Canagliflozin
 | |
| Names | |
|---|---|
| Pronunciation | /ˌkænəɡlɪˈfloʊzɪn/ KAN-ə-glif-LOH-zin |
| Trade names | Invokana, Sulisent, Prominad, others |
IUPAC name
| |
| Clinical data | |
| Drug class | SGLT2 inhibitor[1] |
| Main uses | Type 2 diabetes[1] |
| Side effects | Vaginal yeast infections, nausea, constipation, urinary tract infection[1] |
| WHO AWaRe | UnlinkedWikibase error: ⧼unlinkedwikibase-error-statements-entity-not-set⧽ |
| Pregnancy category |
|
| Routes of use | By mouth (tablets) |
| Defined daily dose | 200 mg[2] |
| External links | |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a613033 |
| Legal | |
| License data |
|
| Legal status | |
| Pharmacokinetics | |
| Bioavailability | 65% |
| Protein binding | 99% |
| Metabolism | Liver glucuronidation |
| Elimination half-life | 11.8 (10–13) hours |
| Excretion | 53% faecal and 33% kidney |
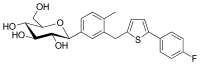
| Chemical and physical data | |
| Formula | C24H25FO5S |
| Molar mass | 444.52 g·mol−1 |
| 3D model (JSmol) | |
SMILES
| |
InChI
| |
Canagliflozin, sold under the brand name Invokana among others, is a medication used to treat type 2 diabetes.[1] It is a third-line medication to metformin.[3] It is used together with exercise and diet.[1] It is not recommended in type 1 diabetes.[1] It is taken by mouth.[1]
Common side effects include vaginal yeast infections, nausea, constipation, and urinary tract infections.[1] Serious side effects may include low blood sugar, Fournier's gangrene, leg amputation, kidney problems, high blood potassium, and low blood pressure.[1] Diabetic ketoacidosis may occur despite nearly normal blood sugar levels.[1] Use in pregnancy and breastfeeding is not recommended.[4] Canagliflozin is a sodium-glucose cotransporter 2 (SGLT2) inhibitor.[1] It works by increasing the amount of glucose lost in the urine.[1]
Canagliflozin was approved for medical use in the United States in 2013.[1] It is on the World Health Organization's List of Essential Medicines as an alternative to empagliflozin.[5] A month's supply in the United Kingdom costs the NHS about £39 as of 2019.[3] In the United States the wholesale cost of this amount is about US$475.[6] In 2017, it was the 192nd most commonly prescribed medication in the United States, with more than three million prescriptions.[7][8]
Medical use
Canagliflozin is an anti-diabetic medication used to improve blood sugar control in people with type 2 diabetes. It is a third line medication to metformin.[3] Per the British National Formulary it is also less preferred than a sulfonylurea as of 2019 while the American Diabetes Association and European Association for the Study of Diabetes consider either a SGLT2 inhibitor or GLP-1 receptor agonist a reasonable second line medication in those with heart disease.[9]
Canagliflozin decreases HbA1c levels by 0.77% to 1.16% when given by itself, in combination with metformin, in combination with metformin and a sulfonylurea, in combination with metformin and pioglitazone, or in combination with insulin, from initial HbA1c levels of 7.8% to 8.1%. When added to metformin, canagliflozin does not appear worse than sitagliptin or glimepiride in reducing HbA1c levels, while canagliflozin maybe better than sitagliptin and glimiperide in decreasing HbA1c. It is unclear whether or not it has any unique cardiovascular benefits beyond lowering blood sugar.[10] Although canagliflozin produces beneficial effects on HDL cholesterol, it has also been shown to increase LDL cholesterol to produce no change in total cholesterol.[11][12]
Evidence shows that apart from positive effects on glycemic levels, canagliflozin also provides reduces the risk of heart attacks and heart failures.[13]
SGLT2 inhibitors, including canagliflozin, reduce the likelihood of hospitalization for congestive heart failure or progression of renal disease in persons with diabetes mellitus type 2 and reduce the likelihood of stroke and heart attack in persons with diabetes mellitus type 2 who have known atherosclerotic vascular disease.[14]
Dosage
The defined daily dose is 200 mg by mouth.[2]
Contraindications
Canaglifozin is contraindicated in:
- Type 1 diabetes
- Diabetic ketoacidosis[15]
- Severe renal impairment (estimated glomerular filtration rate <30 mL/min/1.73 m2), end-stage renal disease[16]
- Patients on dialysis[12]
Side effects
As with all SGLT2 inhibitors, canagliflozin is associated with increased risk of urinary tract infections, fungal infections of the genital area, thirst,[17] elevations in LDL cholesterol, increased urination and episodes of low blood pressure. Rarely, use of canagliflozin is associated with necrotizing fasciitis of the perineum, also called Fournier gangrene.[18] There are concerns that it may also increase the risk of diabetic ketoacidosis.[19]
