Fructose malabsorption
| Fructose malabsorption | |
|---|---|
| Other names: Dietary fructose intolerance | |
 | |
| Chemical structure of fructose | |
Fructose malabsorption, formerly named dietary fructose intolerance (DFI), is a digestive disorder[1] in which absorption of fructose is impaired by deficient fructose carriers in the small intestine's enterocytes. This results in an increased concentration of fructose in the entire intestine. Intolerance to fructose was first identified and reported in 1956.[2]
Fructose malabsorption is fairly common, affecting up to 1 in 3 people.[3] Occurrence in patients identified to have symptoms of irritable bowel syndrome is not higher than occurrence in the normal population. However, due to the similarity in symptoms, patients with fructose malabsorption often fit the profile of those with irritable bowel syndrome.[4] In some cases, fructose malabsorption may be caused by several diseases which cause intestinal damage, such as celiac disease.[5]
Fructose malabsorption is not to be confused with hereditary fructose intolerance, a potentially fatal condition in which the liver enzymes that break up fructose are deficient.
Symptoms and signs
Fructose malabsorption may cause gastrointestinal symptoms such as abdominal pain, bloating, flatulence or diarrhea.[6][7]
Pathophysiology
Fructose is absorbed in the small intestine without help of digestive enzymes. Even in healthy persons, however, only about 25–50 g of fructose per sitting can be properly absorbed. People with fructose malabsorption absorb less than 25 g per sitting.[8] Simultaneous ingestion of fructose and sorbitol seems to increase malabsorption of fructose.[5] Fructose that has not been adequately absorbed is fermented by intestinal bacteria producing hydrogen, carbon dioxide, methane and short-chain fatty acids.[6][9] This abnormal increase in hydrogen may be detectable with the hydrogen breath test.[5]
The physiological consequences of fructose malabsorption include increased osmotic load, rapid bacterial fermentation, altered gastrointestinal motility, the formation of mucosal biofilm and altered profile of bacteria. These effects are additive with other short-chain poorly absorbed carbohydrates such as sorbitol. The clinical significance of these events depends upon the response of the bowel to such changes. Some effects of fructose malabsorption are decreased tryptophan,[10] folic acid[11] and zinc in the blood.[11]
Restricting dietary intake of free fructose and/or fructans may provide symptom relief in a high proportion of patients with functional gut disorders.[12]
Diagnosis
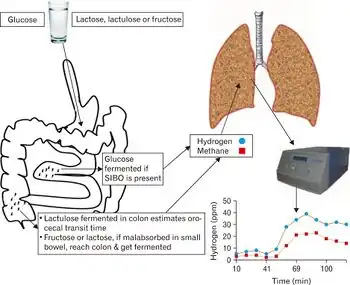
The diagnostic test, when used, is similar to that used to diagnose lactose intolerance. It is called a hydrogen breath test and is the method currently used for a clinical diagnosis. Nevertheless, some authors argue this test is not an appropriate diagnostic tool, because a negative result does not exclude a positive response to fructose restriction, implying a lack of sensitivity.[5]
Treatment
Physical activity (avoiding sitting down for long periods)
Sitting down can cause your abdomen to compress, which slows down digestion. This can lead to issues such as bloating, heartburn and constipation.[14] It could thus increase or cause fructose malabsorption. A study show that physical activity between long periods of sitting is not enough: "focusing on acquiring the recommended dose of exercise is not a strong enough of a stimulant to completely protect the body from physical inactivity the other 23+ h/day".[15] "Reducing prolonged overall sitting time may reduce metabolic disturbances"[16]
Dietary supplements
Xylose isomerase acts to convert fructose sugars into glucose. Dietary supplements of xylose isomerase may improve some symptoms of fructose malabsorption, although there is currently only a single scientific study available.[17]
Diet
There is no known cure, but an appropriate diet and the enzyme xylose isomerase can help.[5] The ingestion of glucose simultaneously with fructose improves fructose absorption and may prevent the development of symptoms. For example, people may tolerate fruits such as grapefruits or bananas, which contain similar amounts of fructose and glucose, but apples are not tolerated because they contain high levels of fructose and lower levels of glucose.[6] But a randomised controlled trials in patients with fructose malabsorption (made by the Cochrane institute) found that "Adding glucose to food and solutions to enhance fructose absorption is not effective in preventing fructose-induced functional gastrointestinal symptoms".[18]
Foods that should be avoided by people with fructose malabsorption include:
- Foods and beverages containing greater than 0.5 g fructose in excess of glucose per 100 g and greater than 0.2 g of fructans per serving should be avoided. Foods with >3 g of fructose per serving are termed a 'high fructose load' and possibly present a risk of inducing symptoms. However, the concept of a 'high fructose load' has not been evaluated in terms of its importance in the success of the diet.[19]
- Foods with high fructose-to-glucose ratio. Glucose enhances absorption of fructose, so fructose from foods with fructose-to-glucose ratio <1, like white potatoes, are readily absorbed, whereas foods with fructose-to-glucose ratio >1, like apples and pears, are often problematic regardless of the total amount of fructose in the food.[20]
- Foods rich in fructans and other fermentable oligo-, di- and mono-saccharides and polyols (FODMAPs), including artichokes, asparagus, leeks, onions, and wheat-containing products, including breads, cakes, biscuits, breakfast cereals, pies, pastas, pizzas, and wheat noodles.
