Darier disease
| Darier's disease | |
|---|---|
| Other names: Darier disease, Darier–White disease,[1] Dyskeratosis follicularis,[1] and Keratosis follicularis[2] | |
 | |
| Linear Darier's disease | |
Darier disease (DAR) is an inherited skin disorder that presents with multiple greasy, crusting, thick brown bumps that merge into patches.[3][4][5] It is characterized by dark crusty patches on the skin that are mildly greasy and that emit a strong odor. These patches, also known as keratotic papules, keratosis follicularis, or dyskeratosis follicularis, most often appear on the scalp, forehead, upper arms, chest, back, knees, elbows, and behind the ear.[6][7]
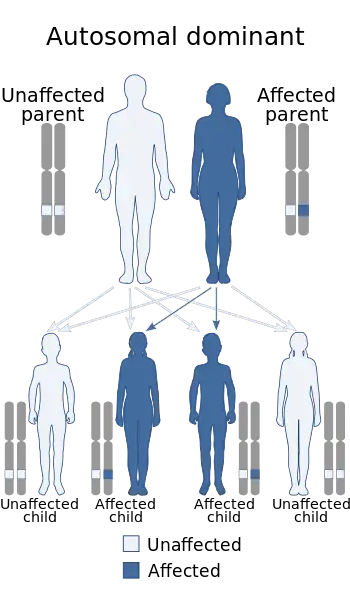
Darier disease is autosomal dominant.[4]
The French dermatologist Ferdinand-Jean Darier described the first case.[2]
Signs and symptoms
Mild forms of the disease are the most common, consisting solely of skin rashes that flare up under certain conditions such as high humidity, high stress, or tight-fitting clothes. Short stature, when combined with poorly-formed fingernails that contain vertical striations, is diagnostic even for mild forms of DAR. Symptoms will usually appear in late childhood or early adulthood between the ages of 15 to 30 years and will vary over the course of one’s life.
- Clinical symptoms that are often seen in the presentation of the disease:
- Seborrhoeic areas
- This is defined as areas where excess oil and sebum is released.
- Overall greasy or scaly skin either in the central chest and back or in the folds of the skin.
- Fragile or poorly formed fingernails
- Nail disease leading to V-shaped nicks at the edge of the nail.
- Rash that covers many areas of the body
- The rash is often associated with a strong unpleasant odor
- The rash can be aggravated by heat, humidity, and exposure to sunlight.
- Mucosal manifestation
- White cobblestone pattern of small papules
- Overgrowth of gums
- Usually affects the mouth, esophagus, rectum, vulva, vagina
- Oral symptoms can be diagnosed by a routine dental examination
- Seborrhoeic areas
- Other symptoms and their overall prevalence in the affected population:[8]
- In 80-90% of patients
- Acrokeratosis Verruciformis[9]
- Acrokeratosis is characterized by several small wart-like and flat-topped bumps that line the skin on typically the hand and feet.[10]
- Hypermelanotic macule
- Patches on the skin that contain excess pigment, they often appear as dark patches in the skin.
- Pruritus
- Itching
- Subungual hyperkeratotic fragments
- Thickened skin that is often discolored, under nails, on either hands or feet.
- Palmar pits
- Usually red in color, they are pits or depressions in the palms or soles of the hands and feet.
