Tacrolimus
 | |
 | |
| Names | |
|---|---|
| Trade names | Prograf, Advagraf, Protopic, others |
| Other names | FK-506, fujimycin |
IUPAC name
| |
| Clinical data | |
| WHO AWaRe | UnlinkedWikibase error: ⧼unlinkedwikibase-error-statements-entity-not-set⧽ |
| Pregnancy category | |
| Routes of use | Topical, by mouth, intravenous |
| External links | |
| AHFS/Drugs.com | Systemic: Monograph Topical: Monograph |
| MedlinePlus | a601117 |
| Legal | |
| License data |
|
| Legal status |
|
| Pharmacokinetics | |
| Bioavailability | 24% (5–67%), less after eating food rich in fat |
| Protein binding | ≥98.8% |
| Metabolism | Liver CYP3A4, CYP3A5 |
| Elimination half-life | 11.3 h post transplant (range 3.5–40.6 h) |
| Excretion | Mostly faecal |
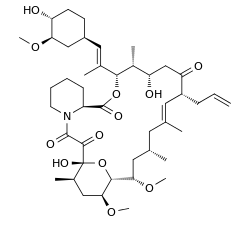
| Chemical and physical data | |
| Formula | C44H69NO12 |
| Molar mass | 804.018 g·mol−1 |
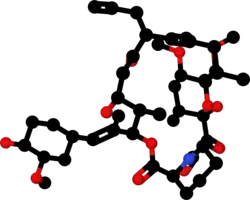
| 3D model (JSmol) | |
SMILES
| |
InChI
| |
Tacrolimus is a medication used by mouth or by injection to prevent rejection after organ transplant.[2][3] Levels of the medication should be regularly monitored.[3] As a cream it is used for moderate to severe eczema or psoriasis when other treatments are not sufficient.[2][4]
Common side effects when take by mouth or injection include kidney problems, diarrhea, nausea, high blood potassium, and infection.[5] Other side effects may include high blood sugar, neurological problems, lymphoma, and anaphylaxis.[3] Common side effects when used as a cream include itchiness, headache, and red skin.[4] It is unclear if the cream is safe in pregnancy.[6] Tacrolimus is a calcineurin inhibitor.[2] It is believed to works by decreasing the activity of T cells.[3]
Tacrolimus was discovered in 1987, and approved for medical use in the United States in 1994.[5] It is available as a generic medication.[7] It is on the World Health Organization's List of Essential Medicines.[8] In the United Kingdom 50 tablets of 5 mg costs the NHS about 206 pounds in 2020.[2] In the United States this amount costs about 82 USD as of 2020 while 30 grams of 0.1% cream costs about 36 USD.[7][9] It was initially made from a soil sample in Japan that contained the bacterium Streptomyces tsukubaensis.[10]
Medical uses
Organ transplantation
It has similar immunosuppressive properties to ciclosporin, but is much more potent. Immunosuppression with tacrolimus was associated with a significantly lower rate of acute rejection compared with ciclosporin-based immunosuppression (30.7% vs 46.4%) in one study.[11] Clinical outcome is better with tacrolimus than with ciclosporin during the first year of liver transplantation.[12][13] Long-term outcome has not been improved to the same extent. Tacrolimus is normally prescribed as part of a post-transplant cocktail including steroids, mycophenolate, and IL-2 receptor inhibitors such as basiliximab. Dosages are titrated to target blood levels.
Skin
As an ointment, tacrolimus is used in the treatment of eczema. It suppresses inflammation in a similar way to steroids, and is equally as effective as a mid-potency steroid. An important advantage of tacrolimus is that, unlike steroids, it does not cause skin thinning (atrophy).[14] Medical literature also points out that solitary mastocytoma can be treated with topical tacrolimus successfully[15]
 Solitary mastocytoma/cutaneous mastocytosis- Complete subsidence of the lesion with residual marginal pigmentation noted at the end of three months of therapy.The central atrophic scar due to biopsy can be seen in the centre of the lesion.