Possible cardiovascular problems are an ongoing issue with gliflozin drugs.[20] The pre-specified endpoint for cardiovascular safety in the canagliflozin clinical development program was "Major Cardiovascular Events Plus", defined as the occurrence of cardiovascular death, non-fatal myocardial infarctions, non-fatal strokes, or unstable angina leading to hospitalization. This endpoint occurred in more people in the placebo group (20.5%) than in the canagliflozin treated group (18.9%).
Nonetheless, a United States Food and Drug Administration advisory committee expressed concern regarding the cardiovascular safety of canagliflozin. A greater number of cardiovascular events was observed during the first 30 days in study subjects who received canagliflozin (0.45%) compared those who received placebo (0.07%), suggesting an early period of increased cardiovascular risk. In addition, there was an increased risk of stroke in subjects who received canagliflozin. However, none of these effects were statistically significant. Additional cardiovascular safety data from another ongoing study are expected in 2015.[20]
On May 15, 2015, the FDA issued a warning that certain SGLT2 diabetes drugs, including canagliflozin, may lead to ketoacidosis, a condition where the body produces higher levels of ketone bodies. The FDA is continuing to investigate the issue, and cautions that patients should not stop taking canagliflozin without first talking to their doctor.[21]
On September 10, 2015, the FDA issued a drug safety communication for canagliflozin to address risks for bone fracture and decreased bone density. A label warning for fractures was already included in the Adverse Reactions section; however, the FDA made the addition to the Warnings and Precautions section to reflect new information from a placebo study. They advised that health care professionals should consider fracture risk factors before prescribing canagliflozin, and patients should disclose any bone fracture risk factors to their doctors, but that patients should not stop taking the medication without first talking to their doctor.[22]
On December 4, 2015, the FDA issued another safety communication for SGLT2 inhibitors, indicating that it would require new warnings to be added to the canagliflozin label about elevated blood acid levels and urinary tract infections.[23]
A June 29, 2016 report on the ongoing cardiovascular outcomes trial for canagliflozin (CANVAS) revealed interim findings of new safety concerns including heightened risk of bone fracture that was found to increase with the duration of treatment.[24]
On May 16, 2017, the FDA concluded that canagliflozin causes an increased risk of leg and foot amputations.[25] The FDA began requiring a boxed warning to be added to the canagliflozin drug labels to describe this risk.[26]
To lessen the risk of developing ketoacidosis (a serious condition in which the body produces high levels of blood acids called ketones) after surgery, the FDA has approved changes to the prescribing information for SGLT2 inhibitor diabetes medicines to recommend they be stopped temporarily before scheduled surgery. Canagliflozin, dapagliflozin, and empagliflozin should each be stopped at least three days before, and ertugliflozin should be stopped at least four days before scheduled surgery.[27]
Symptoms of ketoacidosis include nausea, vomiting, abdominal pain, tiredness, and trouble breathing.[27]
Interactions
The drug may increase the risk of dehydration in combination with diuretic drugs.[28]
Because it increases renal excretion of glucose, treatment with canagliflozin prevents renal reabsorption of 1,5-anhydroglucitol, leading to artifactual decreases in serum 1,5-anhydroglucitol. Therefore, canagliflozin can interfere with the use of serum 1,5-anhydroglucitol (assay trade name, GlycoMark) as a measure of postprandial glucose levels.[29]
Dosing adjustment is also required for concomitant therapy with UDP-glucuronosyl transferase (UGT) inducers such as rifampin, phenytoin, or phenobarbital, ritonavir.[1]
Pharmacology
Mechanism of action
Canagliflozin is an inhibitor of subtype 2 sodium-glucose transport proteins (SGLT2), which is responsible for at least 90% of renal glucose reabsorption (the remaining 10% is done by SGLT1). Blocking this transporter causes up to 119 grams of blood glucose per day to be eliminated through the urine,[30] corresponding to 476 kilocalories. Additional water is eliminated by osmotic diuresis, resulting in a lowering of blood pressure.
