Amitriptyline
 | |
 | |
| Names | |
|---|---|
| Pronunciation | /ˌæmɪˈtrɪptɪliːn/[1] |
| Trade names | Elavil, others |
| Other names | Amitryptyline; Amytriptyline; Amitryptiline; Amitriptiline; MK-230; N-750; Ro 4-1575 |
IUPAC name
| |
| Clinical data | |
| Drug class | Tricyclic antidepressant (TCA) |
| Main uses | Major depression, neuropathic pain[2] |
| Side effects | Sleepiness, low blood pressure on standing, dry mouth, mental confusion[2] |
| Pregnancy category |
|
| Routes of use | By mouth, intramuscular injection |
| Defined daily dose | 75 mg[3] |
| External links | |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a682388 |
| Legal | |
| License data |
|
| Legal status | |
| Pharmacokinetics | |
| Bioavailability | 30–60% |
| Protein binding | 96%[4] |
| Metabolism | Liver[4] (CYP2D6, CYP2C19) |
| Metabolites | nortriptyline |
| Elimination half-life | 10–50 hours[4] |
| Excretion | Urine[4] |
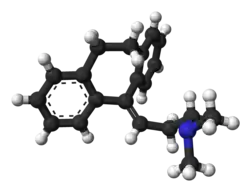
| Chemical and physical data | |
| Formula | C20H23N |
| Molar mass | 277.411 g·mol−1 |
| 3D model (JSmol) | |
| Melting point | 188 °C (370 °F) |
SMILES
| |
InChI
| |
Amitriptyline, sold under the brand name Elavil among others, is a medicine primarily used to treat a number of mental illnesses.[4] These include major depressive disorder and anxiety disorders, and less commonly attention deficit hyperactivity disorder (ADHD) and bipolar disorder.[4][5] Other uses include prevention of migraines, treatment of neuropathic pain such as fibromyalgia and postherpetic neuralgia, and less commonly insomnia.[4][6] It is in the tricyclic antidepressant (TCA) class and its exact mechanism of action is unclear.[4] Amitriptyline is taken by mouth.[4]
Common side effects include blurred vision, dry mouth, low blood pressure on standing, sleepiness, and constipation.[4] Serious side effects may include seizures, an increased risk of suicide in those less than 25 years of age, urinary retention, glaucoma, and a number of heart issues.[4] It should not be taken with MAO inhibitors or the medication cisapride.[4] Amitriptyline may cause problems if taken during pregnancy.[4][7] Use during breastfeeding appears to be relatively safe.[8]
Amitriptyline was discovered in 1960[9] and approved by the US Food and Drug Administration (FDA) in 1961.[10] It is on the World Health Organization's List of Essential Medicines.[11] It is available as a generic medication.[4] The wholesale cost in the developing world as of 2014 was between 0.01 and US$0.04 per dose.[12] In the United States, it costs about US$0.20 per dose.[4] In 2017, it was the 87th most commonly prescribed medication in the United States, with more than nine million prescriptions.[13][14]
Medical uses
Amitriptyline is used for a number of medical conditions including major depressive disorder (MDD).[15][16][17] Some evidence suggests amitriptyline may be more effective than other antidepressants,[18][19] including selective serotonin reuptake inhibitors (SSRIs),[20] although it is rarely used as a first-line antidepressant due to its higher toxicity in overdose and generally poorer tolerability,[16] so is used as a second-line treatment when SSRIs do not work.[21] It is used in addition to other medications for pain.[22] A 2001 review called it "the gold-standard antidepressant".[18]
It is TGA-labeled in Australia for migraine prevention, also in cases of neuropathic pain disorders,[16] fibromyalgia[6] and nocturnal enuresis.[16][23] Amitriptyline is a popular off-label treatment for irritable bowel syndrome (IBS),[24] although it is most frequently reserved for severe cases of abdominal pain in patients with IBS because it needs to be taken regularly to work and has a generally poor tolerability profile, although a firm evidence base supports its efficacy in this indication.[24] Amitriptyline can also be used as an anticholinergic drug in the treatment of early-stage Parkinson's disease if depression also needs to be treated.[25] Amitriptyline is the most widely researched agent for prevention of frequent tension headaches.[26]
Dosage
The defined daily dose is 75 mg by mouth or injection.[3] The initial dose for depression and neuropathic pain in adults is 25 mg at night which may be increased up to 75 mg at night.[2] A lower dose should be used in older people.[2]
For depression treatment is recommended for at least nine months and should be stopped slowly.[2] For neuropathic pain treatment is recommended until three to six month after symptoms have resolved.[2]
Contraindications
The known contraindications of amitriptyline are:[27]
- Hypersensitivity to TCAs or to any of its excipients
- History of myocardial infarction
- History of arrhythmias, particularly heart block to any degree
- Congestive heart failure
- Coronary artery insufficiency
- Mania
- Severe liver disease
- Being under seven years of age
- Breast feeding
- Patients who are taking monoamine oxidase inhibitors (MAOIs) or have taken them within the last 14 days.