Solitary mastocytoma/cutaneous mastocytosis- Complete subsidence of the lesion with residual marginal pigmentation noted at the end of three months of therapy.The central atrophic scar due to biopsy can be seen in the centre of the lesion. Tacrolimus 0.1% ointment
Tacrolimus 0.1% ointment
Other
There is tentative evidence for tacrolimus in ulcerative colitis (UC).[16]
Tacrolimus has been shown to reduce the risk of serious infection in lupus nephritis, when compared to other agents.[17]
Dosage
The by mouth formulation is taken twice per day.[3] Levels of the medication should be regularly monitored.[3] The lower level of dosing is recommended in those with liver or kidney problems.[3]
Side effects
By mouth or intravenous
Contraindications and precautions include:[18]
- Breast-feeding
- Liver disease
- Immunosuppression
- Infants
- Infection
- Cancer such as:
- Oliguria
- Pregnancy
- QT interval prolongation
- Sunlight (UV) exposure
- Grapefruit juice[19]
Side effects can be severe and include infection, cardiac damage, hypertension, blurred vision, liver and kidney problems (tacrolimus nephrotoxicity),[20] hyperkalemia, hypomagnesemia, hyperglycemia, diabetes mellitus, itching, lung damage (sirolimus also causes lung damage),[21] and various neuropsychiatric problems such as loss of appetite, insomnia, posterior reversible encephalopathy syndrome, confusion, weakness, depression, vivid nightmares, cramps, neuropathy, seizures, tremors, and catatonia.[22]
In addition, it may potentially increase the severity of existing fungal or infectious conditions such as herpes zoster or polyoma viral infections.[18]
Cancer
In people receiving immunosuppressants to reduce transplant graft rejection, an increased risk of malignancy (cancer) is a recognised complication.[18] The most common cancers are non-Hodgkin's lymphoma[23] and skin cancers. The risk appears to be related to the intensity and duration of treatment.
Topical
It is not recommended with
- Occlusive dressing
- Known or suspected skin cancer
- Netherton's syndrome or similar skin diseases
- Certain skin infections[14]
The most common side effects associated with the use of topical tacrolimus ointments, especially if used over a wide area, include a burning or itching sensation on the initial applications, with increased sensitivity to sunlight and heat on the affected areas. Less common are flu-like symptoms, headache, cough, and burning eyes.[24]
Cancer
Tacrolimus and a related drug for eczema (pimecrolimus) were suspected of carrying a cancer risk, though the matter is still a subject of controversy. The FDA issued a health warning in March 2005 for the drug, based on animal models and a small number of patients. Until further human studies yield more conclusive results, the FDA recommends that users be advised of the potential risks. However, current practice by UK dermatologists is not to consider this a significant real concern and they are increasingly recommending the use of these new drugs.[25]
Interactions
Also like cyclosporin, it has a wide range of interactions. Tacrolimus is primarily metabolised by the cytochrome P450 system of liver enzymes, and there are many substances that interact with this system and induce or inhibit the system's metabolic activity.[18]
Interactions include that with grapefruit which increases tacrolimus plasma concentrations. As infections are a major cause of morbidity and mortality in the post-transplant patient, the most commonly reported interactions include interactions with anti-microbial drugs. Macrolide antibiotics including erythromycin and clarithromycin, as well as several of the newer classes of antifungals, especially of the azole class (fluconazole, voriconazole), increase tacrolimus levels by competing for cytochrome enzymes.[18]
Pharmacology
Mechanism of action
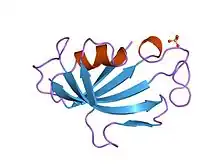
Tacrolimus is a macrolide calcineurin inhibitor. In T-cells, activation of the T-cell receptor normally increases intracellular calcium, which acts via calmodulin to activate calcineurin. Calcineurin then dephosphorylates the transcription factor nuclear factor of activated T-cells (NF-AT), which moves to the nucleus of the T-cell and increases the activity of genes coding for IL-2 and related cytokines. Tacrolimus prevents the dephosphorylation of NF-AT.[26]
In detail, tacrolimus reduces peptidylprolyl isomerase activity by binding to the immunophilin FKBP12 (FK506 binding protein), creating a new complex. This FKBP12–FK506 complex interacts with and inhibits calcineurin, thus inhibiting both T-lymphocyte signal transduction and IL-2 transcription.[27] Although this activity is similar to that of cyclosporin, the incidence of acute rejection is reduced by tacrolimus use over cyclosporin use.[11] Although short-term immunosuppression concerning patient and graft survival is found to be similar between the two drugs, tacrolimus results in a more favorable lipid profile, and this may have important long-term implications given the prognostic influence of rejection on graft survival.[28]