This mechanism is associated with a low risk of hypoglycaemia (too low blood glucose) compared to other types of anti-diabetic drugs such as sulfonylurea derivatives and insulin.[31]
Pharmacokinetics
When taken by mouth, canagliflozin reaches highest blood plasma concentrations after one to two hours and has an absolute bioavailability of 65%, independently of food intake. When in the bloodstream, 99% of the substance are bound to plasma proteins, mainly albumin. It is metabolized mainly by O-glucuronidation via the enzymes UGT1A9 and UGT2B4, and by hydroxylation to a lesser extent. The terminal half life is 10.6 hours for a 100 mg dose and 13.1 hours for a 300 mg dose, with 43% being excreted in the faeces (mostly in unchanged form) and 33% in the urine (mostly as glucuronide).[32]
History
It was developed by Mitsubishi Tanabe Pharma and is marketed under license by Janssen, a division of Johnson & Johnson.[33]
On July 4, 2011, the European Medicines Agency approved a paediatric investigation plan and granted both a deferral and a waiver for canagliflozin (EMEA-001030-PIP01-10) in accordance with EC Regulation No.1901/2006 of the European Parliament and of the council.[34]
Canagliflozin was approved by the FDA on March 29, 2013, and became the first SGLT2 inhibitor in the United States.[35][36]
Society and culture
Cost
A month's supply in the United Kingdom costs the NHS about £39 as of 2019.[3]In the United States the wholesale cost of this amount is about US$475.[6] In 2017, it was the 192nd most commonly prescribed medication in the United States, with more than three million prescriptions.[7][8]
.svg.png.webp) Canagliflozin costs (US)
Canagliflozin costs (US).svg.png.webp) Canagliflozin prescriptions (US)
Canagliflozin prescriptions (US)
See also
References
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 "Canagliflozin Monograph for Professionals". Drugs.com. American Society of Health-System Pharmacists. Archived from the original on 6 April 2019. Retrieved 6 April 2019.
- 1 2 "WHOCC - ATC/DDD Index". www.whocc.no. Archived from the original on 28 August 2021. Retrieved 8 September 2020.
- 1 2 3 4 British national formulary : BNF 76 (76 ed.). Pharmaceutical Press. 2018. p. 687. ISBN 9780857113382.
- ↑ "Canagliflozin (Invokana) Use During Pregnancy". Drugs.com. Archived from the original on 6 April 2019. Retrieved 6 April 2019.
- ↑ World Health Organization (2023). The selection and use of essential medicines 2023: web annex A: World Health Organization model list of essential medicines: 23rd list (2023). Geneva: World Health Organization. hdl:10665/371090. WHO/MHP/HPS/EML/2023.02.
- 1 2 "NADAC as of 2019-02-27". Centers for Medicare and Medicaid Services. Archived from the original on 2019-03-06. Retrieved 3 March 2019.
- 1 2 "The Top 300 of 2020". ClinCalc. Archived from the original on 12 February 2021. Retrieved 11 April 2020.
- 1 2 "Canagliflozin - Drug Usage Statistics". ClinCalc. Archived from the original on 13 April 2020. Retrieved 11 April 2020.
