clin. Endocrinol. Metab. 47 (3): 691–4. doi:10.1210/jcem-47-3-691. PMID 95623.
- Muhn P, Fuhrmann U, Fritzemeier KH, Krattenmacher R, Schillinger E (June 1995). "Drospirenone: a novel progestogen with antimineralocorticoid and antiandrogenic activity". Ann. N. Y. Acad. Sci. 761 (3): 311–35. Bibcode:1995NYASA.761..311M. doi:10.1111/j.1749-6632.1995.tb31386.x. PMID 7625729. S2CID 36861309.
- Iversen P, Melezinek I, Schmidt A (January 2001). "Nonsteroidal antiandrogens: a therapeutic option for patients with advanced prostate cancer who wish to retain sexual interest and function". BJU International. 87 (1): 47–56. doi:10.1046/j.1464-410x.2001.00988.x. PMID 11121992. S2CID 28215804.
- Mahler C, Verhelst J, Denis L (May 1998). "Clinical pharmacokinetics of the antiandrogens and their efficacy in prostate cancer". Clinical Pharmacokinetics. 34 (5): 405–17. doi:10.2165/00003088-199834050-00005. PMID 9592622. S2CID 25200595.
- Shlomo Melmed (2016). Williams Textbook of Endocrinology. Elsevier Health Sciences. pp. 626–. ISBN 978-0-323-29738-7.
- Stripp B, Taylor AA, Bartter FC, Gillette JR, Loriaux DL, Easley R, Menard RH (1975). "Effect of spironolactone on sex hormones in man". J. Clin. Endocrinol. Metab. 41 (4): 777–81. doi:10.1210/jcem-41-4-777. PMID 1176584.
- Drapier-Faure, Evelyne; Faure, Michel (2006). "Antiandrogens". Hidradenitis Suppurativa. pp. 124–127. doi:10.1007/978-3-540-33101-8_16. ISBN 978-3-540-33100-1.
- Douglas T. Carrell; C. Matthew Peterson (23 March 2010). Reproductive Endocrinology and Infertility: Integrating Modern Clinical and Laboratory Practice. Springer Science & Business Media. pp. 162–. ISBN 978-1-4419-1436-1.
A modest improvement in hirsutism can be anticipated in 70-80% of women using even the minimum of 100 mg of spironolactone per day for 6 months [157]. [...] The most common dosage is 100-200 mg per day in a divided dosage. Women treated with 200 mg/day show a greater reduction in hair shaft diameter than women receiving 100 mg/day [159]. [...] Menstrual irregularity (usually metrorrhagia), is the most common side effect of spironolactone and occurs in over 50% of patients with a dosage of 200 mg/day [159]. [...] Patients must be counseled to use contraception while taking spironolactone because it theoretically can feminize a male fetus.
- Israel Journal of Medical Sciences. Israel Medical Association, National Council for Research and Development. July 1984.
- Jerry Shapiro (12 November 2012). Hair Disorders: Current Concepts in Pathophysiology, Diagnosis and Management, An Issue of Dermatologic Clinics. Elsevier Health Sciences. pp. 186–. ISBN 978-1-4557-7169-1.
- Campen TJ, Fanestil DD (1982). "Spironolactone: a glucocorticoid agonist or antagonist?". Clinical and Experimental Hypertension, Part A. 4 (9–10): 1627–36. doi:10.3109/10641968209061629. PMID 6128090.
- Couette B, Marsaud V, Baulieu EE, Richard-Foy H, Rafestin-Oblin ME (1992). "Spironolactone, an aldosterone antagonist, acts as an antiglucocorticosteroid on the mouse mammary tumor virus promoter". Endocrinology. 130 (1): 430–6. doi:10.1210/endo.130.1.1309341. PMID 1309341.