Pharmacokinetics
Oral tacrolimus is slowly absorbed in the gastrointestinal tract, with a total bioavailability of 20 to 25% (but with variations from 5 to 67%) and highest blood plasma concentrations (Cmax) reached after one to three hours. Taking the drug together with a meal, especially one rich in fat, slows down resorption and reduces bioavailability. In the blood, tacrolimus is mainly bound to erythrocytes; only 5% are found in the plasma, of which more than 98.8% are bound to plasma proteins.[18][29]
The substance is metabolized in the liver, mainly via CYP3A, and in the intestinal wall. All metabolites found in the circulation are inactive. Biological half-life varies widely and seems to be higher for healthy persons (43 hours on average) than for patients with liver transplants (12 hours) or kidney transplants (16 hours), due to differences in clearance. Tacrolimus is predominantly eliminated via the faeces in form of its metabolites.[18][29]
When applied locally on eczema, tacrolimus has little to no bioavailability.[18]
Pharmacogenetics
The predominant enzyme responsible for metabolism of tacrolimus is CYP3A5. Genetic variations within CYP3A5 that result in changes to the activity of the CYP3A5 protein can affect concentrations of tacrolimus within the body. In particular, individuals who are homozygous for the G allele at the single nucleotide polymorphism (SNP) rs776746 (also known as CYP3A5 *3/*3) have a non-functional CYP3A5 protein. The frequency of the G allele varies worldwide, from 4% in some African populations to 80–90% in Caucasian populations.[30] Across a large number of studies, individuals homozygous for the G allele have been shown to have higher concentrations of tacrolimus and require lower doses of the drug, as compared to individuals who are not homozygous for the G allele. Achieving target concentrations of tacrolimus is important – if levels are too low, then there is a risk of transplant rejection, if levels are too high, there is a risk of drug toxicities. There is evidence to suggest that dosing patients based on rs776746 genotype can result in faster and more frequent achievement of target tacrolimus levels. However, there is a lack of consistent evidence as to whether dosing based on rs776746 genotype results in improved clinical outcomes (such as a decreased risk for transplant rejection or drug toxicities), likely because patients taking tacrolimus are subject to therapeutic drug monitoring.[31][32][33][34]
Studies have shown that genetic polymorphisms of genes other than CYP3A5, such as NR1I2[35][36] (encoding PXR), also significantly influence the pharmacokinetics of tacrolimus.
History
Tacrolimus was discovered in 1987;[37] it was among the first macrolide immunosuppressants discovered, preceded by the discovery of rapamycin (sirolimus) on Rapa Nui (Easter Island) in 1975.[38] It is produced by a soil bacterium, Streptomyces tsukubaensis.[39] The name tacrolimus is derived from "Tsukuba macrolide immunosuppressant".[40]
Tacrolimus was first approved by the US Food and Drug Administration (FDA) in 1994,[41][42] for use in liver transplantation; the indications were extended to include kidney, heart, small bowel, pancreas, lung, trachea, skin, cornea, bone marrow, and limb transplants. Generic versions of tacrolimus were approved in the US in 2017.[43]
Tacrolimus was approved for medical use in the European Union in 2002, for the treatment of moderate to severe atopic dermatitis.[44] In 2007, the indications were expanded to include the prophylaxis of transplant rejection in adult kidney or liver allograft recipients and the treatment of allograft rejection resistant to treatment with other immunosuppressive medicinal products in aduls.[45] In 2009, the indications were expanded to include the prophylaxis of transplant rejection in adult and paediatric, kidney, liver or heart allograft recipients and the treatment of allograft rejection resistant to treatment with other immunosuppressive medicinal products in adults and children.[46]
Society and culture
Cost
The oral capsule for this medication of 1 mg is about $124 for 100 capsules[47]
.svg.png.webp) Tacrolimus costs (US)
Tacrolimus costs (US).svg.png.webp) Tacrolimus prescriptions (US)
Tacrolimus prescriptions (US)
Available forms
A branded version of the drug is owned by Astellas Pharma, and is sold under the brand name Prograf, given twice daily. A number of other manufacturers hold marketing authorisation for alternative brands of the twice-daily formulation.[48]
Once-daily formulations with marketing authorisation include Advagraf (Astellas Pharma) and Envarsus (marketed as Envarsus XR in US by Veloxis Pharmaceuticals and marketed in Europe by Chiesi).[48] These formulations are intended to reduce pharmacokinetic variation in blood levels and facilitate compliance with dosing.