- Acrokeratosis Verruciformis[9]
- In 30-79% of patients
- Abnormal hair morphology
- Acne Conglobata
- Typically described as cystic acne
- In 80-90% of patients
Genetics
Mutations in a single gene, ATP2A2, are responsible for the development of Darier’s disease. ATP2A2 encodes the SERCA2 protein, which is a calcium pump localized to the membranes of the endoplasmic reticulum (ER) in nearly all cells and the sarcoplasmic reticulum (SR) in muscle cells. The ER is where protein processing and transport begins for proteins targeted for secretion. The SR is a specialized form of ER found in muscle cells that sequesters calcium, the regulated efflux of which into the cytosol stimulates muscle fiber contraction. Calcium acts as a second messenger in many cellular signal transduction pathways. SERCA2 is required for Ca2+ signaling in cells by removing nearly all Ca2+ ions from the cytoplasm and storing them in the ER/SR compartments.[11][12][13][14]
A large number of mutant alleles of ATP2A2 have been identified in association with Darier’s Disease. One study of 19 families and 6 sporadic cases found 24 specific, novel mutations associated with DAR symptoms. This study reported a loose, imperfect correlation between the severity of ATP2A2 mutations with the severity of the condition. Significant variability in disease severity between members of the same family carrying the same mutation was also reported by this study, suggesting that genetic modifiers contribute to the phenotypic penetrance of certain mutations.[15]
The mutation is inherited in an autosomal dominant pattern. This means that only one allele needs to be mutated in order to express the trait. This also means that someone who is born to one parent with DAR has a 50% chance of inheriting the mutant allele and having the disease. Loss-of-function mutations typically display recessive inheritance while the gain-of-function or hyperactive function of proteins is characteristic of dominant mutations. The observation that only one mutated allele of the SERCA2 is sufficient to produce clinical symptoms suggests that proper “gene dosage” is necessary for maintaining Ca2+ homeostasis in cells.[12] This means that two wild type copies of ATP2A2 are needed for proper cell function, which provides a logical basis for dominant phenotypes arising from loss-of-function alleles. Most ATP2A2 mutations are haploinsufficiency mutations, which means that only having only one functional copy of the functional gene results in a reduced level of protein expression that is not sufficient for wild type function for making enough of the coded protein for the cell to function properly. However, there is significant variability in disease severity in how the mutations are expressed even within families that have the same mutation. It is currently unclear in the current research why a reduction in SERCA2 expression/activity causes clinical symptoms restricted to the epidermis. One hypothesis that some researchers have given is that other cell types express additional “back-up” Ca2+ pumps that can compensate for the reduced function or expression of the SERCA2 protein, while skin cells rely exclusively on the SERCA2 gene for calcium sequestration, meaning only they are affected by its reduction in expression.[13]
As mentioned above, some cases of DAR result from somatic mutations to ATP2A2 in epidermal stem cells. These cases are referred to as instances of “linear” Darier’s disease. Such individuals display phenotypic mosaicism, where the Darier’s phenotype only affects the subset of epidermal tissue arising from the mutated progenitor cell. Somatic mutations are not inherited by the offspring of such individuals.[16]
Diagnosis
Diagnosis of Darier disease is often made by the appearance of the skin, family history, or genetic testing for the mutation in the ATP2A2 gene. However, many individuals affected by this disorder are never diagnosed, due to the mildness of symptoms in most cases. Mild cases present clinically are minor rashes (without odor) that can become exacerbated by heat, humidity, stress, and sunlight. The symptoms of the disease are thought to be caused by an abnormality in the desmosome-keratin filament complex leading to a breakdown in cell adhesion.[13][9]
Darier's disease is an incommunicable disorder that is seen in males and females equally. Symptoms typically arise between the ages of 15 and 30. One study of 100 British individuals diagnosed with Darier's disease reported that affected individuals display elevated frequencies of neuropsychiatric conditions. There were high lifetime rates for mood disorders (50%), including depression (30%), bipolar disorder (4%), suicidal thoughts (31%), and suicide attempts (13%), suggesting a possible common genetic link.[17] Several case studies have suggested affected populations display elevated frequencies of learning disorders, but this has yet to be confirmed.