- Young EA, Lopez JF, Murphy-Weinberg V, Watson SJ, Akil H (September 1998). "The role of mineralocorticoid receptors in hypothalamic-pituitary-adrenal axis regulation in humans". The Journal of Clinical Endocrinology and Metabolism. 83 (9): 3339–45. doi:10.1210/jcem.83.9.5077. PMID 9745451.
- Otte C, Moritz S, Yassouridis A, et al. (January 2007). "Blockade of the mineralocorticoid receptor in healthy men: effects on experimentally induced panic symptoms, stress hormones, and cognition". Neuropsychopharmacology. 32 (1): 232–8. doi:10.1038/sj.npp.1301217. PMID 17035932. S2CID 10624783.
- Diamanti-Kandarakis E (September 1999). "Current aspects of antiandrogen therapy in women". Curr. Pharm. Des. 5 (9): 707–23. doi:10.2174/1381612805666230111201150. PMID 10495361.
- Greiner JW, Rumbaugh RC, Kramer RE, Colby HD (October 1978). "Relation of canrenone to the actions of spironolactone on adrenal cytochrome P-450 dependent enzymes". Endocrinology. 103 (4): 1313–20. doi:10.1210/endo-103-4-1313. PMID 311283.
- Schuetz EG, Brimer C, Schuetz JD (December 1998). "Environmental xenobiotics and the antihormones cyproterone acetate and spironolactone use the nuclear hormone pregnenolone X receptor to activate the CYP3A23 hormone response element". Mol. Pharmacol. 54 (6): 1113–7. doi:10.1124/mol.54.6.1113. PMC 3662300. PMID 9855641.
- Kocarek TA, Schuetz EG, Strom SC, Fisher RA, Guzelian PS (March 1995). "Comparative analysis of cytochrome P4503A induction in primary cultures of rat, rabbit, and human hepatocytes". Drug Metab. Dispos. 23 (3): 415–21. PMID 7628309.
- Ghanem CI, Gómez PC, Arana MC, Perassolo M, Delli Carpini G, Luquita MG, Veggi LM, Catania VA, Bengochea LA, Mottino AD (September 2006). "Induction of rat intestinal P-glycoprotein by spironolactone and its effect on absorption of orally administered digoxin". J. Pharmacol. Exp. Ther. 318 (3): 1146–52. doi:10.1124/jpet.106.105668. PMID 16740618. S2CID 8680890.
- Ruiz ML, Villanueva SS, Luquita MG, Sánchez-Pozzi EJ, Crocenzi FA, Pellegrino JM, Ochoa JE, Vore M, Mottino AD, Catania VA (February 2005). "Mechanisms involved in spironolactone-induced choleresis in the rat. Role of multidrug resistance-associated protein 2". Biochem. Pharmacol. 69 (3): 531–9. doi:10.1016/j.bcp.2004.10.017. PMID 15652244.
- Ruiz ML, Villanueva SS, Luquita MG, Pellegrino JM, Rigalli JP, Arias A, Sánchez Pozzi EJ, Mottino AD, Catania VA (November 2009). "Induction of intestinal multidrug resistance-associated protein 2 (Mrp2) by spironolactone in rats". Eur. J. Pharmacol. 623 (1–3): 103–6. doi:10.1016/j.ejphar.2009.09.014. PMID 19766108.
- Sorrentino R, Autore G, Cirino G, d'Emmanuele de Villa Bianca R, Calignano A, Vanasia M, et al. (2000). "Effect of spironolactone and its metabolites on contractile property of isolated rat aorta rings". J Cardiovasc Pharmacol. 36 (2): 230–235. doi:10.1097/00005344-200008000-00013. PMID 10942165.
- Bendtzen, K.; Hansen, P. R.; Rieneck, K. (2003). "Spironolactone inhibits production of proinflammatory cytokines, including tumour necrosis factor-alpha and interferon-gamma, and has potential in the treatment of arthritis". Clinical and Experimental Immunology. 134 (1): 151–158. doi:10.1046/j.1365-2249.2003.02249.x. ISSN 0009-9104. PMC 1808828. PMID 12974768.