Side effects
Common side effects, occurring in more than 1% of users, include dizziness, headache, and weight gain. Side effects common to anticholinergics occur more often than with other TCAs such as imipramine. Cognitive side effects include delirium and confusion, as well as mood disturbances such as anxiety and agitation. Cardiovascular side effects may include orthostatic hypotension, sinus tachycardia, and QT-interval prolongation.[28] Sexual side effects include loss of libido and impotence, while sleep disturbances may include drowsiness, insomnia, and nightmares.[15][16][17][27][29][30] Of the TCAs, amitriptyline is said to have the most anticholinergic side effects and to be the most likely to produce delirium.[31]
Overdose
The symptoms and the treatment of an overdose are largely the same as for the other TCAs, including the presentation of serotonin syndrome and adverse cardiac effects. The British National Formulary notes that amitriptyline can be particularly dangerous in overdose,[17] thus it and other TCAs are no longer recommended as first-line therapy for depression. Alternative agents, SSRIs and SNRIs, are safer in overdose, though they are no more efficacious than TCAs. English folk singer Nick Drake died from an overdose of Tryptizol in 1974.[32]
The possible symptoms of amitriptyline overdose include:[30]
- Drowsiness
- Hypothermia (low body temperature)
- Tachycardia (high heart rate)
- Other arrhythmic abnormalities, such as bundle branch block
- ECG evidence of impaired conduction
- Congestive heart failure
- Dilated pupils
- Convulsions (e.g. seizures, myoclonus)
- Severe hypotension (very low blood pressure)
- Stupor
- Coma
- Death
- Polyradiculoneuropathy
- Changes in the electrocardiogram, particularly QT-interval prolongation[28] and change in QRS axis or width
- Agitation
- Hyperactive reflexes
- Muscle rigidity
- Vomiting
The treatment of overdose is mostly supportive as no specific antidote for amitriptyline overdose is available.[30] Activated charcoal may reduce absorption if given within 1–2 hours of ingestion.[30] If the affected person is unconscious or has an impaired gag reflex, a nasogastric tube may be used to deliver the activated charcoal into the stomach.[30] ECG monitoring for cardiac conduction abnormalities is essential and if one is found close monitoring of cardiac function is advised.[30] Body temperature should be regulated with measures such as heating blankets if necessary.[30] Cardiac monitoring is advised for at least five days after the overdose.[30] Benzodiazepines are recommended for control of seizures.[30] Dialysis is of no use due to the high degree of protein binding with amitriptyline.[30]
Interactions
Amitriptyline is known to interact with:[30]
- Monoamine oxidase inhibitors as it can potentially induce a serotonin syndrome
- CYP2D6 inhibitors and substrates such as fluoxetine due to the potential for an increase in plasma concentrations of the drug to be seen
- Guanethidine as it can reduce the antihypertensive effects of this drug
- Anticholinergic agents such as benztropine, hyoscine (scopolamine) and atropine, because the two might exacerbate each other's anticholinergic effects, including paralytic ileus and tachycardia
- Antipsychotics due to the potential for them to exacerbate the sedative, anticholinergic, epileptogenic and pyrexic (fever-promoting) effects. Also increases the risk of neuroleptic malignant syndrome
- Cimetidine due to the potential for it to interfere with hepatic metabolism of amitriptyline and hence increasing steady-state concentrations of the drug
- Disulfiram due to the potential for the development of delirium
- ECT may increase the risks associated with this treatment
- Antithyroid medications may increase the risk of agranulocytosis
- Thyroid hormones have a potential for increased adverse effects such as CNS stimulation and arrhythmias.
- Analgesics, such as tramadol and pethidine due to the potential for an increase in seizure risk and serotonin syndrome.
- Medications subject to gastric inactivation (e.g. levodopa) due to the potential for amitriptyline to delay gastric emptying and reduce intestinal motility
- Medications subject to increased absorption given more time in the small intestine (e.g. anticoagulants)
- Serotonergic agents such as the SSRIs and triptans due to the potential for serotonin syndrome.
Pharmacology
Pharmacodynamics
| Site | AMI | NTI | Species | Ref |
|---|---|---|---|---|
| SERT | 2.8–4.3 | 15–18 | Human | [34][35] |
| NET | 19–35 | 1.8–4.4 | Human | [34][35] |
| DAT | 3,250 | 1,140 | Human | [34] |
| 5-HT1A | 450–1,800 | 294 | Human | [36][37] |
| 5-HT1B | 840 | ND | Rat | [38] |
| 5-HT2A | 18–23 | 5.0–41 | Human/rat | [36][37] |
| 5-HT2B | 174 13.4 (KB) | ND | Human | [39] |
| 5-HT2C | 4.0 | 8.5 | Human/rat | [40][41] |
| 5-HT3 | 430 | 1,400 | Rat | [42] |
| 5-HT6 | 65–141 | 148 | Human/rat | [43][44][45] |
| 5-HT7 | 92.8–123 | ND | Rat | [46] |
| α1 | 4.4–24 | 55 | Human | [35][36] |
| α2 | 114–690 | 2,030 | Human | [35][36] |
| β | >10,000 | >10,000 | Rat | [47][48] |
| D1 | 89 | ND | Human | [49] |
| D2 | 196–1,460 | 2,570 | Human | [36][49] |
| D3 | 206 | ND | Human | [49] |
| D4 | ND | ND | ND | ND |
| D5 | 170 | ND | Human | [49] |
| H1 | 0.5–1.1 | 3.0–15 | Human | [49][50][51] |
| H2 | 66 | 646 | Human | [50] |
| H3 | 75,900 | 45,700 | Human | [49][50] |
| H4 | 26,300 | 6,920 | Human | [50][52] |
| mACh | 9.6 | 37 | Human | [36] |
| M1 | 11.0–14.7 | 40 | Human | [53][54] |
| M2 | 11.8 | 110 | Human | [53] |
| M3 | 12.8–39 | 50 | Human | [53][54] |
| M4 | 7.2 | 84 | Human | [53] |
| M5 | 15.7–24 | 97 | Human | [53][54] |
| σ1 | 300 | 2,000 | Guinea pig | [55] |
| σ2 | ND | ND | ND | ND |
| hERG | >3,000 | ND | Human | [56] |
| Values are Ki (nM), unless otherwise noted. The smaller the value, the more strongly the drug binds to the site. | ||||
Amitriptyline is classified as a tricyclic antidepressant (TCA), with strong actions on the serotonin transporter (SERT) and moderate effects on the norepinephrine transporter (NET).[34][57] It has negligible influence on the dopamine transporter (DAT) and therefore does not affect dopamine reuptake, being nearly 1,000 times weaker on inhibition of the reuptake of this neurotransmitter than on serotonin.[34] It is metabolized to nortriptyline, a more potent and selective norepinephrine reuptake inhibitor, and this may serve to complement its effects on norepinephrine reuptake.[30]
