Cyproheptadine
Cyproheptadine, sold under the brand name Periactin among others, is a first-generation antihistamine with additional anticholinergic, antiserotonergic, and local anesthetic properties.
 | |
 | |
| Clinical data | |
|---|---|
| Pronunciation | (/ˌsaɪproʊˈhɛptədiːn/[1] |
| Trade names | Periactin, others |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a682541 |
| License data | |
| Pregnancy category |
|
| Routes of administration | Oral |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Protein binding | 96 to 99% |
| Metabolism | Hepatic,[2][3] mostly CYP3A4 mediated. |
| Elimination half-life | 8.6 hours[4] |
| Excretion | Faecal (2–20%; of which, 34% as unchanged drug) and renal (40%; none as unchanged drug)[2][3] |
| Identifiers | |
IUPAC name
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.004.482 |
| Chemical and physical data | |
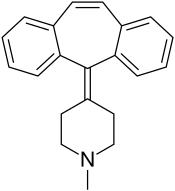
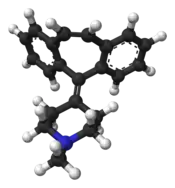
| Formula | C21H21N |
| Molar mass | 287.406 g·mol−1 |
| 3D model (JSmol) | |
SMILES
| |
InChI
| |
| (verify) | |
It was patented in 1959 and came into medical use in 1961.[5]
Medical uses

Cyproheptadine is used to treat allergic reactions (specifically hay fever).[6] The evidence for its use for this purpose indicates its effectiveness but second generation antihistamines such as ketotifen and loratadine have shown equal results with fewer side effects.[7]
It is also used as a preventive treatment against migraine. In a 2013 study the frequency of migraine was dramatically reduced in patients within 7 to 10 days after starting treatment. The average frequency of migraine attacks in these patients before administration was 8.7 times per month, this was decreased to 3.1 times per month at 3 months after the start of treatment.[7][8] This use is on the label in the UK and some other countries.
It is also used off-label in the treatment of cyclical vomiting syndrome in infants; the only evidence for this use comes from retrospective studies.[9]
Cyproheptadine is sometimes used off-label to improve akathisia in people on antipsychotic medications.[10]
It is used off-label to treat various dermatological conditions, including psychogenic itch[11] drug-induced hyperhidrosis (excessive sweating),[12] and prevention of blister formation for some people with epidermolysis bullosa simplex.[13]
One of the effects of the drug is increased appetite and weight gain, which has led to its use (off-label in the USA) for this purpose in children who are wasting as well as people with cystic fibrosis.[14][15][16][17]
It is also used off-label in the management of moderate to severe cases of serotonin syndrome, a complex of symptoms associated with the use of serotonergic drugs, such as selective serotonin reuptake inhibitors (and monoamine oxidase inhibitors), and in cases of high levels of serotonin in the blood resulting from a serotonin-producing carcinoid tumor.[18][19]
Cyproheptadine has sedative effects and can be used to treat insomnia similarly to other centrally-acting antihistamines.[20][21][22][23] The recommended dose for this use is 4 to 8 mg.[21]
Adverse effects
Adverse effects include:[2][3]
- Sedation and sleepiness (often transient)
- Dizziness
- Disturbed coordination
- Confusion
- Restlessness
- Excitation
- Nervousness
- Tremor
- Irritability
- Insomnia
- Paresthesias
- Neuritis
- Convulsions
- Euphoria
- Hallucinations
- Hysteria
- Faintness
- Allergic manifestation of rash and edema
- Diaphoresis
- Urticaria
- Photosensitivity
- Acute labyrinthitis
- Diplopia (seeing double)
- Vertigo
- Tinnitus
- Hypotension (low blood pressure)
- Palpitation
- Extrasystoles
- Anaphylactic shock
- Hemolytic anemia
- Blood dyscrasias such as leukopenia, agranulocytosis and thrombocytopenia
- Cholestasis
- Hepatic (liver) side effects such as:
- Hepatitis
- Jaundice
- Liver failure[24]
- Hepatic function abnormality
- Epigastric distress
- Anorexia
- Nausea
- Vomiting
- Diarrhea
- Anticholinergic side effects such as:
- Blurred vision
- Constipation
- Xerostomia (dry mouth)
- Tachycardia (high heart rate)
- Urinary retention
- Difficulty passing urine
- Nasal congestion
- Nasal or throat dryness
- Urinary frequency
- Early menses
- Thickening of bronchial secretions