- The role that fructans play in fructose malabsorption is still under investigation. However, it is recommended that fructan intake for fructose malabsorbers should be kept to less than 0.5 grams/serving,[21] and supplements with inulin and fructooligosaccharide (FOS), both fructans, should be avoided.[21]
- Foods containing artificial sweeteners like sorbitol (present in some diet drinks and foods and occurring naturally in some stone fruits), xylitol (present in some berries) and other polyols (sugar alcohols, such as erythritol, mannitol and other ingredients that end with -tol, commonly added as in commercial foods).
- Foods containing high fructose corn syrup.
Foods with a high glucose content ingested with foods containing excess fructose may help patients absorb the excess fructose.[22]
Foods with high fructose content
According to the USDA database,[23] foods with more fructose than glucose include:
| Food | Fructose (grams / 100 grams) | Glucose (grams / 100 grams) |
|---|---|---|
| Sucrose (for reference) |
50 | 50 |
| Apples | 5.9 | 2.4 |
| Pears | 6.2 | 2.8 |
| Fruit juice e.g. Apples, Pears |
5–7 | 2–3 |
| Watermelon | 3.4 | 1.6 |
| Raisins | 29.8 | 27.8 |
| Honey | 40.9 | 35.7 |
| High fructose corn syrup |
42–55 | 42–53 |
| Mango | 4.68 | 2.01 |
| Agave nectar | 55.6 | 12.43 |
| Ginger | 1.78 | 1.22 |
The USDA food database reveals that many common fruits contain nearly equal amounts of the fructose and glucose, and they do not present problems for those individuals with fructose malabsorption.[24] Some fruits with a greater ratio of fructose than glucose are apples, pears and watermelon, which contain more than twice as much fructose as glucose. Fructose levels in grapes varies depending on ripeness and variety, where unripe grapes contain more glucose.
Dietary guidelines for management
Researchers at Monash University in Australia developed dietary guidelines[21] for managing fructose malabsorption, particularly for individuals with IBS.
Unfavorable foods (i.e. more fructose than glucose)
- Fruit – apple, pear, honeydew melon, nashi pear, pawpaw, papaya, quince, star fruit, watermelon;
- Dried fruit – apple, currant, date, fig, pear, raisin, sultana;
- Fortified wines
- Foods containing added sugars, such as agave nectar, some corn syrups, and fruit juice concentrates.
Favorable foods (i.e. fructose equal to or less than glucose)
The following list of favorable foods was cited in the paper: "Fructose malabsorption and symptoms of Irritable Bowel Syndrome Guidelines for effective dietary management".[21] The fructose and glucose contents of foods listed on the Australian food standards[25] would appear to indicate that most of the listed foods have higher fructose levels.
- Stone fruit: apricot, nectarine, peach, plum (caution – these fruits contain sorbitol);
- Berry fruit: blackberry, boysenberry, cranberry, raspberry, strawberry, loganberry;
- Citrus fruit: kumquat, grapefruit, lemon, lime, mandarin, orange, tangelo;
- Other fruits: ripe banana, jackfruit, passion fruit, pineapple, rhubarb, tamarillo.