The topical formulation is marketed by LEO Pharma under the name Protopic.[48]
Biosynthesis
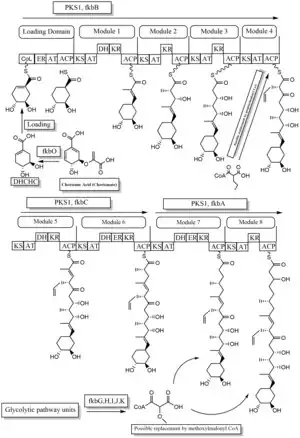
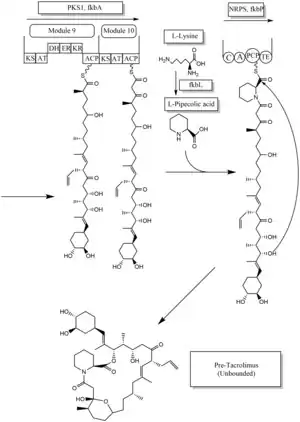
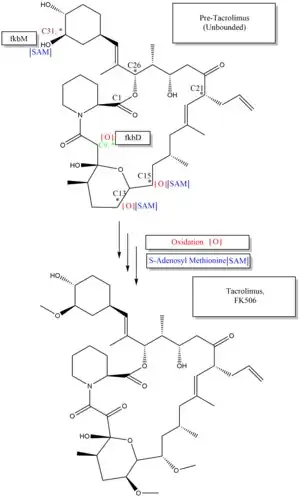
The biosynthesis of tacrolimus is hybrid synthesis of both type 1 polyketide synthases (PKS 1) and nonribosomal peptide synthases (NRPS). The research shows the hybrid synthesis consists of ten modules of type 1 polyketide synthase and one module of nonribosomal peptide synthase. The synthetic enzymes for tacrolimus are found in 19 gene clusters named fkb. The 19 genes are fkbQ, fkbN, fkbM, fkbD, fkbA, fkbP, fkbO, fkbB, fkbC, fkbL, fkbK, fkbJ, fkbI, fkbH, fkbG, allD, allR, allK and allA.[49]
There are several possible ways of biosynthesis of tacrolimus. The fundamental units for biosynthesis are following: one molecule of 4,5-dihydroxycyclohex-1-enecarboxylic acid (DHCHC) as a starter unit, four molecules of malonyl-CoA, five molecules of methylmalonyl-CoA, one molecule of allylmalonyl-CoA as elongation units. However, two molecules of malonyl-CoA are able to be replaced by two molecules of methoxymalonyl CoA. Once two malonyl-CoA molecules are replaced, post-synthase tailoring steps are no longer required where two methoxymalonyl CoA molecules are substituted. The biosynthesis of methoxymalonyl CoA to Acyl Carrier protein is proceeded by five enzymes (fkbG, fkbH, fkbI, fkbJ, and fkbK). Allylmalonyl-CoA is also able to be replaced by propionylmalonyl-CoA.[49]
The starter unit, DHCHC from the chorismic acid is formed by fkbO enzyme and loaded onto CoA-ligase domain (CoL). Then, it proceeds to NADPH dependent reduction(ER). Three enzymes, fkbA,B,C enforce processes from the loading module to the module 10, the last step of PKS 1. fkbB enzyme is responsible of allylmalonyl-CoA synthesis or possibly propionylmalonyl-CoA at C21, which it is an unusual step of general PKS 1. As mentioned, if two methoxymalonyl CoA molecules are substituted for two malonyl-CoA molecules, they will take place in module 7 and 8 (C13 and C15), and fkbA enzyme will enforce this process. After the last step (module 10) of PKS 1, one molecule of L-pipecolic acid formed from L-lysine and catalyzed through fkbL enzyme synthesizes with the molecule from the module 10. The process of L-pipecolic acid synthesis is NRPS enforced by fkbP enzyme. After synthesizing the entire subunits, the molecule is cyclized. After the cyclization, the pre-tacrolimus molecule goes through the post-synthase tailoring steps such as oxidation and S-adenosyl methionine. Particularly fkbM enzyme is responsible of alcohol methylation targeting the alcohol of DHCHC starter unit (Carbon number 31 depicted in brown), and fkbD enzyme is responsible of C9 (depicted in green). After these tailoring steps, the tacrolimus molecule becomes biologically active.[49][50][51]