Amitriptyline additionally acts as an antagonist or inverse agonist of the serotonin 5-HT2A, 5-HT2C, 5-HT3, 5-HT6, and 5-HT7 receptors, the α1-adrenergic receptor, the histamine H1 and H2 receptors,[58] and the muscarinic acetylcholine receptors, and as an agonist of the sigma σ1 receptor.[35][59][60][61] It has also been shown to be a relatively weak NMDA receptor antagonist via the dizocilpine (MK-801)/phencyclidine (PCP) site.[62] Amitriptyline inhibits sodium channels, L-type calcium channels, and Kv1.1, Kv7.2, and Kv7.3 voltage-gated potassium channels, and therefore acts as a sodium, calcium, and potassium channel blocker as well.[63][64]
Amitriptyline has been demonstrated to act as an agonist of the TrkA and TrkB receptors.[65] It promotes the heterodimerization of these proteins in the absence of NGF and has potent neurotrophic activity both in-vivo and in-vitro in mouse models.[65][66] These are the same receptors BDNF activates, an endogenous neurotrophin with powerful antidepressant effects, and as such this property may contribute significantly to its therapeutic efficacy against depression. Amitriptyline also acts as a functional inhibitor of acid sphingomyelinase,[67] and as a PARP1 inhibitor.[68]
Mechanism of action
Amitriptyline inhibits neuronal reuptake of serotonin and noradrenaline from the synapse in the central nervous system; this increases their availability in the synapse to cause neurotransmission on the post-synaptic neurone.[69] Amitriptyline is metabolised by cytochrome P450 enzymes in the liver to nortriptyline, which also acts as a noradrenaline reuptake inhibitor; this potentiates the antidepressant effects of amitriptyline.[70]
Pharmacokinetics
Amitriptyline is a highly lipophilic molecule having an octanol-water partition coefficient (pH 7.4) of 3.0,[71] while the log P of the free base was reported as 4.92.[72] Solubility in water is 9.71 mg/litre at 24 °C.[73]
Amitriptyline is readily absorbed from the gastrointestinal tract and is extensively metabolized on first pass through the liver.[30] It is metabolized mostly by CYP2D6, CYP3A4, and CYP2C19-mediated N-demethylation into nortriptyline,[30] which is another TCA in its own right.[74] It is 96% bound to plasma proteins; nortriptyline is 93–95% bound to plasma proteins.[30][75] It is mostly excreted in the urine (around 30–50%) as metabolites either free or as glucuronide and sulfate conjugates within 24 hours.[30] 2% of the unchanged drug is excreted in the urine.[69] Small amounts are also excreted in feces.[29] Amitriptyline has an elimination half life of 25 hours an its volume of distribution is 10–50L/kg.[70]
Therapeutic levels of amitriptyline range from 75 to 175 ng/mL (270–631 nM),[76] or 80–250 ng/mL of both amitriptyline and its metabolite nortriptyline.[77]
Pharmacogenetics
Since amitriptyline is primarily metabolized by CYP2D6 and CYP2C19, genetic variations within the genes coding for these enzymes can affect its metabolism, leading to changes in the concentrations of the drug in the body.[78] Increased concentrations of amitriptyline may increase the risk for side effects, including anticholinergic and nervous system adverse effects, while decreased concentrations may reduce the drug's efficacy.[79][80][81][82]
Individuals can be categorized into different types of CYP2D6 or CYP2C19 metabolizers depending on which genetic variations they carry. These metabolizer types include poor, intermediate, extensive, and ultrarapid metabolizers. Most individuals (about 77–92%) are extensive metabolizers,[81] and have "normal" metabolism of amitriptyline. Poor and intermediate metabolizers have reduced metabolism of the drug as compared to extensive metabolizers; patients with these metabolizer types may have an increased probability of experiencing side effects. Ultrarapid metabolizers use amitriptyline much faster than extensive metabolizers; patients with this metabolizer type may have a greater chance of experiencing pharmacological failure.[79][80][81][82]
The Clinical Pharmacogenetics Implementation Consortium recommends avoiding amitriptyline in patients who are CYP2D6 ultrarapid or poor metabolizers, due to the risk for a lack of efficacy and side effects, respectively. The consortium also recommends considering an alternative drug not metabolized by CYP2C19 in patients who are CYP2C19 ultrarapid metabolizers. A reduction in starting dose is recommended for patients who are CYP2D6 intermediate metabolizers and CYP2C19 poor metabolizers. If use of amitriptyline is warranted, therapeutic drug monitoring is recommended to guide dose adjustments.[81] The Dutch Pharmacogenetics Working Group also recommends selecting an alternative drug or monitoring plasma concentrations of amitriptyline in patients who are CYP2D6 poor or ultrarapid metabolizers, and selecting an alternative drug or reducing initial dose in patients who are CYP2D6 intermediate metabolizers.[83]
Chemistry
Amitriptyline is a tricyclic compound, specifically a dibenzocycloheptadiene, and possesses three rings fused together with a side chain attached in its chemical structure.[84] Other dibenzocycloheptadiene TCAs include nortriptyline (noramitriptyline, N-desmethylamitriptyline), protriptyline, and butriptyline.[84] Amitriptyline is a tertiary amine TCA, with its side chain-demethylated metabolite nortriptyline being a secondary amine.[85][86] Other tertiary amine TCAs include imipramine, clomipramine, dosulepin (dothiepin), doxepin, and trimipramine.[87][88] The chemical name of amitriptyline is 3-(10,11-dihydro-5H-dibenzo[a,d]cycloheptene-5-ylidene)-N,N-dimethylpropan-1-amine and its free base form has a chemical formula of C20H23N with a molecular weight of 277.403 g/mol.[89] The drug is used commercially mostly as the hydrochloride salt; the free base form is used rarely and the embonate (pamoate) salt is used for intramuscular administration.[89][90] The CAS Registry Number of the free base is 50-48-6, of the hydrochloride is 549-18-8, and of the embonate is 17086-03-2.[89][90]
History
Amitriptyline was first synthesized in 1960 and was introduced for medical use in United States in 1961 and in the United Kingdom in 1962, in both countries under the brand name Elavil.[91][92][93][94] It was the second TCA to be introduced, following the introduction of imipramine in 1957.[92][93]
Society and culture

Cost
The wholesale cost in the developing world as of 2014 was between 0.01 and US$0.04 per dose.[12] In the United States, it costs about US$0.20 per dose.[4] In 2017, it was the 87th most commonly prescribed medication in the United States, with more than nine million prescriptions.[13][14]