Food-labeling
Producers of processed food in most or all countries, including the US, are not currently required by law to mark foods containing "fructose in excess of glucose". This can cause some surprises and pitfalls for fructose malabsorbers.
Foods (such as bread) marked "gluten-free" are usually suitable for fructose malabsorbers, though they need to be careful of gluten-free foods that contain dried fruit or high fructose corn syrup or fructose itself in sugar form. However, fructose malabsorbers do not need to avoid gluten, as those with celiac disease must.
Many fructose malabsorbers can eat breads made from rye and corn flour. However, these may contain wheat unless marked "wheat-free" (or "gluten-free") (Note: Rye bread is not gluten-free.) Although often assumed to be an acceptable alternative to wheat, spelt flour is not suitable for people with fructose malabsorption, just as it is not appropriate for those with wheat allergies or celiac disease. However, some fructose malabsorbers do not have difficulty with fructans from wheat products while they may have problems with foods that contain excess free fructose.
There are many breads on the market that boast having no high fructose corn syrup. In lieu of high fructose corn syrup, however, one may find the production of special breads with a high inulin content, where inulin is a replacement in the baking process for the following: high fructose corn syrup, flour and fat. Because of the caloric reduction, lower fat content, dramatic fiber increase and prebiotic tendencies of the replacement inulin, these breads are considered a healthier alternative to traditionally prepared leavening breads. Though the touted health benefits may exist, people with fructose malabsorption will likely find no difference between these new breads and traditionally prepared breads in alleviating their symptoms because inulin is a fructan, and, again, consumption of fructans should be reduced dramatically in those with fructose malabsorption in an effort to appease symptoms.
Research
Fructose and fructans are FODMAPs (fermentable oligo-, di- and mono-saccharides and polyols) known to cause gastrointestinal discomfort in susceptible individuals. FODMAPs are not the cause of these disorders,[26] but FODMAPs restriction (a low-FODMAP diet) might help to improve short-term digestive symptoms in adults with irritable bowel syndrome (IBS) and other functional gastrointestinal disorders (FGID).[26][27][28][29] Nevertheless, its long-term follow-up can have negative effects because it causes a detrimental impact on the gut microbiota and metabolome.[28][29][30][31]
See also
References
- ↑ "MayoClinic.com". Archived from the original on 31 July 2019. Retrieved 25 August 2022.
- ↑ Chambers, R.A; Pratt, R.T.C (1956). "Idiosyncrasy to Fructose". The Lancet. 268 (6938): 340. doi:10.1016/S0140-6736(56)92196-1. PMID 13358219.
- ↑ "Fructose Malabsorption: Symptoms, Management, and More". Healthline. 19 September 2017. Archived from the original on 4 September 2022. Retrieved 25 August 2022.
- ↑ Ledochowski M, et al. (2001). "Fruktosemalabsorption" (PDF). Journal für Ernährungsmedizin (in Deutsch). 3 (1): 15–19. Archived (PDF) from the original on 2 April 2012. Retrieved 25 August 2022.
- 1 2 3 4 5 Berni Canani, Roberto; Pezzella, Vincenza; Amoroso, Antonio; Cozzolino, Tommaso; Di Scala, Carmen; Passariello, Annalisa (2016). "Diagnosing and Treating Intolerance to Carbohydrates in Children". Nutrients. 8 (3): 157. doi:10.3390/nu8030157. PMC 4808885. PMID 26978392.
- 1 2 3 Ebert, Karolin; Witt, Heiko (2016). "Fructose malabsorption". Molecular and Cellular Pediatrics. 3 (1): 10. doi:10.1186/s40348-016-0035-9. PMC 4755956. PMID 26883354.
- ↑ Putkonen L, Yao CK, Gibson PR (July 2013). "Fructose malabsorption syndrome". Curr Opin Clin Nutr Metab Care (Review). 16 (4): 473–7. doi:10.1097/MCO.0b013e328361c556. PMID 23739630. S2CID 3124240.
- ↑ "University of Iowa Hospitals & Clinics". Archived from the original on 20 April 2009. Retrieved 25 August 2022.
