Estradiol benzoate/estradiol phenylpropionate
 | |
 | |
| Combination of | |
|---|---|
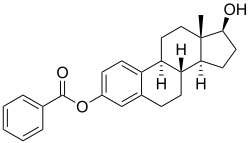
| Estradiol benzoate | Estrogen |
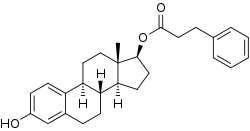
| Estradiol phenylpropionate | Estrogen |
| Clinical data | |
| Trade names | Dimenformon Prolongatum |
| Other names | EB/EPP; Org 369-2 |
| Routes of administration | Intramuscular injection |
| Identifiers | |
| CAS Number | |
| PubChem CID | |
| ChemSpider | |
| UNII | |
Estradiol benzoate/estradiol phenylpropionate (EB/EPP), sold under the brand name Dimenformon Prolongatum, is an injectable combination formulation of estradiol benzoate (EB), a shorter-acting estrogen, and estradiol phenylpropionate (EPP), a longer-acting estrogen, which has been used in menopausal hormone therapy for women in Europe but appears to no longer be available.[1][2][3][4] It has also been used to suppress lactation in women and has been used in feminizing hormone therapy for transgender women.[5][6] It has been provided in the form of 1 mL ampoules containing 2.5 mg EB and 10 mg EPP in oil solution and is administered by intramuscular injection at regular intervals.[2]
The pharmacokinetics of this formulation and its constituent components have been studied.[7][8][9][10][11][12]
A combination of 12.5 mg EB and 10 mg EPP (developmental code name Org 369–2) has been studied for use in women as a postcoital contraceptive within 48 hours of unprotected sex.[13][9][14][15][16]
See also
References
- ↑ Index Nominum 2000: International Drug Directory. Taylor & Francis. 2000. pp. 406–. ISBN 978-3-88763-075-1.
- 1 2 Muller (19 June 1998). European Drug Index: European Drug Registrations, Fourth Edition. CRC Press. pp. 370–. ISBN 978-3-7692-2114-5.
- ↑ https://www.micromedexsolutions.com/
- ↑ "Estradiol: Uses, Dosage & Side Effects".
- ↑ Leleux D, Merveille JJ, Capel P, Picard C, L'Hermite M (October 1981). "Bromocriptine compared to long-acting estrogens in lactation prevention: clinical efficacy, prolactin secretion and coagulation parameters" (PDF). Eur. J. Obstet. Gynecol. Reprod. Biol. 12 (4): 235–42. doi:10.1016/0028-2243(81)90014-9. PMID 7197648.
- ↑ Imbimbo, Ciro; Arcaniolo, Davide (2015). "Male-to-Female Transsexualism". Clinical Uro-Andrology. pp. 15–28. doi:10.1007/978-3-662-45018-5_2. ISBN 978-3-662-45017-8.
Table 2.2 Guidelines on hormone therapy [...] Presurgical A.2.: Induction of designated sex characteristics [...] estradiol benzoate, estradiol phenylpropionate (25 mg/2 weeks) [...]
- ↑ Rauramo L, Punnonen R, Kaihola LH, Grönroos M (January 1980). "Serum oestrone, oestradiol and oestriol concentrations in castrated women during intramuscular oestradiol valerate and oestradiolbenzoate-oestradiolphenylpropionate therapy". Maturitas. 2 (1): 53–8. doi:10.1016/0378-5122(80)90060-2. PMID 7402086.
- ↑ Rauramo L, Punnonen R, Grönroos M (August 1981). "Serum concentrations of oestrone, oestradiol and oestriol during various oestrogen treatments". Maturitas. 3 (2): 183–6. doi:10.1016/0378-5122(81)90010-4. PMID 7289888.
- 1 2 Haspels AA, Linthorst GA, Kicovic PM (January 1977). "Effect of postovulatory administration of a "morning-after" injection on corpus luteum function and endometrium". Contraception. 15 (1): 105–12. doi:10.1016/0010-7824(77)90042-7. PMID 880800.