Other animals
It is used to treat dry eye syndrome in cats and dogs.[52][53]
See also
- Tohru Kino
- Stuart Schreiber
- Thomas Starzl
- FK1012, a derivative
- Ciclosporin
References
- 1 2 "Tacrolimus Use During Pregnancy". Drugs.com. 3 October 2019. Archived from the original on 7 August 2020. Retrieved 29 April 2020.
- 1 2 3 4 BNF 79 : March 2020. London: Royal Pharmaceutical Society. 2020. p. 868. ISBN 9780857113658.
- 1 2 3 4 5 6 7 "Tacrolimus Monograph for Professionals". Drugs.com. Archived from the original on 7 August 2020. Retrieved 12 October 2020.
- 1 2 "Tacrolimus topical Monograph for Professionals". Drugs.com. Archived from the original on 6 May 2021. Retrieved 12 October 2020.
- 1 2 "Tacrolimus Monograph for Professionals". Drugs.com. Archived from the original on 7 August 2020. Retrieved 12 October 2020.
- ↑ "Tacrolimus topical (Protopic) Use During Pregnancy". Drugs.com. Archived from the original on 3 December 2020. Retrieved 12 October 2020.
- 1 2 "Tacrolimus Prices, Coupons & Savings Tips". GoodRx. Retrieved 12 October 2020.
- ↑ World Health Organization (2021). World Health Organization model list of essential medicines: 22nd list (2021). Geneva: World Health Organization. hdl:10665/345533. WHO/MHP/HPS/EML/2021.02.
- ↑ "Tacrolimus Prices and Tacrolimus Coupons". GoodRx. Archived from the original on 22 July 2020. Retrieved 12 October 2020.
- ↑ Chakravarty, Dilip; Chakravarty, Dilip K.; Lee, W. C. (2010). Liver Transplantation. Boydell & Brewer Ltd. p. 169. ISBN 978-81-8448-770-1. Archived from the original on 29 August 2021. Retrieved 12 October 2020.
- 1 2 McCauley, Jerry (19 May 2004). "Long-Term Graft Survival In Kidney Transplant Recipients". Slide Set Series on Analyses of Immunosuppressive Therapies. Medscape. Archived from the original on 7 March 2011. Retrieved 6 June 2006.
- ↑ Haddad EM, McAlister VC, Renouf E, Malthaner R, Kjaer MS, Gluud LL (October 2006). McAlister V (ed.). "Cyclosporin versus tacrolimus for liver transplanted patients". The Cochrane Database of Systematic Reviews. 4 (4): CD005161. doi:10.1002/14651858.CD005161.pub2. PMID 17054241. Archived from the original on 11 January 2020. Retrieved 6 February 2011.
- ↑ O'Grady JG, Burroughs A, Hardy P, Elbourne D, Truesdale A (October 2002). "Tacrolimus versus microemulsified ciclosporin in liver transplantation: the TMC randomised controlled trial". Lancet. 360 (9340): 1119–25. doi:10.1016/S0140-6736(02)11196-2. PMID 12387959.
- 1 2 Haberfeld, H, ed. (2015). Austria-Codex (in German). Vienna: Österreichischer Apothekerverlag. Protopic.