Treatment
Treatment of Darier disease depends on the severity of the presented clinical symptoms. In most minor cases, the disorder can be managed using sunscreen, moisturizing lotions, avoidance of non-breathable clothing, and excessive perspiration. In more severe cases of Darier's disease, affected individuals may display frequent relapse and remit patterns. In less severe cases, signs and symptoms may clear up completely through hygienic interventions. Most patients with Darier's disease live normal, healthy lives. Rapid resolution of rash symptoms can be complicated due to the increased vulnerability of affected skin surfaces by secondary bacterial or viral infections. Epidermal Staphylococcus aureus, human papillomavirus (HPV) and herpes simplex virus (HSV) infections have been reported. In these cases, topical and/or oral antibiotic/antiviral medications may need to be prescribed.[18]
Typical recommendations are:
- Application of antiseptics
- Soak in astringents
- Antibiotics
- Benzoyl peroxide[19]
- Topical diclofenac sodium[20][21]
If Darier's is more localized, common treatments include:
- Topical retinoids: used to help in the reduction of hyperkeratosis, retinoids work by causing the skin cells in the top layers to die and be shed off. The common retinoids used for this disorder are:
- Dermabrasion
- Removal of the top layer of skin to help smooth and stimulate new growth of the skin.[22]
- Electrosurgery
- Used to help stop bleeding and remove abnormal skin growths.
- Topical corticosteroids
If symptoms are severe, oral retinoids be prescribed and have been proven to be 90% effective. However, there can be many adverse side-effects associated with prolonged use.[23] Common oral retinoids are:
- Acitretin
- Isotretinoin
- Cyclosporine
Some patients are able to prevent flares with use of topical sunscreens and oral vitamin C.[24]
Further information on and advocacy work for Darier's disease are provided by the FIRST Skin Foundation.[25]
Epidemiology
Worldwide prevalence is estimated as between 1:30,000 and 1:100,000. Case studies have shown estimated prevalence by country to be 3.8:100,000 in Slovenia,[26] 1:36,000 in north-east England,[27] 1:30,000 in Scotland,[28] and 1:100,000 in Denmark.[29]
History
Darier’s disease was first described by the dermatologist Ferdinand-Jean Darier in the French dermatological journal Annales de dermatologie et de syphilographie. Darier was a well-regarded dermatologist of the time who was the head of the medical department at the Hôpital Saint-Louis. Darier was an early proponent of histopathology, or the examination of samples of diseased flesh under a microscope to determine the cause of illnesses. Using this technique, he was able to uncover the origins of Darier’s disease and a host of others that also bear his name.[30]
James Clark White, a dermatologist at Harvard Medical School, independently characterized and published his observations on this dermatological disorder in the same year as Darier (1889), which is why Darier's disease is also referred to as Darier-White disease.
See also
References
- 1 2 Rapini, Ronald P.; Bolognia, Jean L.; Jorizzo, Joseph L. (2007). Dermatology: 2-Volume Set. St. Louis, MO: Mosby. ISBN 978-1-4160-2999-1.
- 1 2 Crissey, John Thorne; Parish, Lawrence C.; Holubar, Karl (2013). "Late nineteenth century French dermatology". Historical Atlas of Dermatology and Dermatologists. CRC Press. p. 75. ISBN 978-1-84184-864-8. Archived from the original on 2023-06-30. Retrieved 2023-05-20.
- ↑ "Darier disease - About the Disease - Genetic and Rare Diseases Information Center". rarediseases.info.nih.gov. National Center for Advancing Translational Sciences. Archived from the original on 24 September 2020. Retrieved 20 May 2023.
- 1 2 James, William D.; Elston, Dirk; Treat, James R.; Rosenbach, Misha A.; Neuhaus, Isaac (2020). "27. Genodermatoses and congenital anomalies". Andrews' Diseases of the Skin: Clinical Dermatology (13th ed.). Elsevier. p. 572. ISBN 978-0-323-54753-6. Archived from the original on 2023-03-14. Retrieved 2023-05-20.
- ↑ "Darier disease". dermnetnz.org. Dermnetnz. Archived from the original on 30 June 2023. Retrieved 20 May 2023.
- ↑ National Organization for Rare Disorders (2002). NORD Guide to Rare Disorders. Lippincott Williams & Wilkins. ISBN 0-7817-3063-5.