- ↑ Kaiser R (September 1961). "Die Östrogenausscheidung im Zyklus und nach Injektion von Östradiolestern" [Estrogen excretion during the cycle and after injection of estradiol esters. A contribution to therapy with depot estrogens]. Geburtshilfe Frauenheilkd (in German). 21: 868–78. PMID 13750804.
- ↑ Kaiser, R (1962). "Über die Oestrogenausscheidung nach Injektion von Oestradiolestern" [Estrogen excretion after injection of estradiol esters]. Gewebs-und Neurohormone: Physiologie des Melanophorenhormons [Tissue and Neurohormones: Physiology of the Melanophore Hormone]. Springer, Berlin, Heidelberg. pp. 227–232. doi:10.1007/978-3-642-86860-3_24. ISBN 978-3-540-02909-0.
- ↑ Vermeulen A (1975). "Longacting steroid preparations". Acta Clin Belg. 30 (1): 48–55. doi:10.1080/17843286.1975.11716973. PMID 1231448.
- ↑ Marcus Filshie; John Guillebaud (22 October 2013). Contraception: Science and Practice. Elsevier Science. pp. 128–. ISBN 978-1-4831-6366-6.
- ↑ Schindler AE, Keller E, Göser R, Barlas P, Friedrich E (July 1977). "Postcoitale Kontrazeption mit einem hochdosierten Depotöstrogen (Org 369-2)" [Postcoital contraception using a high-dose depot estrogen (Org 369-2)]. Arch Gynakol (in German). 224 (1–4): 29. doi:10.1007/BF00679421. ISSN 0003-9128. PMID 579823. S2CID 36220628.
A combination of 12.5 mg estradiol benzoate and 10 mg estradiol phenylpropionate was used for postcoital contraception in 60 women. Treatment occurred within 48 hours of unprotected coitus in almost all cases, and generally between the 10th and 18th days of the cycle. Plasma luteinizing hormone, follicle-stimulating hormone, prolactin, estradiol, and progesterone were determined before and 8 days after treatment, and after the following menstruation. Few side effects were observed. Cycle length and duration of menstruation were not greatly changed. In 7 women plasma progesterone levels were above 5 ng/ml before treatment, while in 35 others they were below 1 ng. In about one-third of the women, plasma progesterone was below 1 ng/ml in both determinations, indicating anovulatory cycles. It is impossible to determine whether the estrogen medication was responsible for these. Since 3 pregnancies were observed in the group, the effectiveness of this treatment is questionable.
- ↑ Haspels AA; Coelingh Bennink HJ; van der Steeg HJ (1978). "Recent findings of research on hormonal contraception, 1. Interception: the use of post-coital oestrogens.". International Symposium on Hormonal Contraception. (Proceedings of a Symposium, Utrecht, The Netherlands, September 10, 1977). Amsterdam-Oxford, Excerpta Medica. pp. 68–71.
With respect to morning-after injection, 150 volunteers given 12.5 mg estradiol benzoate and 10 mg of estradiol phenylpropionate exhibited very low frequency of side effects; however, 4 pregnancies, considered to be method-failures, were observed. Endometrial biopsy and histological examination showed pronounced local epithelial proliferation in 3 cases. Recordings of post-ovulatory basal body temperature showed a consistent pattern, possibly due to the low dosage used. These results suggest immediate treatment with the indicated dosage levels after unprotected intercourse may be effective especially in emergency cases such as failure of other contraceptive methods, unexpected intercourse and rape.
- ↑ Schindler AE, Ladanyi S, Göser R, Keller E (August 1980). "Postcoital contraception with an injectable estrogen preparation (Org 369 - 2)". Contraception. 22 (2): 165–74. doi:10.1016/0010-7824(80)90060-8. PMID 6778652.