- ↑ Davies, Melanie J.; D’Alessio, David A.; Fradkin, Judith; Kernan, Walter N.; Mathieu, Chantal; Mingrone, Geltrude; Rossing, Peter; Tsapas, Apostolos; Wexler, Deborah J.; Buse, John B. (December 2018). "Management of Hyperglycemia in Type 2 Diabetes, 2018. A Consensus Report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD)". Diabetes Care. 41 (12): 2669–2701. doi:10.2337/dci18-0033. PMC 6245208. PMID 30291106.
patients with clinical CVD not meeting individualized glycemic targets while treated with metformin (or in whom metformin is contraindicated or not tolerated) should have an SGLT2 inhibitor or GLP-1 receptor agonist with proven benefit for cardiovascular risk reduction added
- ↑ Heston TF, Olson AH, Randall NR (December 2017). "Canagliflozin lowers blood sugar, but does it also lower cardiovascular risk? Maybe not". Annals of Translational Medicine. 5 (23): 473. doi:10.21037/atm.2017.09.28. PMC 5733311. PMID 29285506.
- ↑ "Summary Review" (PDF). fda.gov. March 29, 2013. Archived (PDF) from the original on 2014-10-31. Retrieved 2014-07-09.
- 1 2 "Invokana (canagliflozin) Tablets, for Oral Use. Full Prescribing Information" (PDF). Janssen Pharmaceuticals, Inc. Archived from the original (PDF) on 26 September 2016. Retrieved 14 November 2016.
- ↑ Usman MS, Siddiqi TJ, Memon MM, Khan MS, Rawasia WF, Talha Ayub M, Sreenivasan J, Golzar Y (March 2018). "Sodium-glucose co-transporter 2 inhibitors and cardiovascular outcomes: A systematic review and meta-analysis". European Journal of Preventive Cardiology. 25 (5): 495–502. doi:10.1177/2047487318755531. PMID 29372664.
- ↑ Zelniker TA, Wiviott SD, Raz I, Im K, Goodrich EL, Bonaca MP, Mosenzon O, Kato ET, Cahn A, Furtado RH, Bhatt DL, Leiter LA, McGuire DK, Wilding JP, Sabatine MS (January 2019). "SGLT2 inhibitors for primary and secondary prevention of cardiovascular and renal outcomes in type 2 diabetes: a systematic review and meta-analysis of cardiovascular outcome trials". Lancet. 393 (10166): 31–39. doi:10.1016/S0140-6736(18)32590-X. PMID 30424892.
- ↑ Canagliflozin. Lexi-Drugs. Lexicomp Online [database online]. Hudson, OH: Lexicomp, Inc. http://online.lexi.com. Updated April 8, 2017. Accessed April 13, 2017.
- ↑ Canagliflozin. Lexi-Drugs. Lexicomp Online [database online]. Hudson, OH: Lexicomp, Inc. http://online.lexi.com. Updated March 31, 2017. Accessed April 5, 2017.
- ↑ Haberfeld, H (ed.). Austria-Codex (in German) (2013/14, supplement 01/14 ed.). Vienna: Österreichischer Apothekerverlag.
{{cite book}}: CS1 maint: unrecognized language (link) - ↑ "Drug Safety and Availability - FDA warns about rare occurrences of a serious infection of the genital area with SGLT2 inhibitors for diabetes". FDA. 2019-02-09. Archived from the original on 2019-02-07. Retrieved 2019-02-02.
- ↑ FDA (2015-05-15). "SGLT2 inhibitors: Drug Safety Communication - FDA Warns Medicines May Result in a Serious Condition of Too Much Acid in the Blood". Archived from the original on 2016-10-27. Retrieved 19 May 2015.
- 1 2 Tucker, Miriam (10 January 2013). "FDA Advisory Panel Supports Diabetes Drug Canagliflozin". Medscape Family Medicine. Archived from the original on 16 June 2016. Retrieved 3 August 2015.
Safety discussions by the panel circled back repeatedly to the cardiovascular risk data
- ↑ Research, Center for Drug Evaluation and. "Drug Safety and Availability - FDA Drug Safety Communication: FDA warns that SGLT2 inhibitors for diabetes may result in a serious condition of too much acid in the blood". www.fda.gov. Archived from the original on 2017-07-22. Retrieved 2016-06-07.