- ↑ Sehgal, V. N.; Srivastava, G. (2005). "Darier's (Darier-White) disease/keratosis follicularis". International Journal of Dermatology. 44 (3): 184–192. doi:10.1111/j.1365-4632.2004.02408.x. PMID 15807723. S2CID 45303870.
- ↑ "Darier disease | Genetic and Rare Diseases Information Center (GARD) – an NCATS Program". rarediseases.info.nih.gov. Archived from the original on 2020-09-24. Retrieved 2020-05-08.
- 1 2 3 4 "Darier disease NZ". DermNet. Archived from the original on 2020-08-03. Retrieved 2020-05-07.
- ↑ "Acrokeratosis Verruciformis of Hopf: Background, Pathophysiology, Etiology". 2020-03-26. Archived from the original on 2020-11-26. Retrieved 2020-05-08.
{{cite journal}}: Cite journal requires|journal=(help) - ↑ Monk, Sarah; Sakuntabhai, Anavaj; Carter, Simon A.; Bryce, Steven D.; Cox, Roger; Harrington, Louise; Levy, Elaine; Ruiz-Perez, Victor L.; Katsantoni, Eleni; Kodvawala, Ahmer; Munro, Colin S. (April 1998). "Refined Genetic Mapping of the Darier Locus to a <1-cM Region of Chromosome 12q24.1, and Construction of a Complete, High-Resolution P1 Artificial Chromosome/Bacterial Artificial Chromosome Contig of the Critical Region". The American Journal of Human Genetics. 62 (4): 890–903. doi:10.1086/301794. ISSN 0002-9297. PMC 1377034. PMID 9529352.
- 1 2 Foggia, Lucie; Hovnanian, Alain (2004). "Calcium pump disorders of the skin". American Journal of Medical Genetics Part C: Seminars in Medical Genetics (in français). 131C (1): 20–31. doi:10.1002/ajmg.c.30031. ISSN 1552-4876. PMID 15468148. S2CID 675895.
- 1 2 3 Reference, Genetics Home. "Darier disease". Genetics Home Reference. Archived from the original on 2020-06-26. Retrieved 2020-05-08.
- ↑ Sakuntabhai, Anavaj; Ruiz-Perez, Victor; Carter, Simon; Jacobsen, Nick; Burge, Susan; Monk, Sarah; Smith, Melanie; Munro, Colin S.; O'Donovan, Michael; Craddock, Nick; Kucherlapati, Raju (March 1999). "Mutations in ATP2A2, encoding a Ca 2+ pump, cause Darier disease". Nature Genetics. 21 (3): 271–277. doi:10.1038/6784. ISSN 1546-1718. PMID 10080178. S2CID 38684482. Archived from the original on 2021-03-08. Retrieved 2020-05-08.
- ↑ Ruiz-Perez, Victor L.; Carter, Simon A.; Healy, Eugene; Todd, Carole; Rees, Jonathan L.; Steijlen, Peter M.; Carmichael, Andrew J.; Lewis, Helen M.; Hohl, D.; Itin, Peter; Vahlquist, Anders (1999-09-01). "ATP2A2 Mutations in Darier's Disease: Variant Cutaneous Phenotypes Are Associated with Missense Mutations, But Neuropsychiatry Features Are Independent of Mutation Class". Human Molecular Genetics. 8 (9): 1621–1630. doi:10.1093/hmg/8.9.1621. ISSN 0964-6906. PMID 10441324. Archived from the original on 2019-06-10. Retrieved 2020-05-08.
- ↑ Sakuntabhai, Anavaj; Dhitavat, Jittima; Hovnanian, Alain; Burge, Susan (December 2000). "Mosaicism for ATP2A2 Mutations Causes Segmental Darier's Disease". Journal of Investigative Dermatology. 115 (6): 1144–1147. doi:10.1046/j.1523-1747.2000.00182.x. ISSN 0022-202X. PMID 11121153.