.svg.png.webp) Amitriptyline costs (USA)
Amitriptyline costs (USA).svg.png.webp) Amitriptyline prescriptions (USA)
Amitriptyline prescriptions (USA)
Generic names
Amitriptyline is the English and French generic name of the drug and its INN, BAN, and DCF, while amitriptyline hydrochloride is its USAN, USP, BANM, and JAN.[89][90][95][96] Its generic name in Spanish and Italian and its DCIT are amitriptilina, in German is Amitriptylin, and in Latin is amitriptylinum.[90][96] The embonate salt is known as amitriptyline embonate, which is its BANM, or as amitriptyline pamoate unofficially.[90]
Brand names
As of September 2018, amitriptyline was marketed under many brand names worldwide alone and as a combination drug with each of chlordiazepoxide, perphenazine, and medazepam.[97]
Brands include Adepril, ADT, Ambival, Amicon, Amilavil, Amilin, Amiline, Amineurin, Amiplin, Amirol, Amit, Amitin, Amitone, Amitrac, Amitrip, Amitriptilina, Amitriptilino, Amitriptilins, Amitriptine, Amitriptylin, Amitriptyline, Amitriptylinhydrochlorid, Amitriptylini, Amitriptylinum, Amitryp, Amotrip, Amyline, Amypres, Amytril, Amyzol, Anapsique, Arpidox, Deprelio, Elatrol, Elatrolet, Elavil, Endep, Fiorda, Laroxyl, Latilin, Levate, Maxitrip, Maxivalet, Mitryp, Modup, Normaln, Odep, Pinsaun, Polytanol, Protanol, Qualitriptine, Redomex, Saroten, Sarotex, Stelminal, Syneudon, Teperin, Trepiline, Triamyl, Trilin, Trip, Tripta, Triptiline, Triptizol, Triptric, Triptyl, Triptyline, Tripyline, Trynol, Tryptalgin, Tryptanol, Tryptin, Tryptizol, Tryptomer, and Vanatrip.[97]
Brands as of that date for the combination with chlordiazepoxide included Amicon Forte, Amitrac-CZ, Amypres-C, Antalin, Antalin Forte, Arpidox-CP, Axeptyl, Diapatol, Diaztric-A, Emotrip, Klotriptyl, Libotryp, Limbatril, Limbitrol, Limbitryl, Limbival, Limbritol, Maxitrip-CZ, Mitryp Forte, Morelin, Ristryl, and Sedans.[97]
Brands as of that date for the combination with perphenazine included Levazine, Minitran, Mutabase, Mutabon, Pertriptyl, Triavil, and Triptafen.[97]
Brands as of that date for the combination with medazepam included Nobritol.[97]
Research
Amitriptyline has been studied in several disorders:
- Eating disorders:[29] The few randomized controlled trials investigating its efficacy in eating disorders have been discouraging.[98]
- Insomnia: As of 2004, amitriptyline was the most commonly prescribed off-label prescription sleep aid in the United States.[99] Owing to the development of tolerance and the potential for adverse effects such as constipation, its use in the elderly for this indication is recommended against.[16]
- Urinary incontinence. An accepted use for amitriptyline in Australia is the treatment of urinary urge incontinence.[16]
- Cyclic vomiting syndrome[100][101]
- Preventive treatment for patients with recurring biliary dyskinesia (sphincter of Oddi dysfunction)[102]
- Attention deficit/hyperactivity disorder (in addition to, or sometimes in place of ADHD stimulant drugs)[103]
- Retching/dry heaving, especially after the anti-reflux procedure Nissen fundoplication[104]
References
- ↑ Oxford Dictionary: Definition of amitriptyline (British & World English) Archived 14 July 2014 at the Wayback Machine
- 1 2 3 4 5 6 "AMITRIPTYLINE oral - Essential drugs". medicalguidelines.msf.org. Archived from the original on 27 August 2021. Retrieved 25 August 2020.
- 1 2 "WHOCC - ATC/DDD Index". www.whocc.no. Archived from the original on 21 October 2020. Retrieved 22 September 2020.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 "Amitriptyline Hydrochloride". The American Society of Health-System Pharmacists. Archived from the original on 24 September 2014. Retrieved 25 September 2014.
- ↑ Leucht C, Huhn M, Leucht S (December 2012). "Amitriptyline versus placebo for major depressive disorder". The Cochrane Database of Systematic Reviews. 12: CD009138. doi:10.1002/14651858.CD009138.pub2. PMID 23235671.
- 1 2 Moore RA, Derry S, Aldington D, Cole P, Wiffen PJ (July 2015). "Amitriptyline for neuropathic pain in adults". The Cochrane Database of Systematic Reviews. 7 (7): CD008242. doi:10.1002/14651858.CD008242.pub3. PMC 6447238. PMID 26146793.
- ↑ "Prescribing medicines in pregnancy database". Australian Government. 3 March 2014. Archived from the original on 8 April 2014. Retrieved 22 April 2014.
- ↑ "Amitriptyline Levels and Effects while Breastfeeding". drugs.com. 8 September 2014. Archived from the original on 24 September 2014. Retrieved 25 September 2014.
- ↑ Sneader, Walter (2005). Drug Discovery a History. Chichester: John Wiley & Sons. p. 414. ISBN 9780470015520. Archived from the original on 8 September 2017.
- ↑ Fangmann P, Assion HJ, Juckel G, González CA, López-Muñoz F (February 2008). "Half a century of antidepressant drugs: on the clinical introduction of monoamine oxidase inhibitors, tricyclics, and tetracyclics. Part II: tricyclics and tetracyclics". Journal of Clinical Psychopharmacology. 28 (1): 1–4. doi:10.1097/jcp.0b013e3181627b60. PMID 18204333. S2CID 31018835.
- ↑ World Health Organization (2019). World Health Organization model list of essential medicines: 21st list 2019. Geneva: World Health Organization. hdl:10665/325771. WHO/MVP/EMP/IAU/2019.06. License: CC BY-NC-SA 3.0 IGO.
- 1 2 "Amitriptyline". International Drug Price Indicator Guide. Archived from the original on 30 March 2017. Retrieved 2 December 2015.
- 1 2 "The Top 300 of 2020". ClinCalc. Archived from the original on 18 March 2020. Retrieved 11 April 2020.
- 1 2 "Amitriptyline - Drug Usage Statistics". ClinCalc. Archived from the original on 30 April 2017. Retrieved 11 April 2020.
- 1 2 "AMITRIPTYLINE HYDROCHLORIDE tablet, film coated [Dispensing Solutions, Inc.]". DailyMed. Dispensing Solutions, Inc. September 2013. Archived from the original on 3 December 2013. Retrieved 1 December 2013.
- 1 2 3 4 5 6 7 Rossi, S, ed. (2013). Australian Medicines Handbook (2013 ed.). Adelaide: The Australian Medicines Handbook Unit Trust. ISBN 978-0-9805790-9-3.
- 1 2 3 Joint Formulary Committee (2013). British National Formulary (BNF) (65th ed.). London, UK: Pharmaceutical Press. ISBN 978-0-85711-084-8.
- 1 2 Barbui C, Hotopf M (February 2001). "Amitriptyline v. the rest: still the leading antidepressant after 40 years of randomised controlled trials". The British Journal of Psychiatry. 178 (2): 129–44. doi:10.1192/bjp.178.2.129. PMID 11157426.