{{cite book}}: CS1 maint: unrecognized language (link) - ↑ El-Darouti, Mohammad Ali; Al-Ali, Faiza Mohamed (28 August 2019). Challenging Cases in Dermatology Volume 2: Advanced Diagnoses and Management Tactics. Springer Nature. p. 46. ISBN 978-3-030-21855-3. Archived from the original on 22 September 2021. Retrieved 19 September 2021.
- ↑ Baumgart DC, Macdonald JK, Feagan B (July 2008). Baumgart DC (ed.). "Tacrolimus (FK506) for induction of remission in refractory ulcerative colitis". The Cochrane Database of Systematic Reviews. 16 (3): CD007216. doi:10.1002/14651858.CD007216. PMID 18646177.
- ↑ Singh JA, Hossain A, Kotb A, Wells G (September 2016). "Risk of serious infections with immunosuppressive drugs and glucocorticoids for lupus nephritis: a systematic review and network meta-analysis". BMC Medicine. 14 (1): 137. doi:10.1186/s12916-016-0673-8. PMC 5022202. PMID 27623861.
- 1 2 3 4 5 6 7 8 Haberfeld, H, ed. (2015). Austria-Codex (in German). Vienna: Österreichischer Apothekerverlag. Prograf.
{{cite book}}: CS1 maint: unrecognized language (link) - ↑ Fukatsu S, Fukudo M, Masuda S, Yano I, Katsura T, Ogura Y, Oike F, Takada Y, Inui K (April 2006). "Delayed effect of grapefruit juice on pharmacokinetics and pharmacodynamics of tacrolimus in a living-donor liver transplant recipient". Drug Metabolism and Pharmacokinetics. 21 (2): 122–5. doi:10.2133/dmpk.21.122. PMID 16702731.
- ↑ Naesens M, Kuypers DR, Sarwal M (February 2009). "Calcineurin inhibitor nephrotoxicity" (PDF). Clinical Journal of the American Society of Nephrology. 4 (2): 481–508. doi:10.2215/CJN.04800908. PMID 19218475. Archived (PDF) from the original on 20 July 2018. Retrieved 20 April 2018.
- ↑ Miwa Y, Isozaki T, Wakabayashi K, Odai T, Matsunawa M, Yajima N, Negishi M, Ide H, Kasama T, Adachi M, Hisayuki T, Takemura T (2008). "Tacrolimus-induced lung injury in a rheumatoid arthritis patient with interstitial pneumonitis". Modern Rheumatology. 18 (2): 208–11. doi:10.1007/s10165-008-0034-3. PMID 18306979.
- ↑ O'Donnell MM, Williams JP, Weinrieb R, Denysenko L (2007). "Catatonic mutism after liver transplant rapidly reversed with lorazepam". General Hospital Psychiatry. 29 (3): 280–1. doi:10.1016/j.genhosppsych.2007.01.004. PMID 17484951.
- ↑ "Key Statistics for Non-Hodgkin Lymphoma". www.cancer.org. Archived from the original on 24 August 2019. Retrieved 19 February 2020.
- ↑ Hanifin JM, Paller AS, Eichenfield L, Clark RA, Korman N, Weinstein G, Caro I, Jaracz E, Rico MJ (August 2005). "Efficacy and safety of tacrolimus ointment treatment for up to 4 years in patients with atopic dermatitis". Journal of the American Academy of Dermatology. 53 (2 Suppl 2): S186–94. doi:10.1016/j.jaad.2005.04.062. PMID 16021174.
- ↑ N H Cox; Catherine H Smith (December 2002). "Advice to dermatologists re topical tacrolimus" (PDF). Therapy Guidelines Committee. British Association of Dermatologists. Archived from the original (PDF) on 13 December 2013.
- ↑ William F. Ganong (8 March 2005). Review of medical physiology (22nd ed.). Lange medical books. p. 530. ISBN 978-0-07-144040-0.
- ↑ Liu J, Farmer JD, Lane WS, Friedman J, Weissman I, Schreiber SL (August 1991). "Calcineurin is a common target of cyclophilin-cyclosporin A and FKBP-FK506 complexes". Cell. 66 (4): 807–15. doi:10.1016/0092-8674(91)90124-H. PMID 1715244.