- ↑ Gordon-Smith K, Jones LA, Burge SM, Munro CS, Tavadia S, Craddock N (September 2010). "The neuropsychiatric phenotype in Darier disease". Br. J. Dermatol. 163 (3): 515–22. doi:10.1111/j.1365-2133.2010.09834.x. PMID 20456342. S2CID 22856369.
- ↑ Hohl, D. Hand, J. Darier disease. (2017) Corona, R. (Ed) Uptodate.
- ↑ Lippincott's Illustrated Reviews: Biochemistry (Champe, Harvey & Ferrier, ISBN 0-7817-2265-9, 3rd ed., Lippincott Williams & Wilkins 2005)
- ↑ Kamijo M, Nishiyama C, Takagi A, Nakano N, Hara M, Ikeda S, Okumura K, Ogawa H (May 2012). "Cyclooxygenase-2 inhibition restores ultraviolet B-induced downregulation of ATP2A2/SERCA2 in keratinocytes: possible therapeutic approach of cyclooxygenase-2 inhibition for treatment of Darier disease". Br. J. Dermatol. 166 (5): 1017–22. doi:10.1111/j.1365-2133.2011.10789.x. PMID 22413864. S2CID 42918432.
- ↑ Millán-Parrilla F, Rodrigo-Nicolás B, Molés-Poveda P, Armengot-Carbó M, Quecedo-Estébanez E, Gimeno-Carpio E (April 2014). "Improvement of Darier disease with diclofenac sodium 3% gel". J. Am. Acad. Dermatol. 70 (4): e89–e90. doi:10.1016/j.jaad.2013.11.033. PMID 24629373.
- ↑ "Dermabrasion: MedlinePlus Medical Encyclopedia". medlineplus.gov. Archived from the original on 2020-07-03. Retrieved 2020-05-08.
- ↑ "How do retinol creams work, anyway?". Sundaily. Archived from the original on 2020-09-28. Retrieved 2020-05-08.
- ↑ Andrew's Diseases of the Skin (James, Berger, Elston, 10th ed., Saunders Elsevier, 2006)
- ↑ "FIRST Skin Foundation". Archived from the original on 2019-05-30. Retrieved 2020-05-08.
- ↑ Godic A, Miljkovic J, Kansky A, Vidmar G (June 2005). "Epidemiology of Darier's Disease in Slovenia". Acta Dermatovenerol Alp Pannonica Adriat. 14 (2): 43–8. PMID 16001099.
- ↑ Munro CS (August 1992). "The phenotype of Darier's disease: penetrance and expressivity in adults and children". Br. J. Dermatol. 127 (2): 126–30. doi:10.1111/j.1365-2133.1992.tb08044.x. PMID 1390140. S2CID 2911858.
- ↑ Tavadia S, Mortimer E, Munro CS (January 2002). "Genetic epidemiology of Darier's disease: a population study in the west of Scotland". Br. J. Dermatol. 146 (1): 107–9. doi:10.1046/j.1365-2133.2002.04559.x. PMID 11841374. S2CID 42621572.
- ↑ Burge SM, Wilkinson JD (July 1992). "Darier-White disease: a review of the clinical features in 163 patients". J. Am. Acad. Dermatol. 27 (1): 40–50. doi:10.1016/0190-9622(92)70154-8. PMID 1619075.
- ↑ Cadogan, Dr Mike (2019-03-01). "Ferdinand-Jean Darier • LITFL". Life in the Fast Lane • LITFL • Medical Blog. Archived from the original on 2020-11-26. Retrieved 2020-05-08.
Cardoso CL, Freitas P, Taveira LAA, Consolaro A. Darier disease:
case report with oral manifestations. Med Oral Patol Oral Cir Bucal 2006;11:E404-6
| Classification | |
|---|---|
| External resources |
.jpg.webp)
.jpg.webp)

