Tolperisone
Tolperisone (trade name Mydocalm among others) is a centrally acting skeletal muscle relaxant used for the treatment of increased muscle tone associated with neurological diseases. It has been used since the 1960s.
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Mydocalm and others |
| AHFS/Drugs.com | International Drug Names |
| Routes of administration | Oral, parenteral |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Metabolism | Liver, kidney |
| Elimination half-life | 1st phase: 2 hrs 2nd phase: 12 hrs |
| Excretion | Renal |
| Identifiers | |
IUPAC name
| |
| CAS Number | |
| PubChem CID | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.010.889 |
| Chemical and physical data | |
| Formula | C16H23NO |
| Molar mass | 245.366 g·mol−1 |
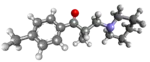
| 3D model (JSmol) | |
SMILES
| |
InChI
| |
| | |
Medical uses
Tolperisone is indicated for use in the treatment of pathologically increased tone of the skeletal muscle caused by neurological diseases (damage of the pyramidal tract, multiple sclerosis, myelopathy, encephalomyelitis) and of spastic paralysis and other encephalopathies manifested with muscular dystonia.[1][2]
Other possible uses include:
- Spondylosis
- Spondylarthrosis
- Cervical and lumbar syndromes
- Arthrosis of the large joints
- Obliterating atherosclerosis of the extremity vessels
- Diabetic angiopathy
- Thromboangiitis obliterans
- Raynaud's syndrome
Contraindications and cautions
Manufacturers report that tolperisone should not be used in patients with myasthenia gravis. Only limited data are available regarding the safety in children, youths, during pregnancy and breastfeeding. It is not known whether tolperisone is excreted into mother's milk.[1][2]
In 2012, following concerns on the safety and efficacy, an "article 31 referral"[3] was triggered at the European Medicines Agency. The European Medicines Agency has recommended restricting the use of tolperisone. After review and a subsequent re-examination in 2012, the Agency concluded the safety and adverse reaction risks of this drug outweigh the benefits, and that there is weak support for its efficacy, in all but one indication (muscle stiffness or spasticity after stroke), and specifically, due to the prevalence of hypersensitivity symptoms such as flushing, rash, severe skin itchiness (with raised lumps), wheezing, difficulty breathing, and swallowing, fast heartbeat and fast decrease in blood pressure (basically anaphylaxis), their recommendations included ceasing advertising in Europe and ceasing injections, updating patient information leaflets, changing to another medicine for existing users, and for prescribers to only use it stroke patients when administered by mouth, not injection.[4]
Side effects
Adverse effects occur in fewer than 1% of patients and include muscle weakness, headache, arterial hypotension, nausea, vomiting, dyspepsia, and dry mouth. All effects are reversible.[1][2] Allergic reactions occur in fewer than 0.1% of patient and include skin rash, hives, Quincke's edema, and in some cases anaphylactic shock.[1][5][6][7]
Overdose
Excitability has been noted after ingestion of high doses by children.[1] In suicide studies of three isolated cases, it is believed that ingestion of tolperisone was the cause of death.[8]
Interactions
Tolperisone does not have a significant potential for interactions with other pharmaceutical drugs. It cannot be excluded that combination with other centrally acting muscle relaxants, benzodiazepines or nonsteroidal anti-inflammatory drugs (NSAIDs) may make a dose reduction necessary in some patients.[1][2]
Pharmacology
Mechanism of action
Tolperisone is a centrally acting muscle relaxant that acts at the reticular formation in the brain stem[1] by blocking voltage-gated sodium and calcium channels.[9][10]
Pharmacokinetics
Tolperisone is absorbed nearly completely from the gut and reaches its peak blood plasma concentration after 1.5 hours. It is extensively metabolised in the liver and kidneys. The substance is excreted via the kidneys in two phases; the first with a half-life of two hours, and the second with a half-life of 12 hours.[1]
Chemistry
Tolperisone a piperidine derivative.
Society and culture
Brand names
Brand names include Mydocalm, Biocalm, Mydeton, Miderizone, Mydoflex, Myolax, Myoxan and Viveo.
See also
- Chemically and mechanistically related drugs: eperisone, inaperisone, lanperisone, silperisone
References
- Jasek, W, ed. (2007). Austria-Codex (in German) (62nd ed.). Vienna: Österreichischer Apothekerverlag. pp. 5510–1. ISBN 978-3-85200-181-4.
- "Midocalm". Romania: InfoMedic.
- https://www.ema.europa.eu/en/human-regulatory/post-authorisation/referral-procedures
- https://www.ema.europa.eu/en/medicines/human/referrals/tolperisone
- Ribi C, Vermeulen C, Hauser C (2003). "Anaphylactic reactions to tolperisone (Mydocalm)". Swiss Medical Weekly. 133 (25–26): 369–371. PMID 12947534.
- Kwaśniewski A, Korbuszewska-Gontarz B, Mika S (2003). "[Mydocalm causing anaphylaxis]". Pneumonologia I Alergologia Polska (in Polish). 71 (5–6): 250–2. PMID 14587432.
- Glück J, Rymarczyk B, Rogala B (2011). "An immediate hypersensitivity reaction caused by tolperisone hydrochloride". J Investig Allergol Clin Immunol. 21 (5): 411–2. PMID 21905508.
- Sporkert, F.; Brunel, C.; Augsburger, M. P.; Mangin, P. (2012). "Fatal tolperisone poisoning: Autopsy and toxicology findings in three suicide cases". Forensic Science International. 215 (1): 101–104. doi:10.1016/j.forsciint.2011.05.025. PMID 21683537.
- Kocsis P, Farkas S, Fodor L, Bielik N, Thán M, Kolok S, Gere A, Csejtei M, Tarnawa I (2005). "Tolperisone-type drugs inhibit spinal reflexes via blockade of voltage-gated sodium and calcium channels". Journal of Pharmacology and Experimental Therapeutics. 315 (3): 1237–1246. doi:10.1124/jpet.105.089805. PMID 16126840. S2CID 13020517.
- Hofer D, Lohberger B, Steinecker B, Schmidt K, Quasthoff S, Schreibmayer W (2006). "A comparative study of the action of tolperisone on seven different voltage dependent sodium channel isoforms". European Journal of Pharmacology. 538 (1–3): 5–14. doi:10.1016/j.ejphar.2006.03.034. PMID 16650844.