- Tightness of chest and wheezing
- Fatigue
- Chills
- Headache
- Increased appetite
- Weight gain
Overdose
Gastric decontamination measures such as activated charcoal are sometimes recommended in cases of overdose. The symptoms are usually indicative of CNS depression (or conversely CNS stimulation in some) and excess anticholinergic side effects. The LD50 in mice is 123 mg/kg and 295 mg/kg in rats.[2][3]
Pharmacology
Pharmacodynamics
| Site | Ki (nM)[lower-alpha 1] | Action[lower-alpha 2] | Species | Ref. |
|---|---|---|---|---|
| H1 | 0.06 | ↓ | Human | |
| H2 | ND | ND | ||
| H3 | >10,000 | Human | ||
| H4 | 202 | Human | ||
| M1 | 12 | ↓ | Human | |
| M2 | 7 | ↓ | Human | |
| M3 | 12 | ↓ | Human | |
| M4 | 8 | ↓ | Human | |
| M5 | 11.8 | ↓ | Human | |
| 5-HT1A | 59 | ↓ | Human | |
| 5-HT2A | 1.67 | ↓ | Human | |
| 5-HT2B | 1.54 | ↓ | Human | |
| 5-HT2C | 2.23 | ↓ | Human | |
| 5-HT3 | 228 | Mouse | ||
| 5-HT6 | 142 | Human | ||
| 5-HT7 | 123 | Human | ||
| D1 | 117 | Human | ||
| D2 | 112 | ↓ | Human | |
| D3 | 8 | Human | ||
| SERT | 4,100 | Rat | ||
| NET | 290 | Rat | ||
| DAT | ND | ND | ||
| ||||
Cyproheptadine is a very potent antihistamine or inverse agonist of the H1 receptor. At higher concentrations, it also has anticholinergic, antiserotonergic, and antidopaminergic activities. Of the serotonin receptors, it is an especially potent antagonist of the 5-HT2 receptors. This is thought to underlie its effectiveness in the treatment of serotonin syndrome.[26] However, it is possible that blockade of 5-HT1 receptors may also contribute to its effectiveness in serotonin syndrome.[27] Cyproheptadine has been reported to block 85% of 5-HT2 receptors in the human brain at a dose of 4 mg three times per day (12 mg/day total) and to block 95% of 5-HT2 receptors in the human brain at a dose of 6 mg three times per day (18 mg/day total) as measured with positron emission tomography (PET).[28] The dose of cyproheptadine recommended to ensure blockade of the 5-HT2 receptors for serotonin syndrome is 20 to 30 mg.[26] Besides its activity at neurotransmitter targets, cyproheptadine has been reported to possess weak antiandrogenic activity.[29]
Pharmacokinetics
Cyproheptadine is well-absorbed following oral ingestion, with peak plasma levels occurring after 1 to 3 hours.[30] Its terminal half-life when taken orally is approximately 8 hours.[4]
Chemistry
Cyproheptadine is a tricyclic benzocycloheptene and is closely related to pizotifen and ketotifen as well as to tricyclic antidepressants.
Research
Cyproheptadine was studied in one small trial as an adjunct in people with schizophrenia whose condition was stable and were on other medication; while attention and verbal fluency appeared to be improved, the study was too small to draw generalizations from.[31] It has also been studied as an adjuvant in two other trials in people with schizophrenia, around fifty people overall, and did not appear to have an effect.[32]
There have been some trials to see if cyproheptadine could reduce sexual dysfunction caused by SSRI and antipsychotic medications.[33]
Cyproheptadine has been studied for the treatment of posttraumatic stress disorder.[32]
Veterinary use
Cyproheptadine is used in cats as an appetite stimulant[34][35]: 1371 and as an adjunct in the treatment of asthma.[36] Possible adverse effects include excitement and aggressive behavior.[37] The elimination half-life of cyproheptadine in cats is 12 hours.[36]
Cyproheptadine is a second line treatment for pituitary pars intermedia dysfunction in horses.[38][39]
References
- "Cyproheptadine". Dictionary.com Unabridged (Online). n.d.
- "CYPROHEPTADINE HYDROCHLORIDE tablet [Boscogen, Inc.]" (PDF). DailyMed. Boscogen, Inc. November 2010. Retrieved 26 October 2013.
- "PRODUCT INFORMATION PERIACTIN® (cyproheptadine hydrochloride)" (PDF). Aspen Pharmacare Australia. Aspen Pharmacare Australia Pty Ltd. 17 November 2011. Archived from the original (PDF) on 29 October 2013. Retrieved 26 October 2013.
- Gunja N, Collins M, Graudins A (2004). "A comparison of the pharmacokinetics of oral and sublingual cyproheptadine". Journal of Toxicology. Clinical Toxicology. 42 (1): 79–83. doi:10.1081/clt-120028749. PMID 15083941. S2CID 20196551.