- ↑ Cipriani A, Furukawa TA, Salanti G, Chaimani A, Atkinson LZ, Ogawa Y, et al. (April 2018). "Comparative efficacy and acceptability of 21 antidepressant drugs for the acute treatment of adults with major depressive disorder: a systematic review and network meta-analysis". Lancet. 391 (10128): 1357–1366. doi:10.1016/S0140-6736(17)32802-7. PMC 5889788. PMID 29477251.
- ↑ Anderson IM (April 2000). "Selective serotonin reuptake inhibitors versus tricyclic antidepressants: a meta-analysis of efficacy and tolerability". Journal of Affective Disorders. 58 (1): 19–36. doi:10.1016/S0165-0327(99)00092-0. PMID 10760555.
- ↑ Hitchings, Andrew; Lonsdale, Dagan; Burrage, Daniel; Baker, Emma (2015). Top 100 drugs : clinical pharmacology and practical prescribing. p. 50. ISBN 978-0-7020-5516-4.
- ↑ Bryson HM, Wilde MI (June 1996). "Amitriptyline. A review of its pharmacological properties and therapeutic use in chronic pain states". Drugs & Aging. 8 (6): 459–76. doi:10.2165/00002512-199608060-00008. PMID 8736630.
- ↑ Kennea NL, Evans JH (June 2000). "Drug Treatment of Nocturnal Enuresis" (PDF). Paediatric and Perinatal Drug Therapy. 4 (1): 12–18. doi:10.1185/1463009001527679. Archived from the original (PDF) on 3 December 2013.
- 1 2 Viera AJ, Hoag S, Shaughnessy J (November 2002). "Management of irritable bowel syndrome" (PDF). American Family Physician. 66 (10): 1867–74. PMID 12469960. Archived (PDF) from the original on 3 December 2013.
- ↑ Parkinson's disease Archived 18 November 2013 at the Wayback Machine. Merck Sharp & Dohme Corp. August 2007. Retrieved 22 December 2013.
- ↑ Millea PJ, Brodie JJ (September 2002). "Tension-type headache". American Family Physician. 66 (5): 797–804. PMID 12322770. Archived from the original on 1 July 2015.
- 1 2 "Amitriptyline Tablets BP 50mg – Summary of Product Characteristics (SPC)". electronic Medicines Compendium. Actavis UK Ltd. 24 March 2013. Archived from the original on 3 December 2013. Retrieved 1 December 2013.
- 1 2 Zemrak WR, Kenna GA (June 2008). "Association of antipsychotic and antidepressant drugs with Q-T interval prolongation". American Journal of Health-System Pharmacy. 65 (11): 1029–38. doi:10.2146/ajhp070279. PMID 18499875. Archived from the original on 21 December 2016.
- 1 2 3 "Levate (amitriptyline), dosing, indications, interactions, adverse effects, and more". Medscape Reference. WebMD. Archived from the original on 3 December 2013. Retrieved 1 December 2013.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 "Endep Amitriptyline hydrochloride" (PDF). TGA eBusiness Services. Alphapharm Pty Limited. 10 December 2012. Archived from the original on 13 August 2017. Retrieved 1 December 2013.
- ↑ Schatzberg, Alan F.; Nemeroff, Charles B. (2009). The American Psychiatric Publishing Textbook of Psychopharmacology. American Psychiatric Pub. pp. 271–. ISBN 978-1-58562-309-9. Archived from the original on 8 September 2017.
- ↑ Brown, M., "Nick Drake: the fragile genius" Archived 11 March 2018 at the Wayback Machine, The Daily Telegraph, 25 November 2014.
- ↑ Roth BL, Driscol J. "PDSP Ki Database". Psychoactive Drug Screening Program (PDSP). University of North Carolina at Chapel Hill and the United States National Institute of Mental Health. Archived from the original on 27 August 2021. Retrieved 14 August 2017.
- 1 2 3 4 5 Tatsumi M, Groshan K, Blakely RD, Richelson E (1997). "Pharmacological profile of antidepressants and related compounds at human monoamine transporters". Eur. J. Pharmacol. 340 (2–3): 249–58. doi:10.1016/s0014-2999(97)01393-9. PMID 9537821.
- 1 2 3 4 5 Owens MJ, Morgan WN, Plott SJ, Nemeroff CB (1997). "Neurotransmitter receptor and transporter binding profile of antidepressants and their metabolites". J. Pharmacol. Exp. Ther. 283 (3): 1305–22. PMID 9400006.
- 1 2 3 4 5 6 Cusack B, Nelson A, Richelson E (1994). "Binding of antidepressants to human brain receptors: focus on newer generation compounds". Psychopharmacology. 114 (4): 559–65. doi:10.1007/bf02244985. PMID 7855217.
- 1 2 Peroutka SJ (1988). "Antimigraine drug interactions with serotonin receptor subtypes in human brain". Ann. Neurol. 23 (5): 500–4. doi:10.1002/ana.410230512. PMID 2898916.
- ↑ Peroutka SJ (1986). "Pharmacological differentiation and characterization of 5-HT1A, 5-HT1B, and 5-HT1C binding sites in rat frontal cortex". J. Neurochem. 47 (2): 529–40. doi:10.1111/j.1471-4159.1986.tb04532.x. PMID 2942638.
- ↑ Schmuck K, Ullmer C, Kalkman HO, Probst A, Lubbert H (1996). "Activation of meningeal 5-HT2B receptors: an early step in the generation of migraine headache?". Eur. J. Neurosci. 8 (5): 959–67. doi:10.1111/j.1460-9568.1996.tb01583.x. PMID 8743744.
- ↑ Roth BL, Kroeze WK (2006). "Screening the receptorome yields validated molecular targets for drug discovery". Curr. Pharm. Des. 12 (14): 1785–95. doi:10.2174/138161206776873680. PMID 16712488.
- ↑ Pälvimäki EP, Roth BL, Majasuo H, Laakso A, Kuoppamäki M, Syvälahti E, Hietala J (1996). "Interactions of selective serotonin reuptake inhibitors with the serotonin 5-HT2c receptor". Psychopharmacology. 126 (3): 234–40. doi:10.1007/bf02246453. PMID 8876023.
- ↑ Schmidt AW, Hurt SD, Peroutka SJ (1989). "'[3H]quipazine' degradation products label 5-HT uptake sites". Eur. J. Pharmacol. 171 (1): 141–3. doi:10.1016/0014-2999(89)90439-1. PMID 2533080.