- Gómez, Ricardo; Núñez, Lucía; Caballero, Ricardo; Vaquero, Miguel; Tamargo, Juan; Delpón, Eva (2005). "Spironolactone and its main metabolite canrenoic acid block hKv1.5, Kv4.3 and Kv7.1+minK channels". British Journal of Pharmacology. 146 (1): 146–161. doi:10.1038/sj.bjp.0706302. ISSN 0007-1188. PMC 1576250. PMID 15980874.
- Wehr MC, Hinrichs W, Brzózka MM, Unterbarnscheidt T, Herholt A, Wintgens JP, Papiol S, Soto-Bernardini MC, Kravchenko M, Zhang M, Nave KA, Wichert SP, Falkai P, Zhang W, Schwab MH, Rossner MJ (October 2017). "Spironolactone is an antagonist of NRG1-ERBB4 signaling and schizophrenia-relevant endophenotypes in mice". EMBO Mol Med. 9 (10): 1448–1462. doi:10.15252/emmm.201707691. PMC 5653977. PMID 28743784.
- Good, Miranda E.; Chiu, Yu-Hsin; Poon, Ivan K.H.; Medina, Christopher B.; Butcher, Joshua T.; Mendu, Suresh K.; DeLalio, Leon J.; Lohman, Alexander W.; Leitinger, Norbert; Barrett, Eugene; Lorenz, Ulrike M.; Desai, Bimal N.; Jaffe, Iris Z.; Bayliss, Douglas A.; Isakson, Brant E.; Ravichandran, Kodi S. (2018). "Pannexin 1 Channels as an Unexpected New Target of the Anti-Hypertensive Drug Spironolactone". Circulation Research. 122 (4): 606–615. doi:10.1161/CIRCRESAHA.117.312380. ISSN 0009-7330. PMC 5815904. PMID 29237722.
- Caballero, Ricardo; Moreno, Ignacio; González, Teresa; Arias, Cristina; Valenzuela, Carmen; Delpón, Eva; Tamargo, Juan (2003). "Spironolactone and Its Main Metabolite, Canrenoic Acid, Block Human Ether-a-Go-Go–Related Gene Channels". Circulation. 107 (6): 889–895. doi:10.1161/01.CIR.0000048189.58449.F7. hdl:10261/24675. ISSN 0009-7322. PMID 12591761. S2CID 24556181.
- Rozner RN, Freites-Martinez A, Shapiro J, Geer EB, Goldfarb S, Lacouture ME (November 2018). "Safety of 5α-reductase inhibitors and spironolactone in breast cancer patients receiving endocrine therapies". Breast Cancer Res. Treat. 174 (1): 15–26. doi:10.1007/s10549-018-4996-3. PMC 6773272. PMID 30467659.
- Thompson DF, Carter JR (1993). "Drug-induced gynecomastia". Pharmacotherapy. 13 (1): 37–45. doi:10.1002/j.1875-9114.1993.tb02688.x. PMID 8094898. S2CID 30322620.
- Dhondt B, Buelens S, Van Besien J, Beysens M, De Bleser E, Ost P, Lumen N (November 2018). "Abiraterone and spironolactone in prostate cancer: a combination to avoid". Acta Clin Belg. 74 (6): 439–444. doi:10.1080/17843286.2018.1543827. hdl:1854/LU-8582726. PMID 30477405. S2CID 53738534.
- Abshagen U, Spörl S, L'age M (February 1978). "Non-interaction of spironolactone medication and cortisol metabolism in man". Klin. Wochenschr. 56 (3): 135–8. doi:10.1007/BF01478568. PMID 628197. S2CID 30885047.