- Fischer, Jnos; Ganellin, C. Robin (2006). Analogue-based Drug Discovery. John Wiley & Sons. p. 547. ISBN 9783527607495.
- MedlinePlus Drug Information: Cyproheptadine
- De Bruyne, P; Christiaens, T; Boussery, K; Mehuys, E; Van Winckel, M (January 2017). "Are antihistamines effective in children? A review of the evidence". Archives of Disease in Childhood. 102 (1): 56–60. doi:10.1136/archdischild-2015-310416. PMID 27335428. S2CID 21185048.
- Saito, Y; Yamanaka, G; Shimomura, H; Shiraishi, K; Nakazawa, T; Kato, F; Shimizu-Motohashi, Y; Sasaki, M; Maegaki, Y (May 2017). "Reconsideration of the diagnosis and treatment of childhood migraine: A practical review of clinical experiences". Brain & Development. 39 (5): 386–394. doi:10.1016/j.braindev.2016.11.011. PMID 27993427. S2CID 34703034.
- Salvatore, S; Barberi, S; Borrelli, O; Castellazzi, A; Di Mauro, D; Di Mauro, G; Doria, M; Francavilla, R; Landi, M; Martelli, A; Miniello, VL; Simeone, G; Verduci, E; Verga, C; Zanetti, MA; Staiano, A; SIPPS Working Group on, FGIDs. (16 July 2016). "Pharmacological interventions on early functional gastrointestinal disorders". Italian Journal of Pediatrics. 42 (1): 68. doi:10.1186/s13052-016-0272-5. PMC 4947301. PMID 27423188.
- Taylor, David M.; Paton, Carol; Kapur, Shitij (2015). The Maudsley Prescribing Guidelines in Psychiatry. John Wiley & Sons. p. 85. ISBN 978-1-118-75457-3.
- Szepietowski, Jacek C.; Reszke, Radomir (2016). "Psychogenic Itch Management". Itch - Management in Clinical Practice. Current Problems in Dermatology. Vol. 50. pp. 124–132. doi:10.1159/000446055. ISBN 978-3-318-05888-8. PMID 27578081.
- Ashton AK, Weinstein WL (May 2002). "Cyproheptadine for drug-induced sweating". American Journal of Psychiatry. 159 (5): 874–5. doi:10.1176/appi.ajp.159.5.874-a. PMID 11986151.
- So, Jodi Y.; Teng, Joyce (1993). "Epidermolysis Bullosa Simplex". GeneReviews®. University of Washington, Seattle. PMID 20301543.
- Ciproheptadina, estimulante del apetito (Cyproheptadine, appetite stimulant)
- "Bioplex NF". Archived from the original on 2018-04-18. Retrieved 2018-04-18.
- Harrison ME, Norris ML, Robinson A, Spettigue W, Morrissey M, Isserlin L (2019). "Use of cyproheptadine to stimulate appetite and body weight gain: A systematic review". Appetite. 137: 62–72. doi:10.1016/j.appet.2019.02.012. PMID 30825493. S2CID 72333631.
{{cite journal}}: CS1 maint: uses authors parameter (link) - Kim SY, Yun JM, Lee JW, Cho YG, Cho KH, Park YG, Cho B (September 2021). "Efficacy and Tolerability of Cyproheptadine in Poor Appetite: A Multicenter, Randomized, Double-blind, Placebo-controlled Study". Clin Ther. 43 (10): 1757–1772. doi:10.1016/j.clinthera.2021.08.001. PMID 34509304. S2CID 237493456.
- Rossi, S, ed. (2013). Australian Medicines Handbook (2013 ed.). Adelaide: The Australian Medicines Handbook Unit Trust. ISBN 978-0-9805790-9-3.
- Iqbal, MM; Basil, MJ; Kaplan, J; Iqbal, MT (November 2012). "Overview of serotonin syndrome". Annals of Clinical Psychiatry. 24 (4): 310–8. PMID 23145389.
- Badr B, Naguy A (February 2021). "Cyproheptadine: a psychopharmacological treasure trove?". CNS Spectr. 27 (5): 533–535. doi:10.1017/S1092852921000250. PMID 33632345.
- Ekambaram V, Owens J (January 2021). "Medications Used for Pediatric Insomnia". Child Adolesc Psychiatr Clin N Am. 30 (1): 85–99. doi:10.1016/j.chc.2020.09.001. PMID 33223070. S2CID 227131545.
- Rombaut, Niekol Elvire Irma (1995). Antihistamines and Sedation: Methods and Measures (Thesis). OCLC 59660401. ProQuest 301570569.