- ↑ "FDA Drug Safety Communication: FDA revises label of diabetes drug canagliflozin (Invokana, Invokamet) to include updates on bone fracture risk and new information on decreased bone mineral density". FDA. U.S. Food & Drug Administration. Archived from the original on 15 September 2015. Retrieved 10 September 2015.
- ↑ "SGLT2 Inhibitors: Drug Safety Communication - Labels to Include Warnings About Too Much Acid in the Blood and Serious Urinary Tract Infections". FDA. Food and Drug Administration. Archived from the original on 16 March 2016. Retrieved 11 March 2016.
- ↑ Schroeder, C. "New Report Warns of Increasing SGLT2 & Invokana Risks". DrugNews. Pro Media One. Archived from the original on 14 August 2020. Retrieved 8 August 2016.
- ↑ "Press Release: FDA Confirms Increased Risk of Leg and Foot Amputations With Diabetes Medicine Canagliflozin". Fox Business. 2017-05-16. Archived from the original on 2018-02-15. Retrieved 2017-05-16.
- ↑ "FDA Drug Safety Communication: FDA confirms increased risk of leg and foot amputations with the diabetes medicine canagliflozin (Invokana, Invokamet, Invokamet XR)". FDA.gov. 2017-05-16. Archived from the original on 2017-05-28. Retrieved 2017-05-16.
- 1 2 "FDA revises labels of SGLT2 inhibitors for diabetes to include warning". U.S. Food and Drug Administration. 19 March 2020. Archived from the original on 7 June 2020. Retrieved 6 June 2020.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - ↑ Yamout H, Perkovic V, Davies M, Woo V, de Zeeuw D, Mayer C, Vijapurkar U, Kline I, Usiskin K, Meininger G, Bakris G (August 2014). "Efficacy and safety of canagliflozin in patients with type 2 diabetes and stage 3 nephropathy". American Journal of Nephrology. 40 (1): 64–74. doi:10.1159/000364909. PMID 25059406.
- ↑ Balis DA, Tong C, Meininger G (July 2014). "Effect of canagliflozin, a sodium-glucose cotransporter 2 inhibitor, on measurement of serum 1,5-anhydroglucitol". Journal of Diabetes. 6 (4): 378–80. doi:10.1111/1753-0407.12116. PMID 24330128.
- ↑ "Integrity - Clarivate". Archived from the original on 2007-11-05. Retrieved 2009-08-06.
- ↑ A. Klement (20 January 2014). "Tubuläre Senkung des Blutzuckers bei Diabetes mellitus: Invokana". Österreichische Apothekerzeitung (in German) (2/2014): 20f.
{{cite journal}}: CS1 maint: unrecognized language (link) - ↑ Drugs.com: Canagliflozin Monograph.
- ↑ "First Results from Phase 3 CANVAS Trial Show Canagliflozin as Add-on Therapy to Insulin Lowered Blood Sugar Levels in Patients with Type 2 Diabetes at an Elevated Risk for Cardiovascular Disease". Archived from the original on 2013-03-13. Retrieved 2013-02-21.
- ↑ "EMEA-001030-PIP01-10". EMA European Medicines Agency. Archived from the original on December 20, 2013. Retrieved May 6, 2013.
- ↑ "Canagliflozin". www.fda.gov. United States Food and Drug Administration. Retrieved 23 March 2016.
- ↑ "U.S. FDA approves Johnson & Johnson diabetes drug, canagliflozin". Reuters. March 29, 2013. Archived from the original on September 24, 2015. Retrieved June 30, 2017.
U.S. health regulators have approved a new diabetes drug from Johnson & Johnson, making it the first in its class to be approved in the United States.
External links
- "Canagliflozin". Drug Information Portal. U.S. National Library of Medicine. Archived from the original on 2020-06-07. Retrieved 2020-06-07.
| Identifiers: |
|---|