- ↑ Montalto M, Gallo A, Ojetti V, Gasbarrini A (2013). "Fructose, trehalose and sorbitol malabsorption" (PDF). Eur Rev Med Pharmacol Sci (Review). 17 (Suppl 2): 26–9. PMID 24443064. Archived (PDF) from the original on 12 April 2016. Retrieved 25 August 2022.
- ↑ Ledochowski M, Widner B, Murr C, Sperner-Unterweger B, Fuchs D (2001). "Fructose malabsorption is associated with decreased plasma tryptophan". Scand. J. Gastroenterol. 36 (4): 367–71. CiteSeerX 10.1.1.627.6642. doi:10.1080/003655201300051135. PMID 11336160.
- 1 2 Ledochowski M, Uberall F, Propst T, Fuchs D (1999). "Fructose malabsorption is associated with lower plasma folic acid concentrations in middle-aged subjects". Clin. Chem. 45 (11): 2013–4. doi:10.1093/clinchem/45.11.2013. PMID 10545075. Archived from the original on 27 September 2011. Retrieved 25 August 2022.
- ↑ Gibson, P. R; Newnham, E; Barrett, J. S; Shepherd, S. J; Muir, J. G (2006). "Review article: Fructose malabsorption and the bigger picture". Alimentary Pharmacology & Therapeutics. 25 (4): 349–63. doi:10.1111/j.1365-2036.2006.03186.x. PMID 17217453.
- ↑ Ghoshal, Uday C (2011). "How to Interpret Hydrogen Breath Tests". Journal of Neurogastroenterology and Motility. 17 (3): 312–317. doi:10.5056/jnm.2011.17.3.312. ISSN 2093-0879. Retrieved 3 December 2022.
- ↑ "What Sitting All Day Does To Your Body (Spoiler Alert: It's Not Great)". HuffPost UK. 26 March 2019. Archived from the original on 1 September 2022. Retrieved 3 September 2021.
- ↑ Gardiner, Paul A.; Healy, Genevieve N.; Eakin, Elizabeth G.; Clark, Bronwyn K.; Dunstan, David W.; Shaw, Jonathan E.; Zimmet, Paul Z.; Owen, Neville (May 2011). "Associations Between Television Viewing Time and Overall Sitting Time with the Metabolic Syndrome in Older Men and Women: The Australian Diabetes Obesity and Lifestyle Study". Journal of the American Geriatrics Society. 59 (5): 788–796. doi:10.1111/j.1532-5415.2011.03390.x. ISSN 0002-8614. PMID 21568949. S2CID 19714433.
- ↑ Bidwell, Amy J. (28 May 2017). "Chronic Fructose Ingestion as a Major Health Concern: Is a Sedentary Lifestyle Making It Worse? A Review". Nutrients. 9 (6): 549. doi:10.3390/nu9060549. ISSN 2072-6643. PMC 5490528. PMID 28555043.
- ↑ Komericki, P.; Akkilic-Materna, M.; Strimitzer, T.; Weyermair, K.; Hammer, H.F.; Aberer, W. (2012). "Oral xylose isomerase decreases breath hydrogen excretion and improves gastrointestinal symptoms in fructose malabsorption – a double-blind, placebo-controlled study". Alimentary Pharmacology & Therapeutics. 36 (10): 980–987. doi:10.1111/apt.12057. PMID 23002720.
- ↑ Tuck, C. J.; Ross, L. A.; Gibson, P. R.; Barrett, J. S.; Muir, J. G. (2017). "Adding glucose to food and solutions to enhance fructose absorption is not effective in preventing fructose-induced functional gastrointestinal symptoms: randomised controlled trials in patients with fructose malabsorption". Journal of Human Nutrition and Dietetics. 30 (1): 73–82. doi:10.1111/jhn.12409. ISSN 1365-277X. PMID 27600184. S2CID 3722940. Archived from the original on 8 November 2020. Retrieved 25 August 2022.
- ↑ Gibson, Peter R; Shepherd, Susan J (2010). "Evidence-based dietary management of functional gastrointestinal symptoms: The FODMAP approach". Journal of Gastroenterology and Hepatology. 25 (2): 252–8. doi:10.1111/j.1440-1746.2009.06149.x. PMID 20136989.
- ↑ "Division of Gastroenterology & Hepatology — School of Medicine at the University of Virginia". Archived from the original (PDF) on 18 May 2012. Retrieved 2 December 2007.