- Abshagen U, Spörl S, Schöneshöfer M, L'age M, Oelkers W (April 1978). "Interference of spironolactone therapy with adrenal steroid metabolism in secondary hyperaldosteronism". Klin. Wochenschr. 56 (7): 341–9. doi:10.1007/BF01477394. PMID 642407. S2CID 40979545.
- Millar JA, Fraser R, Mason P, Leckie B, Cumming AM, Robertson JI (September 1984). "Metabolic effects of high dose amiloride and spironolactone: a comparative study in normal subjects". Br J Clin Pharmacol. 18 (3): 369–75. doi:10.1111/j.1365-2125.1984.tb02478.x. PMC 1463638. PMID 6386025.
- Abshagen U, Spörl S, Oelkers W (February 1979). "Influence of spironolactone on serum corticosteroids in primary hyperaldosteronism". Klin. Wochenschr. 57 (4): 173–80. doi:10.1007/BF01477405. PMID 423483. S2CID 39169638.
- Yamaji M, Tsutamoto T, Kawahara C, Nishiyama K, Yamamoto T, Fujii M, Horie M (November 2010). "Effect of eplerenone versus spironolactone on cortisol and hemoglobin A₁(c) levels in patients with chronic heart failure". Am. Heart J. 160 (5): 915–21. doi:10.1016/j.ahj.2010.04.024. PMID 21095280.
- Grottoli S, Giordano R, Maccagno B, Pellegrino M, Ghigo E, Arvat E (October 2002). "The stimulatory effect of canrenoate, a mineralocorticoid antagonist, on the activity of the hypothalamus-pituitary-adrenal axis is abolished by alprazolam, a benzodiazepine, in humans". J. Clin. Endocrinol. Metab. 87 (10): 4616–20. doi:10.1210/jc.2002-020331. PMID 12364444.
- Arvat E, Maccagno B, Giordano R, Pellegrino M, Broglio F, Gianotti L, Maccario M, Camanni F, Ghigo E (July 2001). "Mineralocorticoid receptor blockade by canrenoate increases both spontaneous and stimulated adrenal function in humans". J. Clin. Endocrinol. Metab. 86 (7): 3176–81. doi:10.1210/jcem.86.7.7663. PMID 11443185. S2CID 18906508.
- Wellhoener P, Born J, Fehm HL, Dodt C (October 2004). "Elevated resting and exercise-induced cortisol levels after mineralocorticoid receptor blockade with canrenoate in healthy humans". J. Clin. Endocrinol. Metab. 89 (10): 5048–52. doi:10.1210/jc.2004-0086. PMID 15472204. S2CID 9856650.
- Dodt C, Kern W, Fehm HL, Born J (November 1993). "Antimineralocorticoid canrenoate enhances secretory activity of the hypothalamus-pituitary-adrenocortical (HPA) axis in humans". Neuroendocrinology. 58 (5): 570–4. doi:10.1159/000126592. PMID 8115025.
- Iqbal J, Andrew R, Cruden NL, Kenyon CJ, Hughes KA, Newby DE, Hadoke PW, Walker BR (March 2014). "Displacement of cortisol from human heart by acute administration of a mineralocorticoid receptor antagonist". J. Clin. Endocrinol. Metab. 99 (3): 915–22. doi:10.1210/jc.2013-2049. PMC 4392799. PMID 24423282.
- Born J, Steinbach D, Dodt C, Fehm HL (April 1997). "Blocking of central nervous mineralocorticoid receptors counteracts inhibition of pituitary-adrenal activity in human sleep". J. Clin. Endocrinol. Metab. 82 (4): 1106–10. doi:10.1210/jcem.82.4.3856. PMID 9100581.
- Young, Ronald L.; Goldzieher, Joseph W.; Elkind-Hirsch, Karen (1987). "The endocrine effects of spironolactone used as an antiandrogen". Fertility and Sterility. 48 (2): 223–228. doi:10.1016/S0015-0282(16)59346-7. ISSN 0015-0282. PMID 2956130.