- ↑ Kohen R, Metcalf MA, Khan N, Druck T, Huebner K, Lachowicz JE, Meltzer HY, Sibley DR, Roth BL, Hamblin MW (1996). "Cloning, characterization, and chromosomal localization of a human 5-HT6 serotonin receptor". J. Neurochem. 66 (1): 47–56. doi:10.1046/j.1471-4159.1996.66010047.x. PMID 8522988.
- ↑ Hirst WD, Abrahamsen B, Blaney FE, Calver AR, Aloj L, Price GW, Medhurst AD (2003). "Differences in the central nervous system distribution and pharmacology of the mouse 5-hydroxytryptamine-6 receptor compared with rat and human receptors investigated by radioligand binding, site-directed mutagenesis, and molecular modeling". Mol. Pharmacol. 64 (6): 1295–308. doi:10.1124/mol.64.6.1295. PMID 14645659. S2CID 33743899.
- ↑ Monsma FJ, Shen Y, Ward RP, Hamblin MW, Sibley DR (1993). "Cloning and expression of a novel serotonin receptor with high affinity for tricyclic psychotropic drugs". Mol. Pharmacol. 43 (3): 320–7. PMID 7680751.
- ↑ Shen Y, Monsma FJ, Metcalf MA, Jose PA, Hamblin MW, Sibley DR (1993). "Molecular cloning and expression of a 5-hydroxytryptamine7 serotonin receptor subtype". J. Biol. Chem. 268 (24): 18200–4. PMID 8394362.
- ↑ Bylund DB, Snyder SH (1976). "Beta adrenergic receptor binding in membrane preparations from mammalian brain". Mol. Pharmacol. 12 (4): 568–80. PMID 8699.
- ↑ Sánchez C, Hyttel J (1999). "Comparison of the effects of antidepressants and their metabolites on reuptake of biogenic amines and on receptor binding". Cell. Mol. Neurobiol. 19 (4): 467–89. doi:10.1023/A:1006986824213. PMID 10379421. S2CID 19490821.
- 1 2 3 4 5 6 von Coburg Y, Kottke T, Weizel L, Ligneau X, Stark H (2009). "Potential utility of histamine H3 receptor antagonist pharmacophore in antipsychotics". Bioorg. Med. Chem. Lett. 19 (2): 538–42. doi:10.1016/j.bmcl.2008.09.012. PMID 19091563.
- 1 2 3 4 Appl H, Holzammer T, Dove S, Haen E, Strasser A, Seifert R (2012). "Interactions of recombinant human histamine H₁R, H₂R, H₃R, and H₄R receptors with 34 antidepressants and antipsychotics". Naunyn Schmiedebergs Arch. Pharmacol. 385 (2): 145–70. doi:10.1007/s00210-011-0704-0. PMID 22033803. S2CID 14274150.
- ↑ Ghoneim OM, Legere JA, Golbraikh A, Tropsha A, Booth RG (2006). "Novel ligands for the human histamine H1 receptor: synthesis, pharmacology, and comparative molecular field analysis studies of 2-dimethylamino-5-(6)-phenyl-1,2,3,4-tetrahydronaphthalenes". Bioorg. Med. Chem. 14 (19): 6640–58. doi:10.1016/j.bmc.2006.05.077. PMID 16782354.
- ↑ Nguyen T, Shapiro DA, George SR, Setola V, Lee DK, Cheng R, Rauser L, Lee SP, Lynch KR, Roth BL, O'Dowd BF (2001). "Discovery of a novel member of the histamine receptor family". Mol. Pharmacol. 59 (3): 427–33. doi:10.1124/mol.59.3.427. PMID 11179435. Archived from the original on 27 August 2021. Retrieved 11 December 2019.
- 1 2 3 4 5 Stanton T, Bolden-Watson C, Cusack B, Richelson E (1993). "Antagonism of the five cloned human muscarinic cholinergic receptors expressed in CHO-K1 cells by antidepressants and antihistaminics". Biochem. Pharmacol. 45 (11): 2352–4. doi:10.1016/0006-2952(93)90211-e. PMID 8100134.
- 1 2 3 Bymaster FP, Nelson DL, DeLapp NW, Falcone JF, Eckols K, Truex LL, Foreman MM, Lucaites VL, Calligaro DO (1999). "Antagonism by olanzapine of dopamine D1, serotonin2, muscarinic, histamine H1 and alpha 1-adrenergic receptors in vitro". Schizophr. Res. 37 (1): 107–22. doi:10.1016/s0920-9964(98)00146-7. PMID 10227113.
- ↑ Weber E, Sonders M, Quarum M, McLean S, Pou S, Keana JF (1986). "1,3-Di(2-[5-3H]tolyl)guanidine: a selective ligand that labels sigma-type receptors for psychotomimetic opiates and antipsychotic drugs". Proc. Natl. Acad. Sci. U.S.A. 83 (22): 8784–8. Bibcode:1986PNAS...83.8784W. doi:10.1073/pnas.83.22.8784. PMC 387016. PMID 2877462.
- ↑ Teschemacher AG, Seward EP, Hancox JC, Witchel HJ (1999). "Inhibition of the current of heterologously expressed HERG potassium channels by imipramine and amitriptyline". Br. J. Pharmacol. 128 (2): 479–85. doi:10.1038/sj.bjp.0702800. PMC 1571643. PMID 10510461.
- ↑ "Potency of antidepressants to block noradrenaline reuptake". CNS Forum. Archived from the original on 8 November 2012. Retrieved 16 February 2013.
- ↑ Ellis, Albert; Ellis, Gwynn Pennant (1 January 1987). Progress in Medicinal Chemistry. Elsevier. p. 56. ISBN 978-0-444-80876-9. Archived from the original on 13 June 2013. Retrieved 27 November 2011.
- ↑ Schatzberg, Alan F; Nemeroff, Charles B (2006). Essentials of clinical psychopharmacology. American Psychiatric Pub. p. 7. ISBN 978-1-58562-243-6.
- ↑ Rauser L, Savage JE, Meltzer HY, Roth BL (October 2001). "Inverse agonist actions of typical and atypical antipsychotic drugs at the human 5-hydroxytryptamine(2C) receptor". J. Pharmacol. Exp. Ther. 299 (1): 83–9. PMID 11561066.
