Atrioventricular reentrant tachycardia
| Atrioventricular reentrant tachycardia | |
|---|---|
| Other names: Atrioventricular reciprocating tachycardia, atrioventricular reentry tachycardia | |
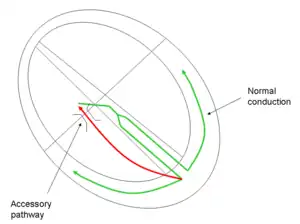 | |
| Conduction pathway in atrioventricular reentrant tachycardia, a form of supraventricular tachycardia | |
| Specialty | Cardiology |
| Symptoms | Palpitations, lightheadedness, chest discomfort[1][2] |
| Usual onset | Sudden[1] |
| Duration | Episodic[1] |
| Types | Orthodromic (90%), antidromic (10%)[2] |
| Causes | Wolff–Parkinson–White syndrome[2] |
| Risk factors | Genetics[3] |
| Diagnostic method | Electrocardiogram (ECG)[2] |
| Differential diagnosis | Orthodromic: AVNRT, sinus tachycardia, atrial flutter[2] Antidromic: Ventricular tachycardia[2] |
| Treatment | Vagal maneuvers, adenosine, procainamide, electrical cardioversion, ablation[2] |
| Frequency | Uncommon[2] |
Atrioventricular reentrant tachycardia (AVRT), is a type of abnormal fast heart rhythm.[4] Symptoms may include episodes of palpitations, lightheadedness, and chest discomfort.[1][2] Onset is generally sudden with a heart rate of 150 to 250 beats per minute.[1][2] Complications are rare.[2] It is a type of paroxysmal supraventricular tachycardia (PSVT).[1]
Causes include Wolff–Parkinson–White syndrome (WPW).[2] The underlying mechanism involves an accessory pathway which allows electrical signals to travel between the upper and lower chambers of the heart, outside the AV node.[2] There are two types: orthodromic in which the signal travels through the accessory pathway from the ventricle to the atria and the QRS complex is generally narrow; and antidromic in which the signal travels from the atria to the ventricle and the QRS complex is wide.[1] Permanent junctional reentrant tachycardia (PJRT) is a type of orthodromic AVRT.[1]
Initial treatment, in those who are otherwise stable, is often with vagal maneuvers.[2] If this is not effective adenosine may be used.[1] Other measures may include verapamil, procainamide, or beta blockers.[2] If this is not effective or the person is unstable electrical cardioversion may be carried out.[1] Recurrent attacks may be prevented with radiofrequency ablation.[4] In those who cannot have ablation flecainide may be used.[2]
AVRT is uncommon, affecting less than 1 % of people.[2] While about 0.2% of people have WPW on their ECG, not all develop a fast heart rate such as AVRT.[1] It is the second most common type of PSVT after AV nodal reentrant tachycardia (AVNRT).[4] Onset is often around the age of 9 to 37.[1] While an accessory pathway was first described in 1893 by Stanley Kent, symptomatic cases were not described until 1930 by Louis Wolff, John Parkinson, and Paul Dudley White.[3]
Signs and symptoms
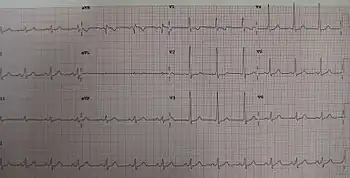
An episode of SVT may present with palpitations, dizziness, shortness of breath, or losing consciousness (fainting). The electrocardiogram (ECG) would appear as a narrow-complex SVT. Between episodes of tachycardia the affected person is likely to be asymptomatic, however, the ECG would demonstrate the classic delta wave in Wolff–Parkinson–White syndrome.[5]
Pathophysiology
.svg.png.webp)
Two distinct pathways are involved: the normal atrioventricular conduction system, and an accessory pathway. During AVRT, the electrical signal passes in the normal manner from the AV node into the ventricles. Then, the electrical impulse pathologically passes back into the atria via the accessory pathway, causing atrial contraction, and returns to the AV node to complete the reentrant circuit (see figure). Once initiated, the cycle may continue causing the heart to beat faster than usual.
Initiation of AVRT may be through a premature impulse of atrial, junctional, or ventricular origin.[6]
Treatment
Acute management is as for SVT in general. The aim is to interrupt the circuit. In people who are unstable, cardioversion may be necessary. In the absence of shock, inhibition at the AV node is attempted. This is achieved first by a trial of specific physical maneuvers such as holding a breath in or bearing down. If these maneuvers fail, using intravenous adenosine[7] causes complete electrical blockade at the AV node and interrupts the reentrant electrical circuit. Long-term management includes beta blocker therapy and radiofrequency ablation of the accessory pathway.
See also
References
- 1 2 3 4 5 6 7 8 9 10 11 12 Page, Richard L.; Joglar, José A.; Caldwell, Mary A.; Calkins, Hugh; Conti, Jamie B.; Deal, Barbara J.; Estes, N. A. Mark; Field, Michael E.; Goldberger, Zachary D. (May 2016). "2015 ACC/AHA/HRS Guideline for the Management of Adult Patients With Supraventricular Tachycardia: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society". Journal of the American College of Cardiology. 67 (13): e27–e115. doi:10.1016/j.jacc.2015.08.856. ISSN 1558-3597. PMID 26409259.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 Jabbour, F; Grossman, SA (January 2020). "Atrioventricular Reciprocating Tachycardia". PMID 30969587.
{{cite journal}}: Cite journal requires|journal=(help) - 1 2 Tsiperfal, Angela; Ottoboni, Linda K.; Beheiry, Salwa; Al-Ahmad, Amin; Natale, Andrea; Wang, Paul J. (2011). Cardiac Arrhythmia Management: A Practical Guide for Nurses and Allied Professionals. John Wiley & Sons. p. 59. ISBN 978-0-470-95932-9. Archived from the original on 2021-08-27. Retrieved 2021-02-09.
- 1 2 3 Helton, MR (1 November 2015). "Diagnosis and Management of Common Types of Supraventricular Tachycardia". American family physician. 92 (9): 793–800. PMID 26554472.
- ↑ Hampton J. The ECG Made Easy. Elsevier 2008
- ↑ "UpToDate: Atrioventricular reentrant tachycardia (AVRT) associated with an accessory pathway". Archived from the original on 2014-11-29. Retrieved 2014-04-12.
- ↑ "UK Resuscitation Council. Adult tachycardia algorithm. 2010" (PDF). Archived (PDF) from the original on 2014-12-25. Retrieved 2014-04-13.
External links
| Classification |
|---|