- ↑ Abou-Jaoude MM, Najm R, Shaheen J, Nawfal N, Abboud S, Alhabash M, Darwish M, Mulhem A, Ojjeh A, Almawi WY (September 2005). "Tacrolimus (FK506) versus cyclosporine microemulsion (neoral) as maintenance immunosuppression therapy in kidney transplant recipients". Transplantation Proceedings. 37 (7): 3025–8. doi:10.1016/j.transproceed.2005.08.040. PMID 16213293.
- 1 2 Dinnendahl, V; Fricke, U, eds. (2003). Arzneistoff-Profile (in German). Vol. 9 (18 ed.). Eschborn, Germany: Govi Pharmazeutischer Verlag. ISBN 978-3-7741-9846-3.
{{cite book}}: CS1 maint: unrecognized language (link) - ↑ Bains, Ripudaman Kaur. "Molecular diversity and population structure at the CYP3A5 gene in Africa" (PDF). University College London. Archived (PDF) from the original on 22 October 2015. Retrieved 13 June 2016.
- ↑ Staatz CE, Tett SE (2004). "Clinical pharmacokinetics and pharmacodynamics of tacrolimus in solid organ transplantation". Clinical Pharmacokinetics. 43 (10): 623–53. doi:10.2165/00003088-200443100-00001. PMID 15244495.
- ↑ Staatz CE, Goodman LK, Tett SE (March 2010). "Effect of CYP3A and ABCB1 single nucleotide polymorphisms on the pharmacokinetics and pharmacodynamics of calcineurin inhibitors: Part I". Clinical Pharmacokinetics. 49 (3): 141–75. doi:10.2165/11317350-000000000-00000. PMID 20170205.
- ↑ Staatz CE, Goodman LK, Tett SE (April 2010). "Effect of CYP3A and ABCB1 single nucleotide polymorphisms on the pharmacokinetics and pharmacodynamics of calcineurin inhibitors: Part II". Clinical Pharmacokinetics. 49 (4): 207–21. doi:10.2165/11317550-000000000-00000. PMID 20214406.
- ↑ Barbarino JM, Staatz CE, Venkataramanan R, Klein TE, Altman RB (October 2013). "PharmGKB summary: cyclosporine and tacrolimus pathways". Pharmacogenetics and Genomics. 23 (10): 563–85. doi:10.1097/fpc.0b013e328364db84. PMC 4119065. PMID 23922006.
- ↑ Benkali K, Prémaud A, Picard N, Rérolle JP, Toupance O, Hoizey G, Turcant A, Villemain F, Le Meur Y, Marquet P, Rousseau A (1 January 2009). "Tacrolimus population pharmacokinetic-pharmacogenetic analysis and Bayesian estimation in renal transplant recipients". Clinical Pharmacokinetics. 48 (12): 805–16. doi:10.2165/11318080-000000000-00000. PMID 19902988.
- ↑ Choi Y, Jiang F, An H, Park HJ, Choi JH, Lee H (January 2017). "A pharmacogenomic study on the pharmacokinetics of tacrolimus in healthy subjects using the DMETTM Plus platform". The Pharmacogenomics Journal. 17 (1): 105–106. doi:10.1038/tpj.2016.85. PMID 27958377.
- ↑ Hatanaka H, Iwami M, Kino T, Goto T, Okuhara M (November 1988). "FR-900520 and FR-900523, novel immunosuppressants isolated from a Streptomyces. I. Taxonomy of the producing strain". The Journal of Antibiotics. 41 (11): 1586–91. doi:10.7164/antibiotics.41.1586. PMID 3198493.
- ↑ Kino T, Hatanaka H, Hashimoto M, Nishiyama M, Goto T, Okuhara M, Kohsaka M, Aoki H, Imanaka H (September 1987). "FK-506, a novel immunosuppressant isolated from a Streptomyces. I. Fermentation, isolation, and physico-chemical and biological characteristics". The Journal of Antibiotics. 40 (9): 1249–55. doi:10.7164/antibiotics.40.1249. PMID 2445721.
