Vanoxerine
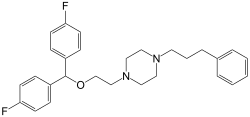
Vanoxerine is a piperazine derivative which is a potent and selective dopamine reuptake inhibitor (DRI). Vanoxerine binds to the target site on the dopamine transporter (DAT) ~ 50 times more strongly than cocaine,[1] but simultaneously inhibits the release of dopamine. This combined effect only slightly elevates dopamine levels, giving vanoxerine only mild stimulant effects.[2] Vanoxerine has also been observed to be a potent blocker of the IKr (hERG) channel.[3] Vanoxerine also binds with nanomolar affinity to the serotonin transporter.[4]
 | |
 | |
| Clinical data | |
|---|---|
| Other names | GBR-12909 |
| ATC code |
|
| Pharmacokinetic data | |
| Elimination half-life | 6 hours approx |
| Identifiers | |
| |
| CAS Number |
|
| PubChem CID | |
| DrugBank |
|
| ChemSpider | |
| UNII |
|
| ChEBI | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| Chemical and physical data | |
| Formula | C28H32F2N2O |
| Molar mass | 450.574 g·mol−1 |
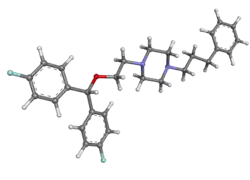
| 3D model (JSmol) | |
| |
| |
| | |
Vanoxerine as a treatment for cocaine dependence
Vanoxerine has been researched for use in treating cocaine dependence both as a substitute for cocaine and to block the rewarding effects. This strategy of using a competing agonist with a longer half-life has been successfully used to treat addiction to opiates such as heroin by substituting with methadone. It was hoped that vanoxerine would be of similar use in treating cocaine addiction.[5][6]
Research also indicates that vanoxerine may have additional mechanisms of action including antagonist action at nicotinic acetylcholine receptors,[7] and it has also been shown to reduce the consumption of alcohol in animal models of alcohol use disorder.[8]
Vanoxerine has been through human trials up to Phase II,[9][10][11] but development was stopped due to observed QTc effects in the context of cocaine use.[12]
However, vanoxerine analogs continue to be studied as treatments for cocaine addiction.[13][14] As an example, GBR compounds are piperazine based and contain a proximal and a distal nitrogen. It was found that piperidine analogs are still fully active DRIs, although they do not have any affinity for the "piperazine binding site" unlike the GBR compounds. Further SAR revealed that while there are 4 atoms connecting the two fluorophenyl rings to the piperazine, the ether in the chain could be omitted in exchange for a tertiary nitrogen. Vanoxerine, a blocker of the dopamine carrier devoid of action on the noradrenaline carrier, while greatly increasing dopamine in the nucleus accumbens, is ineffective in raising extracellular dopamine in the prefrontal cortex.[15]
Vanoxerine as an antiarrhythmic
Vanoxerine is a drug that was in the midst of recruiting participants for a phase III human clinical trial for its use as a cardiac antiarrhythmic when safety concerns arose. It had passed phase IIb human trials without any concerns but the company, Laguna Pharmaceuticals, found safety issues which prompted them to shut down their company and the $30 million effort to produce a new heart medication.[16] It was previously indicated as a treatment for Parkinson’s disease and depression; however, it had no significant benefit with these diseases.[17]
Medical uses
Vanoxerine is a potentially effective treatment for abnormal heart rhythms. A significant cause of abnormal heart rhythms is reentry, an electrophysiologic event in which the proliferating signal refuses to terminate, and endures to preexcite the heart after the refractory period.[18]
It is likely that vanoxerine acts to prevent reentrant circuits. Vanoxerine terminates atrial flutters and atrial fibrillations (both cardiac abnormal heart rhythms) by blocking the recirculating electrical signal, and preventing the reformation of the reentrant circuit.[19] Vanoxerine has also shown a tendency to reduce the recurrence of cardiac arrhythmias, as it was exceedingly difficult to reproduce an atrial flutter or fibrillation in a subject that had been taking vanoxerine.[3]
Experiments have successfully been performed on cell cultures, canine hosts and testing has moved towards human trials.
In clinical human trials with increasing dosages, vanoxerine has shown to have a highly favourable therapeutic index, showing no side effects at concentrations much higher than the therapeutic dose.[3] In canines, the effective therapeutic dose was between 76 ng/ml and 99 ng/ml, however the drug reached plasma concentrations of 550 ng/ml without harmful side effects, presenting a desirable therapeutic index.[3]
One of the major benefits of vanoxerine is that it does not appear to cause the same harmful side effects as its most comparable contender, amiodarone.[17]
Cellular mechanism
At a cellular level, vanoxerine acts to block cardiac ion channels.[17] Vanoxerine is a multichannel blocker, acting on IKr (potassium), L-type calcium and sodium ion channels.[17] By blocking these specific channels, there is a prolongation of the action potential of the cell, preventing reactivation by a reentrant circuit. The block is strongly frequency dependant: as the pacing of the heart increases so does the frequency of ion channel blocking by vanoxerine.[17]
Molecular mechanism
At this time, little is known about the molecular mechanism of vanoxerine, and steps are being made towards understanding how vanoxerine operates on a molecular level.
References
- Izenwasser S, Werling LL, Cox BM (June 1990). "Comparison of the effects of cocaine and other inhibitors of dopamine uptake in rat striatum, nucleus accumbens, olfactory tubercle, and medial prefrontal cortex". Brain Research. 520 (1–2): 303–9. doi:10.1016/0006-8993(90)91719-W. PMID 2145054. S2CID 24436917.