- ↑ Werling LL, Keller A, Frank JG, Nuwayhid SJ (October 2007). "A comparison of the binding profiles of dextromethorphan, memantine, fluoxetine and amitriptyline: treatment of involuntary emotional expression disorder". Exp. Neurol. 207 (2): 248–57. doi:10.1016/j.expneurol.2007.06.013. PMID 17689532. S2CID 38476281.
- ↑ Sills MA, Loo PS (July 1989). "Tricyclic antidepressants and dextromethorphan bind with higher affinity to the phencyclidine receptor in the absence of magnesium and L-glutamate". Mol. Pharmacol. 36 (1): 160–5. PMID 2568580.
- ↑ Pancrazio JJ, Kamatchi GL, Roscoe AK, Lynch C (January 1998). "Inhibition of neuronal Na+ channels by antidepressant drugs". J. Pharmacol. Exp. Ther. 284 (1): 208–14. PMID 9435180.
- ↑ Punke MA, Friederich P (May 2007). "Amitriptyline is a potent blocker of human Kv1.1 and Kv7.2/7.3 channels". Anesthesia and Analgesia. 104 (5): 1256–1264. doi:10.1213/01.ane.0000260310.63117.a2. PMID 17456683. S2CID 21924741. Archived from the original on 27 August 2021. Retrieved 15 October 2009.
- 1 2 Jang SW, Liu X, Chan CB, Weinshenker D, Hall RA, Xiao G, Ye K (June 2009). "Amitriptyline is a TrkA and TrkB receptor agonist that promotes TrkA/TrkB heterodimerization and has potent neurotrophic activity". Chemistry & Biology. 16 (6): 644–56. doi:10.1016/j.chembiol.2009.05.010. PMC 2844702. PMID 19549602.
- ↑ "Pharmaceutical Information – AMITRIPTYLINE". RxMed. Archived from the original on 27 December 2012. Retrieved 16 February 2013.
- ↑ Kornhuber J, Muehlbacher M, Trapp S, Pechmann S, Friedl A, Reichel M, et al. (2011). Riezman H (ed.). "Identification of novel functional inhibitors of acid sphingomyelinase". PLOS ONE. 6 (8): e23852. Bibcode:2011PLoSO...623852K. doi:10.1371/journal.pone.0023852. PMC 3166082. PMID 21909365.
- ↑ Fu L, Wang S, Wang X, Wang P, Zheng Y, Yao D, et al. (December 2016). "Crystal structure-based discovery of a novel synthesized PARP1 inhibitor (OL-1) with apoptosis-inducing mechanisms in triple-negative breast cancer". Scientific Reports. 6 (1): 3. doi:10.1038/s41598-016-0007-2. PMC 5431371. PMID 28442756.
- 1 2 "Amitriptyline". drugbank.ca. Archived from the original on 30 January 2019. Retrieved 29 January 2019.
- 1 2 Gillman, PK (July 2007). "Tricyclic antidepressant pharmacology and therapeutic drug interactions updated". British Journal of Pharmacology. 151 (6): 737–48. doi:10.1038/sj.bjp.0707253. PMC 2014120. PMID 17471183.
- ↑ The Pharmaceutical Codex. 1994. Principles and practice of pharmaceutics, 12th edn. Pharmaceutical press
- ↑ Hansch C, Leo A, Hoekman D. 1995. Exploring QSAR.Hydrophobic, electronic and steric constants. Washington, DC: American Chemical Society.
- ↑ Yalkowsky SH, Dannenfelser RM; The AQUASOL dATAbASE of Aqueous Solubility. Ver 5. Tucson, AZ: Univ AZ, College of Pharmacy (1992)
- ↑ Amitriptyline. Martindale: The Complete Drug Reference. London, UK: Pharmaceutical Press. 30 January 2013. Archived from the original on 27 August 2021. Retrieved 2 December 2013.
- ↑ "Pamelor, Aventyl (nortriptyline) dosing, indications, interactions, adverse effects, and more". Medscape Reference. WebMD. Archived from the original on 3 December 2013. Retrieved 2 December 2013.
- ↑ Sadock, Benjamin J.; Sadock, Virginia A. (2008). Kaplan & Sadock's Concise Textbook of Clinical Psychiatry. Lippincott Williams & Wilkins. pp. 18–. ISBN 978-0-7817-8746-8. Archived from the original on 8 July 2017.
- ↑ Orsulak, PJ (September 1989). "Therapeutic monitoring of antidepressant drugs: guidelines updated". Therapeutic Drug Monitoring. 11 (5): 497–507. doi:10.1097/00007691-198909000-00002. PMID 2683251.
- ↑ Rudorfer MV, Potter WZ (1999). "Metabolism of tricyclic antidepressants". Cell Mol Neurobiol. 19 (3): 373–409. doi:10.1023/A:1006949816036. PMID 10319193. S2CID 7940406.
- 1 2 Stingl JC, Brockmoller J, Viviani R (2013). "Genetic variability of drug-metabolizing enzymes: the dual impact on psychiatric therapy and regulation of brain function". Mol Psychiatry. 18 (3): 273–87. doi:10.1038/mp.2012.42. PMID 22565785. S2CID 20888081.
- 1 2 Kirchheiner J, Seeringer A (2007). "Clinical implications of pharmacogenetics of cytochrome P450 drug metabolizing enzymes". Biochim Biophys Acta. 1770 (3): 489–94. doi:10.1016/j.bbagen.2006.09.019. PMID 17113714.
- 1 2 3 4 Hicks JK, Swen JJ, Thorn CF, Sangkuhl K, Kharasch ED, Ellingrod VL, Skaar TC, Muller DJ, Gaedigk A, Stingl JC (2013). "Clinical Pharmacogenetics Implementation Consortium Guideline for CYP2D6 and CYP2C19 Genotypes and Dosing of Tricyclic Antidepressants" (PDF). Clinical Pharmacology & Therapeutics. 93 (5): 402–8. doi:10.1038/clpt.2013.2. PMC 3689226. PMID 23486447. Archived from the original on 27 August 2021. Retrieved 4 November 2018.
- 1 2 Dean L (2017). "Amitriptyline Therapy and CYP2D6 and CYP2C19 Genotype". In Pratt VM, McLeod HL, Rubinstein WS, et al. (eds.). Medical Genetics Summaries. National Center for Biotechnology Information (NCBI). PMID 28520380. Bookshelf ID: NBK425165. Archived from the original on 26 October 2020. Retrieved 6 February 2020.