- ↑ Pritchard DI (May 2005). "Sourcing a chemical succession for cyclosporin from parasites and human pathogens". Drug Discovery Today. 10 (10): 688–91. doi:10.1016/S1359-6446(05)03395-7. PMID 15896681. Supports source organism, but not team information
- ↑ Ponner, B, Cvach, B (Fujisawa Pharmaceutical Co.): Protopic Update 2005
- ↑ "Prograf: FDA-Approved Drugs". U.S. Food and Drug Administration (FDA). Archived from the original on 7 August 2020. Retrieved 29 April 2020.
- ↑ "Prograf: FDA-Approved Drugs". U.S. Food and Drug Administration (FDA). Archived from the original on 7 August 2020. Retrieved 29 April 2020.
- ↑ "Tacrolimus: FDA-Approved Drugs". U.S. Food and Drug Administration (FDA). Archived from the original on 7 August 2020. Retrieved 29 April 2020.
- ↑ "Protopic EPAR". European Medicines Agency (EMA). Archived from the original on 7 August 2020. Retrieved 29 April 2020.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - ↑ "Advagraf EPAR". European Medicines Agency (EMA). Archived from the original on 7 August 2020. Retrieved 29 April 2020.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - ↑ "Modigraf EPAR". European Medicines Agency (EMA). Archived from the original on 3 August 2020. Retrieved 29 April 2020.
- ↑ "Tacrolimus Prices, Coupons & Patient Assistance Programs". Drugs.com. Archived from the original on 8 December 2015. Retrieved 19 March 2021.
- 1 2 3 Joint Formulary Committee. "British National Formulary (online)". London: BMJ Group and Pharmaceutical Press. Archived from the original on 10 June 2021. Retrieved 24 September 2015.
- 1 2 3 Ordóñez-Robles M, Santos-Beneit F, Martín JF (May 2018). "omic Approaches". Antibiotics. 7 (2): 39. doi:10.3390/antibiotics7020039. PMC 6022917. PMID 29724001.
- ↑ Chen D, Zhang L, Pang B, Chen J, Xu Z, Abe I, Liu W (May 2013). "FK506 maturation involves a cytochrome p450 protein-catalyzed four-electron C-9 oxidation in parallel with a C-31 O-methylation". Journal of Bacteriology. 195 (9): 1931–9. doi:10.1128/JB.00033-13. PMC 3624582. PMID 23435975.
- ↑ Mo S, Ban YH, Park JW, Yoo YJ, Yoon YJ (December 2009). "Enhanced FK506 production in Streptomyces clavuligerus CKD1119 by engineering the supply of methylmalonyl-CoA precursor". Journal of Industrial Microbiology & Biotechnology. 36 (12): 1473–82. doi:10.1007/s10295-009-0635-7. PMID 19756799.
- ↑ Berdoulay A, English RV, Nadelstein B (2005). "Effect of topical 0.02% tacrolimus aqueous suspension on tear production in dogs with keratoconjunctivitis sicca". Veterinary Ophthalmology. 8 (4): 225–32. doi:10.1111/j.1463-5224.2005.00390.x. PMID 16008701.
- ↑ "Tacrolimus for Dogs and Cats". Archived from the original on 27 September 2018. Retrieved 26 September 2018.
Further reading
- Lv X, Qi J, Zhou M, et al. (March 2020). "Comparative efficacy of 20 graft-versus-host disease prophylaxis therapies for patients after hematopoietic stem-cell transplantation: A multiple-treatments network meta-analysis". Crit. Rev. Oncol. Hematol. 150: 102944. doi:10.1016/j.critrevonc.2020.102944. PMID 32247246.
External links
| Identifiers: |
|---|
- "Tacrolimus". Drug Information Portal. U.S. National Library of Medicine. Archived from the original on 7 August 2020. Retrieved 29 April 2020.
- "Tacrolimus Injection". MedlinePlus. Archived from the original on 7 August 2020. Retrieved 29 April 2020.
- "Tacrolimus Topical". MedlinePlus. Archived from the original on 19 March 2021. Retrieved 29 April 2020.
- Tacrolimus at the US National Library of Medicine Medical Subject Headings (MeSH)