- Singh S (March 2000). "Chemistry, design, and structure-activity relationship of cocaine antagonists". Chemical Reviews. 100 (3): 925–1024. doi:10.1021/cr9700538. PMID 11749256.
- Cakulev I, Lacerda AE, Khrestian CM, Ryu K, Brown AM, Waldo AL (November 2011). "Oral vanoxerine prevents reinduction of atrial tachyarrhythmias: preliminary results". Journal of Cardiovascular Electrophysiology. 22 (11): 1266–73. doi:10.1111/j.1540-8167.2011.02098.x. PMC 3172341. PMID 21615815.
- Cararas SA, Izenwasser S, Wade D, Housman A, Verma A, Lomenzo SA, Trudell ML (December 2011). "Further structure-activity relationship studies on 8-substituted-3-[2-(diarylmethoxyethylidenyl)]-8-azabicyclo[3.2.1]octane derivatives at monoamine transporters". Bioorganic & Medicinal Chemistry. 19 (24): 7551–8. doi:10.1016/j.bmc.2011.10.028. PMC 3230044. PMID 22055716.
- Vetulani J (2001). "Drug addiction. Part III. Pharmacotherapy of addiction" (PDF). Polish Journal of Pharmacology. 53 (5): 415–34. PMID 11990060.
- Preti A (June 2007). "New developments in the pharmacotherapy of cocaine abuse". Addiction Biology. 12 (2): 133–51. doi:10.1111/j.1369-1600.2007.00061.x. PMID 17508985. S2CID 21834607.
- Szasz BK, Vizi ES, Kiss JP (March 2007). "Nicotinic acetylcholine receptor antagonistic property of the selective dopamine uptake inhibitor, GBR-12909 in rat hippocampal slices". Neuroscience. 145 (1): 344–9. doi:10.1016/j.neuroscience.2006.11.032. PMID 17207584. S2CID 25447970.
- Kamdar NK, Miller SA, Syed YM, Bhayana R, Gupta T, Rhodes JS (June 2007). "Acute effects of naltrexone and GBR 12909 on ethanol drinking-in-the-dark in C57BL/6J mice". Psychopharmacology. 192 (2): 207–17. doi:10.1007/s00213-007-0711-5. PMID 17273875. S2CID 12497800.
- Søgaard U, Michalow J, Butler B, Lund Laursen A, Ingersen SH, Skrumsager BK, Rafaelsen OJ (October 1990). "A tolerance study of single and multiple dosing of the selective dopamine uptake inhibitor GBR 12909 in healthy subjects". International Clinical Psychopharmacology. 5 (4): 237–51. doi:10.1097/00004850-199010000-00001. PMID 2150527. S2CID 32605858.
- Preti A (October 2000). "Vanoxerine National Institute on Drug Abuse". Current Opinion in Investigational Drugs. 1 (2): 241–51. PMID 11249581.
- Gorelick DA, Gardner EL, Xi ZX (2004). "Agents in development for the management of cocaine abuse". Drugs. 64 (14): 1547–73. doi:10.2165/00003495-200464140-00004. PMID 15233592. S2CID 5421657.
- Herman BH, Elkashef A, Vocci F (2005). "Medications for the treatment of cocaine addiction: Emerging candidates". Drug Discovery Today. 2 (1): 87–92. doi:10.1016/j.ddstr.2005.05.014.
- Rothman RB, Baumann MH, Prisinzano TE, Newman AH (January 2008). "Dopamine transport inhibitors based on GBR12909 and benztropine as potential medications to treat cocaine addiction". Biochemical Pharmacology. 75 (1): 2–16. doi:10.1016/j.bcp.2007.08.007. PMC 2225585. PMID 17897630.
- Runyon SP, Carroll FI (2006). "Dopamine transporter ligands: recent developments and therapeutic potential". Current Topics in Medicinal Chemistry. 6 (17): 1825–43. doi:10.2174/156802606778249775. PMID 17017960.
- Tanda G, Bassareo V, Di Chiara G (January 1996). "Mianserin markedly and selectively increases extracellular dopamine in the prefrontal cortex as compared to the nucleus accumbens of the rat". Psychopharmacology. 123 (2): 127–30. doi:10.1007/bf02246169. PMID 8741935. S2CID 43300151.
- Glenn B (21 November 2011). "Drug developer ChanRx closes series A investment, hires CEO". MEDCITY News. Retrieved 11 March 2012.
- Lacerda AE, Kuryshev YA, Yan GX, Waldo AL, Brown AM (March 2010). "Vanoxerine: cellular mechanism of a new antiarrhythmic". Journal of Cardiovascular Electrophysiology. 21 (3): 301–10. doi:10.1111/j.1540-8167.2009.01623.x. PMC 3107714. PMID 19817928.
- Mahmud F, Shiozawa N, Makikawa M, Nomura T (June 2011). "Reentrant excitation in an analog-digital hybrid circuit model of cardiac tissue". Chaos. 21 (2): 023121. Bibcode:2011Chaos..21b3121M. doi:10.1063/1.3597645. PMID 21721763.
- Matsumoto N, Khrestian CM, Ryu K, Lacerda AE, Brown AM, Waldo AL (March 2010). "Vanoxerine, a new drug for terminating atrial fibrillation and flutter". Journal of Cardiovascular Electrophysiology. 21 (3): 311–9. doi:10.1111/j.1540-8167.2009.01622.x. PMID 19817929. S2CID 32305356.