- ↑ Swen JJ, Nijenhuis M, de Boer A, Grandia L, Maitland-van der Zee AH, Mulder H, Rongen GA, van Schaik RH, Schalekamp T, Touw DJ, van der Weide J, Wilffert B, Deneer VH, Guchelaar HJ (2011). "Pharmacogenetics: from bench to byte—an update of guidelines". Clinical Pharmacology & Therapeutics. 89 (5): 662–73. doi:10.1038/clpt.2011.34. PMID 21412232.
- 1 2 Ritsner, Michael S (15 February 2013). Polypharmacy in Psychiatry Practice, Volume I: Multiple Medication Use Strategies. Springer Science & Business Media. pp. 270–271. ISBN 978-94-007-5805-6. Archived from the original on 8 September 2017.
- ↑ Cutler, Neal R.; Sramek, John J.; Narang, Prem K. (20 September 1994). Pharmacodynamics and Drug Development: Perspectives in Clinical Pharmacology. John Wiley & Sons. pp. 160–. ISBN 978-0-471-95052-3. Archived from the original on 3 August 2020. Retrieved 13 August 2017.
- ↑ Anzenbacher, Pavel; Zanger, Ulrich M. (23 February 2012). Metabolism of Drugs and Other Xenobiotics. John Wiley & Sons. pp. 302–. ISBN 978-3-527-64632-6. Archived from the original on 8 September 2017.
- ↑ Anthony, Patricia K. (2002). Pharmacology Secrets. Elsevier Health Sciences. pp. 39–. ISBN 978-1-56053-470-9. Archived from the original on 16 December 2019. Retrieved 16 August 2017.
- ↑ Cowen, Philip; Harrison, Paul; Burns, Tom (9 August 2012). Shorter Oxford Textbook of Psychiatry. OUP Oxford. pp. 532–. ISBN 978-0-19-162675-3. Archived from the original on 8 September 2017.
- 1 2 3 4 Elks J (14 November 2014). The Dictionary of Drugs: Chemical Data: Chemical Data, Structures and Bibliographies. Springer. pp. 889–. ISBN 978-1-4757-2085-3. Archived from the original on 8 September 2017.
- 1 2 3 4 5 Index Nominum 2000: International Drug Directory. Taylor & Francis. 2000. pp. 48–. ISBN 978-3-88763-075-1.
- ↑ Fagan, Thomas; Warden, Paul G. (1996). Historical Encyclopedia of School Psychology. Greenwood Publishing Group. pp. 307–. ISBN 978-0-313-29015-2. Archived from the original on 27 August 2021. Retrieved 15 December 2017.
- 1 2 López-Muñoz, Francisco; Srinivasan, Venkataramanujam; de Berardis, Domenico; Álamo, Cecilio; Kato, Takahiro A. (16 November 2016). Melatonin, Neuroprotective Agents and Antidepressant Therapy. Springer. pp. 374–. ISBN 978-81-322-2803-5. Archived from the original on 27 August 2021. Retrieved 15 December 2017.
- 1 2 Martin, Andres; Scahill, Lawrence; Kratochvil, Christopher (14 December 2010). Pediatric Psychopharmacology. Oxford University Press, USA. pp. 292–. ISBN 978-0-19-539821-2. Archived from the original on 27 August 2021. Retrieved 15 December 2017.
- ↑ Sittig, Marshall (22 October 2013). Pharmaceutical Manufacturing Encyclopedia (3rd ed.). William Andrew Publishing, Elsevier. pp. 281–. ISBN 978-0-8155-1856-3. Archived from the original on 27 August 2021. Retrieved 15 December 2017.
- ↑ Morton IK, Hall JM (6 December 2012). Concise Dictionary of Pharmacological Agents: Properties and Synonyms. Springer Science & Business Media. pp. 15–. ISBN 978-94-011-4439-1. Archived from the original on 15 February 2017.
- 1 2 "Amitriptyline". Archived from the original on 13 August 2017. Retrieved 13 August 2017.
- 1 2 3 4 5 "Amitriptyline International Brands". Drugs.com. Archived from the original on 13 August 2017. Retrieved 7 September 2018.
- ↑ Flament MF, Bissada H, Spettigue W (March 2012). "Evidence-based pharmacotherapy of eating disorders". International Journal of Neuropsychopharmacology. 15 (2): 189–207. doi:10.1017/S1461145711000381. PMID 21414249.
- ↑ Mendelson WB, Roth T, Cassella J, Roehrs T, Walsh JK, Woods JH, Buysse DJ, Meyer RE (February 2004). "The treatment of chronic insomnia: drug indications, chronic use and abuse liability. Summary of a 2001 New Clinical Drug Evaluation Unit meeting symposium". Sleep Med Rev. 8 (1): 7–17. doi:10.1016/s1087-0792(03)00042-x. PMID 15062207.
- ↑ Sim Y-J, Kim J-M, Kwon S, Choe B-H (2009). "Clinical experience with amitriptyline for management of children with cyclic vomiting syndrome". Korean Journal of Pediatrics. 52 (5): 538–43. doi:10.3345/kjp.2009.52.5.538.
- ↑ Boles RG, Lovett-Barr MR, Preston A, Li BU, Adams K (2010). "Treatment of cyclic vomiting syndrome with co-enzyme Q10 and amitriptyline, a retrospective study". BMC Neurol. 10: 10. doi:10.1186/1471-2377-10-10. PMC 2825193. PMID 20109231.
- ↑ Wald, Arnold (2006). "Functional biliary type pain syndrome". In Pasricha, Pankaj Jay; Willis, William D.; Gebhart, G. F. (eds.). Chronic Abdominal and Visceral Pain. London: Informa Healthcare. pp. 453–62. ISBN 978-0-8493-2897-8.
- ↑ "Amitriptyline Hydrochloride Monograph for Professionals". Archived from the original on 24 September 2014. Retrieved 25 September 2014.
- ↑ "Management of Gastroparesis | American College of Gastroenterology". Archived from the original on 18 June 2015. Retrieved 16 June 2015.
External links
- Dean L (March 2017). "Amitriptyline Therapy and CYP2D6 and CYP2C19 Genotype". In Pratt VM, McLeod HL, Rubinstein WS, et al. (eds.). Medical Genetics Summaries. National Center for Biotechnology Information (NCBI). PMID 28520380. Archived from the original on 26 October 2020. Retrieved 6 February 2020.
| External sites: |
|
|---|---|
| Identifiers: |