- Wanderer AA, St Pierre JP, Ellis EF (October 1977). "Primary acquired cold urticaria. Double-blind comparative study of treatment with cyproheptadine, chlorpheniramine, and placebo". Arch Dermatol. 113 (10): 1375–7. doi:10.1001/archderm.113.10.1375. PMID 334082.
- Chertoff, Jason (8 July 2014). "Cyproheptadine-Induced Acute Liver Failure". ACG Case Reports Journal. 1 (4): 212–213. doi:10.14309/crj.2014.56. PMC 4286888. PMID 25580444.
- Roth, BL; Driscol, J. "PDSP Ki Database". Psychoactive Drug Screening Program (PDSP). University of North Carolina at Chapel Hill and the United States National Institute of Mental Health. Retrieved 14 August 2017.
- Gillman PK (1999). "The serotonin syndrome and its treatment". J Psychopharmacol. 13 (1): 100–9. doi:10.1177/026988119901300111. PMID 10221364. S2CID 17640246.
- Sporer KA (August 1995). "The serotonin syndrome. Implicated drugs, pathophysiology and management". Drug Saf. 13 (2): 94–104. doi:10.2165/00002018-199513020-00004. PMID 7576268. S2CID 19809259.
- Kapur S, Zipursky RB, Jones C, Wilson AA, DaSilva JD, Houle S (June 1997). "Cyproheptadine: a potent in vivo serotonin antagonist". Am J Psychiatry. 154 (6): 884a–884. doi:10.1176/ajp.154.6.884a. PMID 9167527.
- Pucci E, Petraglia F (December 1997). "Treatment of androgen excess in females: yesterday, today and tomorrow". Gynecol. Endocrinol. 11 (6): 411–33. doi:10.3109/09513599709152569. PMID 9476091.
- Lindsay Murray; Frank Daly; David McCoubrie; Mike Cadogan (15 January 2011). Toxicology Handbook. Elsevier Australia. p. 388. ISBN 978-0-7295-3939-5. Retrieved 27 November 2011.
- Buoli, M; Altamura, AC (March 2015). "May non-antipsychotic drugs improve cognition of schizophrenia patients?". Pharmacopsychiatry. 48 (2): 41–50. doi:10.1055/s-0034-1396801. PMID 25584772.
- Dabaghzadeh, F; Khalili, H; Ghaeli, P; Dashti-Khavidaki, S (December 2012). "Potential benefits of cyproheptadine in HIV-positive patients under treatment with antiretroviral drugs including efavirenz". Expert Opinion on Pharmacotherapy. 13 (18): 2613–24. doi:10.1517/14656566.2012.742887. PMID 23140169. S2CID 25769557.
- Nunes, LV; Moreira, HC; Razzouk, D; Nunes, SO; Mari Jde, J (2012). "Strategies for the treatment of antipsychotic-induced sexual dysfunction and/or hyperprolactinemia among patients of the schizophrenia spectrum: a review". Journal of Sex & Marital Therapy. 38 (3): 281–301. doi:10.1080/0092623X.2011.606883. PMID 22533871. S2CID 23406005.
- Agnew, W; Korman, R (September 2014). "Pharmacological appetite stimulation: rational choices in the inappetent cat". Journal of Feline Medicine and Surgery. 16 (9): 749–56. doi:10.1177/1098612X14545273. PMID 25146662. S2CID 37126352.
- Gupta, Ramesh C., ed. (2012). Veterinary Toxicology : Basic and Clinical Principles (2 ed.). Amsterdam Boston: Academic Press. pp. xii+1438. ISBN 978-0-12-385926-6. OCLC 794491298.
- Dowling PM (February 8, 2005). "Systemic Therapy of Airway Disease: Cyproheptadine". In Kahn CM, Line S, Aiello SE (eds.). The Merck Veterinary Manual (9th ed.). John Wiley & Sons. ISBN 978-0-911910-50-6. Retrieved on October 26, 2008.
- Dowling PM (February 8, 2005). "Drugs Affecting Appetite". In Kahn CM, Line S, Aiello SE (eds.). The Merck Veterinary Manual (9th ed.). John Wiley & Sons. ISBN 978-0-911910-50-6. Retrieved on October 26, 2008.
- Durham, AE (April 2017). "Therapeutics for Equine Endocrine Disorders". The Veterinary Clinics of North America. Equine Practice. 33 (1): 127–139. doi:10.1016/j.cveq.2016.11.003. PMID 28190613.
- Merck Vet Manual. "Hirsutism Associated with Adenomas of the Pars Intermedia". Retrieved April 24, 2011.