- 1 2 3 4 Shepherd SJ, Gibson PR (2006). "Fructose malabsorption and symptoms of irritable bowel syndrome: guidelines for effective dietary management" (PDF). Journal of the American Dietetic Association. 106 (10): 1631–9. doi:10.1016/j.jada.2006.07.010. PMID 17000196. Archived (PDF) from the original on 14 March 2011. Retrieved 25 August 2022.
- ↑ Skoog SM, Bharucha AE (2004). "Dietary fructose and gastrointestinal symptoms: a review" (PDF). Am. J. Gastroenterol. 99 (10): 2046–50. doi:10.1111/j.1572-0241.2004.40266.x. PMID 15447771. S2CID 12084142. Archived from the original (PDF) on 1 April 2017. Retrieved 23 July 2006.
- ↑ USDA National Nutrient Database Archived 3 March 2015 at the Wayback Machine Release 20, September 2007
- ↑ Sugar Content of Selected Foods: Individual and Total Sugars Archived 7 September 2006 at the Wayback Machine Ruth H. Matthews, Pamela R. Pehrsson, and Mojgan Farhat-Sabet, (1987) U.S.D.A.
- ↑ "NUTTAB 2010 Online Searchable Database". Food Standards Australia New Zealand. Archived from the original on 24 March 2012. Retrieved 7 July 2013.
- 1 2 Peter R Gibson & Susan J Shepherd (2010). "Evidence-based dietary management of functional gastrointestinal symptoms: The FODMAP approach". Journal of Gastroenterology and Hepatology. 25 (2): 252–258. doi:10.1111/j.1440-1746.2009.06149.x. PMID 20136989.
- ↑ Turco R, Salvatore S, Miele E, Romano C, Marseglia GL, Staiano A (2018). "Does a low FODMAPs diet reduce symptoms of functional abdominal pain disorders? A systematic review in adult and paediatric population, on behalf of Italian Society of Pediatrics". Ital J Pediatr (Systematic Review). 44 (1): 53. doi:10.1186/s13052-018-0495-8. PMC 5952847. PMID 29764491.
- 1 2 Staudacher HM, Irving PM, Lomer MC, Whelan K (April 2014). "Mechanisms and efficacy of dietary FODMAP restriction in IBS". Nat Rev Gastroenterol Hepatol (Review). 11 (4): 256–66. doi:10.1038/nrgastro.2013.259. PMID 24445613. S2CID 23001679.
An emerging body of research now demonstrates the efficacy of fermentable carbohydrate restriction in IBS. [...] However, further work is urgently needed both to confirm clinical efficacy of fermentable carbohydrate restriction in a variety of clinical subgroups and to fully characterize the effect on the gut microbiota and the colonic environ¬ment. Whether the effect on luminal bifidobacteria is clinically relevant, preventable, or long lasting, needs to be investigated. The influence on nutrient intake, dietary diversity, which might also affect the gut microbiota,137 and quality of life also requires further exploration as does the possible economic effects due to reduced physician contact and need for medication. Although further work is required to confirm its place in IBS and functional bowel disorder clinical pathways, fermentable carbohydrate restriction is an important consideration for future national and international IBS guidelines.
- 1 2 Rao SS, Yu S, Fedewa A (2015). "Systematic review: dietary fibre and FODMAP-restricted diet in the management of constipation and irritable bowel syndrome". Aliment. Pharmacol. Ther. 41 (12): 1256–70. doi:10.1111/apt.13167. PMID 25903636. S2CID 27558785.
- ↑ Tuck, CJ; Muir, JG; Barrett, JS; Gibson, PR (2014). "Fermentable oligosaccharides, disaccharides, monosaccharides and polyols: role in irritable bowel syndrome". Expert Rev Gastroenterol Hepatol. 8 (7): 819–834. doi:10.1586/17474124.2014.917956. PMID 24830318. S2CID 28811344.
- ↑ Heiman ML, Greenway FL (2016). "A healthy gastrointestinal microbiome is dependent on dietary diversity". Mol Metab (Review). 5 (5): 317–320. doi:10.1016/j.molmet.2016.02.005. PMC 4837298. PMID 27110483.
External links
| Classification |
|---|